[box type=”bio”] What to Learn from this Article?[/box]
Evaluation and management of Peroneus Tendinopathy.
Surgical treatment using inverted sutures which does not interfere with the gliding of tendon in groove.
Case Report | Volume 5 | Issue 1 | JOCR Jan-March 2015 | Page 34-36 | Mukesh Tiwari, Varun Singh, Rakesh Bhargava. DOI: 10.13107/jocr.2250-0685.250
Authors: Mukesh Tiwari[1], Varun Singh[1], Rakesh Bhargava[1]
[1] Department of Orthopedics, NIMS medical college, Jaipur. India.
Address of Correspondence:
Dr. Mukesh Tiwari, 21/10,Madhyam Marg, Mansarover, Jaipur – 302020, India. Email: wakeuptum@gmail.com
Abstract
Introduction: Peroneus brevis tendinitis with its attritional longitudinal split rupture without any subluxation from peroneal groove and associated enlarged peroneal tubercle is un common presentation.
Case Report: A 40 year old female presented with moderate swelling and tenderness over the lateral and dorso-lateral aspect of left ankle with history of old trauma to ankle with swelling , persistant pain and difficulty in walking. On physical examination during passive eversion and inversion the excursion of the peroneal tendons was painful. Most tender point was just posterior to the tip of the fibula. During surgery we found the intact superior peroneal ligament with both peroneal tendons placed at normal site without subluxation, tendon sheath was inflamed and swollen, on further dissection we could see the attrition of inner surface of the peroneus brevis and a 2 cm longitudinal split tear of the same.
Conclusion: Although rare but peroneus brevis tendon attrition and tear can occur without subluxation from peronal groove. Refractory ankle pain on lateral aspect presenting with on and off swelling should arise suspicion of peroneal tendon tear. Correct diagnosis and proper surgical repair can produce excellent results.
Keywords: Peroneal brevis tendinitis,subluxation,lateral ankle pain.
Introduction
There are only a few reports of peroneal tendon tears with hypertrophied peroneal tubercle, which are thought to be uncommon 1. A longitudinal tear of the peroneal tendon is thought to be the result of repetitive peroneal subluxation [2,3,4]. However, this report documents a case of longitudinal split of the peroneus brevis tendon that had no peroneal tendon subluxation. Subluxation of the peroneal tendons was not identified surgically in this case. Bassett et al reported peroneal tendon tears that did not result in instability of the ankle and there was no subluxation of the tendon when examined clinically. We report here one such uncommon case & technique of treatment for peroneus brevis tendon tear without subluxation of the tendons.
Case report
A 40 year old female patient presented with pain and moderate amount of swelling over lateral aspect of ankle since 2 months. Pain and swelling used to increase on prolonged walking and relieve by rest. She had a past history of twisting injury to the ankle couple of months back. She took conservative treatment as taping and steroid injections for last 2 months to alleviate pain and swelling but they were ineffective. On physical examination retrofibular tenderness on dorsiflexion eversion stress was found. Mild hind foot varus was present There was no evidence of peroneal tendon subluxation. Plain and plantarflexion inversion stress view radiographs were normal.
