[box type=”bio”] What to Learn from this Article?[/box]
Streptococcus pyogenes associated Brodie’s abscess is a cause of post-traumatic lytic lesion of the cuboid bone, and bone grafting is not always required for complete healing of the cavity.
Case Report | Volume 5 | Issue 3 | JOCR July-Sep 2015 | Page 84-86 | Priyadarshi Amit, Karthikeyan Maharajan, Bhaskar Varma. DOI: 10.13107/jocr.2250-0685.318.
Authors: Priyadarshi Amit[1], Karthikeyan Maharajan[2], Bhaskar Varma[1].
[1] Department of Orthopaedics, Acharyashree Bhikshu Government Hospital, Moti Nagar, New Delhi, India.
[2] Department of Orthopaedics, Sri Manakula Vinayagar Medical College and Hospital, Pondicherry, India.
Address of Correspondence
Dr. Priyadarshi Amit, 467, Ground Floor, Niti Khand I, Indirapuram, Ghaziabad – 201 010, Uttar Pradesh, India.
Email: drpamit@gmail.com
Abstract
Introduction: Brodie’s abscess of cuboid bone is one of the rarest diagnosis in children which most often is hematogenous in origin. Although Streptococcus pyogenes has been uncommonly implicated as causative organism in other bones, it is not yet reported in the cuboid.
Case Report: We report the case of 14-year-old boy who presented with a lytic lesion in the cuboid bone. It was preceded by a penetrating injury with a small iron nail. He was treated with simple curettage without the addition of bone graft. Frank pus present in the cavity in the cuboid bone grew S. pyogenes on bacterial culture. Symptoms resolved after 6 weeks of antibiotics, however, complete radiological healing was obtained after 9 months.
Conclusion: Although very rare, S. pyogenes associated Brodie’s abscess should strongly be suspected in a post-traumatic lytic lesion in the cuboid bone and bone grafting is not always required for bone healing even in presence of large pus-filled cavity.
Keywords: Brodie’s abscess, cuboid, osteomyelitis, Streptococcus pyogenes.
Introduction
Numerous cases of Brodie’s abscess have been reported since it was first described by Sir Benjamin Brodie in 1836 for a localized abscess in tibia bone [1]. Primary hematogenous variety is the most frequent type, mostly seen involving metaphysis of the long bones. However, its occurrence in small bones of hand and foot is a rarity [2]. Here, we present a case of non-hematogenous Brodie’s abscess in cuboid bone which was caused by direct invasion of Streptococcus pyogenes during trauma, treated with simple curettage, and also provide a review of relevant literature.
Case report
A 14-year-old boy presented to out-patient clinic at our hospital with moderate pain and swelling over left foot for 2 months duration which was preceded by a penetrating injury with small iron nail a month before the onset of symptoms. He was afebrile and was apparently healthy without systemic illness. Physical examination revealed mild soft tissue swelling over lateral aspect of midfoot with some tenderness without any sign of acute inflammation. He denied history of previous acute osteomyelitis or antibiotic treatment. A well circumscribed lytic lesion in an oval configuration surrounded by dense sclerotic rim was observed in subchondral region of cuboid bone on plain radiograph. Laboratory investigations (leukocyte count, C-reactive protein, blood culture) were inconclusive, except raised erythrocyte sedimentation rate (ESR) (36 mm/h; reference range 3-28 mm/h). Magnetic resonance imaging could not be performed due to the financial restraints of the patient. He was taken to operation theatre for curettage and biopsy. Subsequently, he was treated with intravenous antibiotics (augmentin and amikacin) for 3 weeks followed by 3 weeks of oral augmentin. Weight bearing was avoided for initial 3 months. He was followed up at 3, 6 and 9 months.