Diagnosis: Histologically, specimen of hypertrophied soft tissue which surrounded the peroneal tendon & extra slip of peroneal tendon fibers examined microscopically reveal degeneration of the tendon fibers. There were areas of fibroblastic proliferation present, with lymphocytes infiltrated into the tendon [5].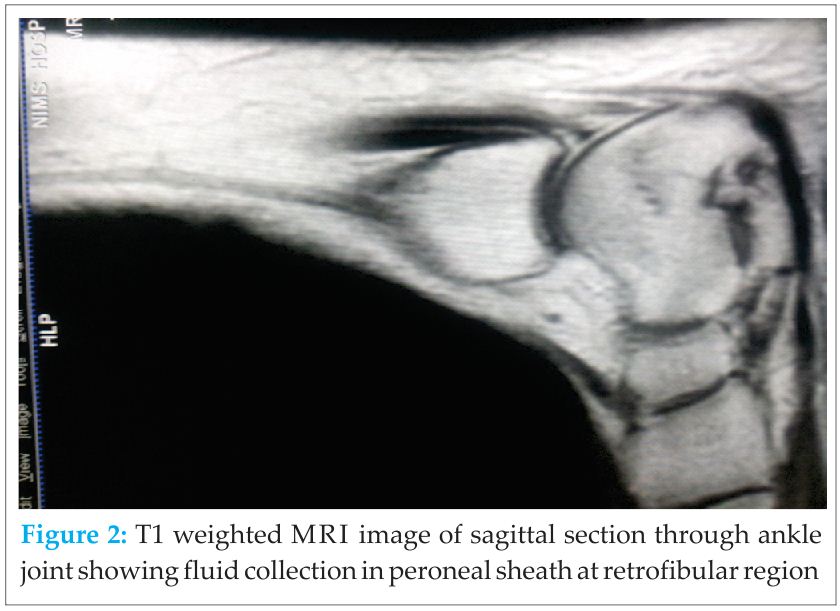
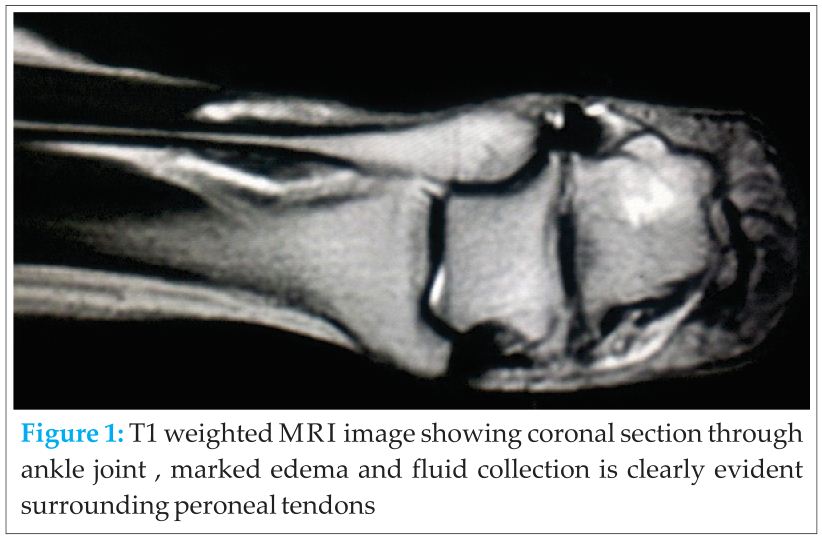
MRI showed significant fluid collection along the peroneal tendon sheath, however split could not be appreciated over the MRI [6,7]. A classification of peroneus brevis tendon splits has been proposed by Sobel [8], (Table 1).
Table 1 Grading Scale For Peroneus Brevis Splits: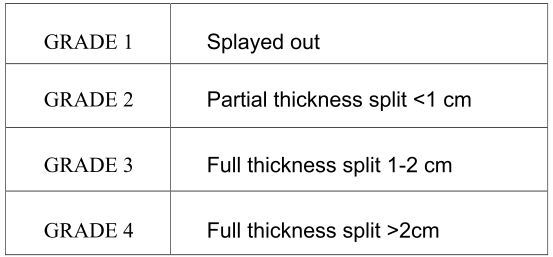
Surgical technique: Surgical treatment of peroneal tendinopathy is indicated after failure of conservative measures. A surgical exploration of the peroneal tendon was performed through the posterior longitudinal incision given behind the fibula. The superior peroneal retinaculum was noted to be uninjured, and there was no subluxation of the tendon. Anatomical abnormalities such as peroneus quartus, low lying peroneus muscle belly, and abnormal shaped fibular groove were not noted. A longitudinal split of the peroneus brevis tendon about 2 cm long was found. Inflamed tendon sheath was excised, with excision of the longitudinal tear and attrited portion of tendon, remaining more than 50% thickness of the tendon was repaired in form of suture-tubulization of tendon with non-absorbable 4-0 nylon sutures [9]. In this 4-0 nylon sutures were applied as inverted sutures so that there smallest size knot remains facing at outer surface of tendon instead of remaining towards the peroneal groove. This will help in gliding the tendon, well in groove as well knot of tendon will not interfere in any function of tendon. The