A cavity filled with yellowish frank purulent fluid (Fig. 1) along with small dark soft friable tissue (Fig. 2), surrounded by thick hard bony wall was found in the cuboid bone.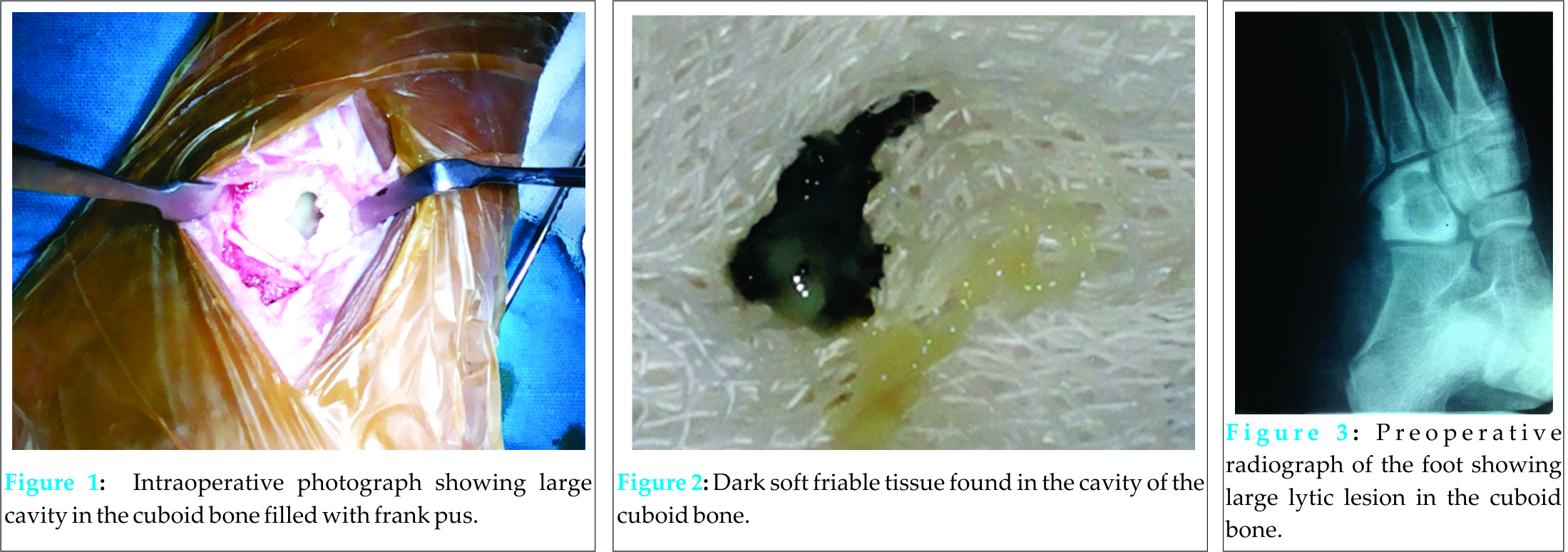 It was curetted till the appearance of punctate bleeding and the wound was closed over Penrose-type drain. Pus culture isolated S. pyogenes, and the dark tissue, on histological examination, revealed dense acute inflammation with foamy histiocytes and fragments of viable bone suggestive of an abscess. On follow-up, he showed complete resolution of disease without recurrence and complete radiological healing was achieved at 9 months (Figs. 3-6).
It was curetted till the appearance of punctate bleeding and the wound was closed over Penrose-type drain. Pus culture isolated S. pyogenes, and the dark tissue, on histological examination, revealed dense acute inflammation with foamy histiocytes and fragments of viable bone suggestive of an abscess. On follow-up, he showed complete resolution of disease without recurrence and complete radiological healing was achieved at 9 months (Figs. 3-6).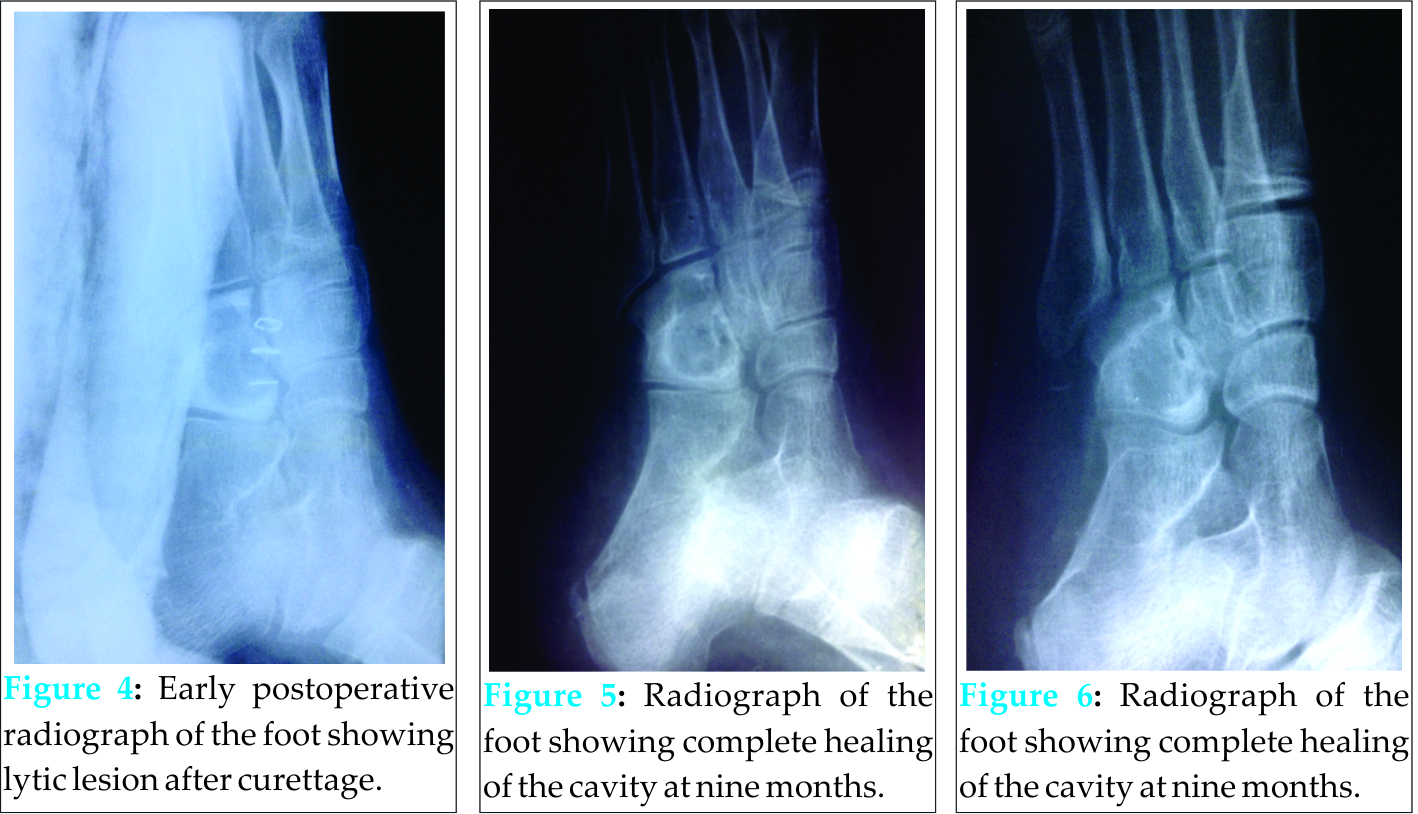
Discussion
Brodie’s abscess of the cuboid bone is an unusual cause of limp in pediatric males which occur without previous acute illness and systemic features [1]. The absence of characteristic sign and symptoms of an abscess along with the lack of specific laboratory test make it a difficult entity to diagnosis [2]. It requires a high index of suspicion, especially in context of predisposing factor like trauma. To the best of our knowledge, this is first reported a case of post-traumatic S. pyogenes associated Brodie’s abscess of the cuboid bone.
Although the pathogenesis of Brodie’s abscess i.e., hair loop arrangement of vessels in the metaphysis along with hypoxia, is same as that of acute osteomyelitis [2], primary hematogenous form of the disease develop when there is altered host-pathogen relationship as a result of increased host resistance or low bacterial virulence. It is also found to be associated with synovitis, acne, pustulosis, hyperostosis and osteitis syndrome or chronic recurrent multifocal osteomyelitis [3]. However, penetrating trauma has not yet been implicated as a predisposing factor. In our case, injury with an iron nail could have led to the introduction of pathologic organism into the bone from the external media, indicating non-hematogenous in origin. High host resistance due to barefoot walking was the additive factor in the development of the abscess.