knot is buried in the substance of tendon. The excessive prominence of peroneal tubercle shaped to normal by undermining the base of tubercle, in this way anatomy near the tendon kept normal. We did closed the superior peroneal retinecula loosely over the tendon. After it wound was closed in layers.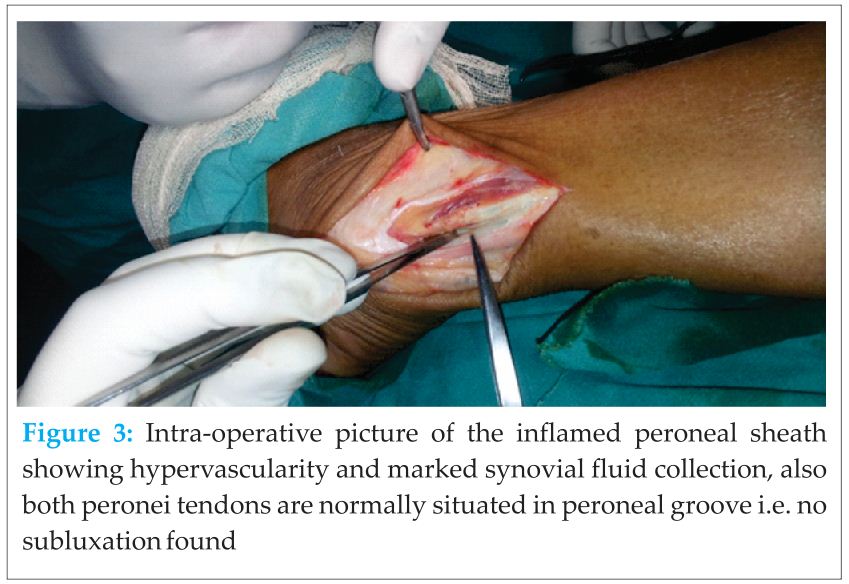
Post-operative protocol: Short leg non-walking cast was given for 2 weeks. At the end of 2 weeks removable short leg walking boot for 4 weeks given and the dorsiflexion and planter flexion exercises were begun. At the end of 6 weeks inversion exercises and progressive weight bearing was started. At 8 weeks eversion exercises started and walking boot was removed. At 4 months patient resumed normal activities with no pain.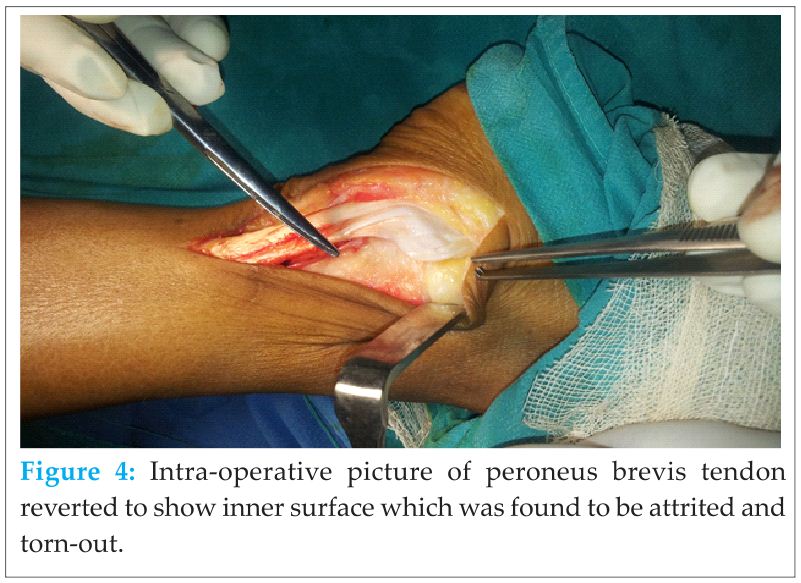
Discussion
Peroneal tendon pathology is rare and it is frequently undiagnosed. It should always be in the differential diagnosis of lateral ankle pain. Peroneus brevis tendon tears are not restricted to the elderly but can also occur in young population in conjunction with lateral ankle sprains. There are several causes of tendon attrition such as: [1] incompetence of the superior peroneal retinaculum, [2] subluxation of the peroneal tendon, and [3] compression from the peroneus longus tendon lying posteriorly to the sharp posterior ridge of the fibula [10,11]. Lateral ankle instability may contribute to it[1]. However, Bassett et al reported peroneal tendon tears in young athletes that occurred after their initial ankle sprains, and all these patients had stable ankles. Uninjured superior peroneal retinaculum with no subluxation of the peroneal tendon was confirmed surgically in all cases [12].Our technique of repairing the tendon is also one of the unique one as this did not interfere in healing of tendon.