Brodie’s abscess occurs most commonly at metaphysis of the tubular bones. Nevertheless, few authors have reported its occurrence in diaphysis of long bone, spine, clavicle, pelvis, metacarpal, metatarsal, calcaneus, navicula, and talus [3,4]. Non-hematogenous Brodie’s abscess of cuboid is rarely reported among tarsal bones. A literature search of published articles could find only two cases of Brodie’s abscess in cuboid bone [5,6]. However, none was associated with frank pus or a positive bacterial isolate or a trauma as a predisposing factor. Literature reports the rate of a positive bacterial isolate from the abscess as 75% [7]. Among them, Saphylococcus aureus is the most common bacteria, rest being Pneumococcus, Klebsiella [8], Salmonella typhi [7], Pseudomonas [4], Kingella kingae, Escherichia coli, Treponema pallidum, Framboesia, Actinomyces, Histoplasma [9]. Although, very few authors have isolated Streptococcus from tubular bones [5,9], it is not yet been found from small tarsal bones. Most of the abscess contains granulation tissue, nidus, etc. [4]. The presence of frank pus, which we saw in our case, is an uncommon finding for a Brodie’s abscess.
Moreover, there is no definite guideline for management of the Brodie’s abscess. Multiple options like curettage alone [4] or with antibiotics [3] or with antibiotics and bone grafting [8], or antibiotics alone [10] have been described in literature with variable success rates. Development of bony lesion has made many authors to undertake some kind of operative treatment [2]. Failure of symptoms to resolve after 6 weeks of antibiotic therapy, aggressive lesion, large lesion with size >3 cm diameter, sinus formation, drainage into a joint, ESR >40 mm/h, or clinical signs of subperiosteal pus have been suggested as indications for surgery [3,8,10]. When inadequately treated, this entity does recur, mostly in first 6 months [2]. We treated our patient with curettage and antibiotics, without the addition of bone grafting, which resulted in complete healing with no recurrence.
Conclusion
A penetrating injury to the cuboid bone can lead to S. pyogenes associated Brodie’s abscess. We suggest that bone grafting is not always necessary for bone healing even in the presence of large pus-filled cavity.
Clinical Message
S. pyogenes associated Brodie’s abscess should strongly be suspected in a post-traumatic lytic lesion in the cuboid bone. This condition can very well be managed by antibiotics and simple curettage, without adding bone graft even in the presence of large pus-filled cavity.
Reference
1. Brodie BC. An account of some cases of chronic abscess of the tibia. Med Chir Trans 1832;17:239-49.
2. Ezra E, Wientroub S. Primary subacute haematogenous osteomyelitis of the tarsal bones in children. J Bone Joint Surg Br 1997;79(6):983-6.
3. Hayek S, Segev E, Weintroub S. Primary subacute hematogenous osteomyelitis in children. Harefuah 2000;138(1):32-5.
4. Pabla R, Tibrewal S, Ramachandran M, Barry M. Primary subacute osteomyelitis of the talus in children: A case series and review. Acta Orthop Belg 2011;77(3):294-8.
5. Bagatur AE, Zorer G. Brodie’s abscess of the cuboid bone: A case report. Clin Orthop Relat Res 2003;(408):292-4.
6. Agarwal S, Akhtar MN, Bareh J. Brodie’s abscess of the cuboid in a pediatric male. J Foot Ankle Surg 2012;51(2):258-61.
7. Ip KC, Lam YL, Chang RY. Brodie’s abscess of the ulna caused by Salmonella typhi. Hong Kong Med J 2008;14(2):154-6.
8. Olasinde AA, Oluwadiya KS, Adegbehingbe OO. Treatment of Brodie’s abscess: Excellent results from curettage, bone grafting and antibiotics. Singapore Med J 2011;52(6):436-9.
9. Harris NH, Kirkaldy-Willis WH. Primary subacute pyogenic osteomyelitis. J Bone Joint Surg Br 1965;47:526-32.
Mehdinasab SA, Sarafan N, Najafzadeh-Khooei A. Primary subacute osteomyelitis of the greater trochanter. Arch Iran Med 2007;10(1):104-6.
| How to Cite This Article: Amit P, Maharajan K, Varma B. Streptococcus pyogenes Associated Post-traumatic Brodie’s Abscess of Cuboid: A Case Report and Review of Literature. Journal of Orthopaedic Case Reports 2015 July – Sep;5(3): 84-86 . Available from: https://www.jocr.co.in/wp/2015/07/10/2250-0685-318-fulltext/ |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com