Conclusion
Peroneal tendon tears without tendon subluxation are uncommon, especially in young people and may be left undiagnosed. Although rare but peroneus brevis tendon attrition and tear can occur without subluxation from peronal groove. Lateral aspect refractory ankle pain presenting with on and off swelling should arise suspicion of peroneal tendon tear. Correct diagnosis and proper surgical repair especially with inverted sutures which does interfere with healing of tendon in groove can produce excellent results.
Clinical Message
Refractory pain at lateral aspect of ankle associated with on & off pain and swelling may be due to peroneal tendon tear.Early diagnosis & surgical repair with grooving of back of fibula can lead to complete recovery.
References
1. Hyer CF, Dawson JM, Philbin TM, Berlet GC, Lee TH., The peroneal tubercle: description, classification, and relevance to peroneus longus tendon pathology . Foot Ankle Int. 2005 Nov;26(11):947-50.
2. Bruce WD, Christofersen MR, Phillips DL. Stenosing tenosynovitis and impingement of the peroneal tendons associated with hypertrophy of peroneal tubercle. Foot Ankle Int. 1999;20:464–467
3. Sobel M, Bohne WHO, Levy ME. Longitudinal attrition of the peroneus brevis tendon in the fibular groove: an anatomic study. Foot Ankle 1990;11:124–8.
4. Sammarco GJ, DiRaimondo C. Chronic peroneus brevis tendon lesions. Foot Ankle 1989;9:163–70.
5. Sobel M, Bohne W HO, DiCarlo E, et al. Longitudinal splitting of the peroneus brevis tendon: an anatomic and histologic study of cadaveric material. Foot Ankle 1991;12:165.
6. Major NM, Helms CA, Fritz RC, et al. The MR imaging appearance of longitudinal split tears of the peroneus brevis tendon. Foot Ankle Int 2000;21:514–19.
7. Schweitzer ME, Eid ME, Deely D, et al. Using MR imaging to differentiate peroneal splits from other peroneal disorders. AJR Am J Roentgenol 1997;168:129–33.
8. Sobel M, Geppert MJ, Olson EJ, Bohne WHO, Arnoczky SP., The dynamics of peroneus brevis tendon splits: A proposed mechanism, technique of diagnosis, and classification of injury. Foot and Ankle 1992;13(7):413-422.
9. Karlsson J, Wiger P, Longitudinal Split of the Peroneus Brevis Tendon and Lateral Ankle Instability:Treatment of Concomitant Lesions. Journal of Athletic Training 2002;37(4):463–466
10. Judith F. Baumhauer, Deborah A. Nawoczenski, Benedict F. DiGiovanni, A. Samuel Flemister, Ankle pain and peroneal tendon pathology. Clin Sports Med 23 (2004) 21– 34.
11. Sobel M, Geppert MJ, Warren RF. Chronic ankle instability as a cause of peroneal tendon injury. Clin Orthop 1993;296:187–91.
12. Bassett FH, Speer KP. Longitudinal rupture of peroneal tendons. Am J Sports Med 1993;21:354–7.
| How to Cite This Article: Tiwari M, Singh V, Bhargava R. Peroneus Brevis Attrition & Longitudinal Split Tear Without Subluxation and Associated Hypertrophy of Peronal Tubercle” – Treatment of an Uncommon Lesion. Journal of Orthopaedic Case Reports 2015 Jan-March;5(1): 34-36. Available from: https://www.jocr.co.in/wp/2015/01/28/2250-0685-250-fulltext/ |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com