[box type=”bio”] What to Learn from this Article?[/box]
Conjoint Lumbosacral Nerve Root- Radiologists Might Miss But Surgeons Eyes Must Not.
Case Report | Volume 5 | Issue 4 | JOCR Oct-Dec 2015 | Page 14-16 | Vispi.H.Jokhi, Saurabh Vilas Ponde, Chandrashekhar Sonawane, Samarjit Singh Bansal, Ashwin Chavhan. DOI: 10.13107/jocr.2250-0685.334
Authors: Vispi.H.Jokhi[1], Saurabh Vilas Ponde[1], Chandrashekhar Sonawane[1], Samarjit Singh Bansal[1], Ashwin Chavhan[1].
[1] Department of Orthopaedics, ESIPGIMSR and MGM Hospital, Parel, Mumbai – 400012. Maharashtra. India.
Address of Correspondence
Dr. Samarjit Singh Bansal,
2nd Floor Plot No.85, Abhinav Nagar, Borivali East, Mumbai-400066. India.
E mail – samarjit212@gmail.com
Abstract
Introduction: Conjoint nerve root is embryological nerve root anomaly mainly involving lumbosacral region. The anomalous roots present primarily as a bifid, conjoined structure arising from a wide area of the dura. Because of their size and attachment to surrounding structures, they are uniquely susceptible to trauma. The effects of compression and entrapment are amplified in the presence of stenosis of the lateral recesses where developmental changes and disc herniations deplete the available reserve space [1].
Case Report: We report a case of conjoint lumbosacral nerve root which was missed on MRI and diagnosed intra-operatively.
Conclusion: The importance of the case report lies in the fact that one must be aware of finding conjoint nerve root directly while operating and do appropriate level of surgery, misinterpretation can lead to devastating results.
Keywords: conjoint nerve root, MRI.
Introduction
Conjoint nerve root is an embryological nerve root anomaly mainly involving the lumbosacral region. The anomalous roots present primarily as a bifid, conjoined structure arising from a wide area of the dura. Because of their size and attachment to surrounding structures, they are uniquely susceptible to trauma. The effects of compression and entrapment are amplified in the presence of stenosis of the lateral recesses where developmental changes and disc herniations deplete the available reserve space [1]. The anomalous root may be difficult to recognize even at the operating table because of swelling and reactive changes which obscure the anatomical details so that the appearance may simulate that of mass lesion.We are reporting a case of conjoint L4-L5 nerve root in a case of spina bifida with severe lumbar canal stenosis.
Case report
38 years old male worker came with chief complaint of low backache and intermittent bilateral lower limb tingling numbness since last 10 years, symptoms had intensified for the past 4 months. Claudication pain was severe and appeared within 10 minutes of walking or standing. Patient was unable to carry on his daily activities with many days of absenteeism from work. No neural deficit on clinical examination. Patient had received conservative management for 3 months but with no relief. X-ray LS spine suggestive of decreased L4-L5 disc space with spina bifida at L5 level. MRI-LS Spine showed Central and lateral recess stenosis at L4-L5 level and moderate stenosis at L3-L4 level with lumbarised S1 vertebra was reported.We decided to operate him .Decompression with L4 laminectomy and bilateral foraminotomy was planned. Intraoperatively, spina bifida was noted at L5 level. Following flavectomy, an unusual appearance of the anatomical structures was encountered. There were two roots emerging separatelyfrom the dural sac, and entering through the same spinal foramen. Right L4 and L5 were leaving through L5 foramen. Both L4, L5 roots were severely compressed at origin and along the course at lateral recess by thickened ligamentum flavum. Post-operatively, patient recovered from his claudication pain almost immediately and pain disappeared completely in 2 weeks. The patient is now able to do his work without any kind of restriction and disability.
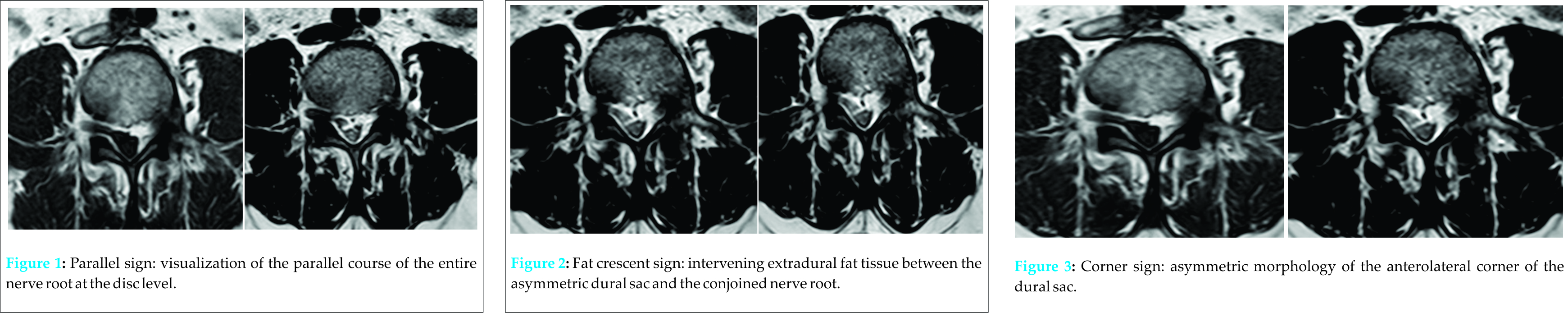
Retrospective evaluation of the MRI brought to our attention all the three signs of conjoint nerve root which were previously overlooked.
Discussion
There have been several reports of lumbosacral root anomalies discovered during surgery undertaken for suspected disc herniation [2,3,4]. Anomalies of the lumbosacral nerve roots probably result from aberrant migration of the involved roots during their embryological development [2]. They could occur either as the result of a local factor, or as a consequence- of widespread embryological disorders associated with other anomalies such as sacrum bifidum, and situsinversus of the viscera. The percentage incidence of these nerve root anomalies shows a range comprised between 0.3 and 30%, although the last figure may be overestimated [5]. The roots most frequently involved by the anomaly are L5 and S1[6], accounting for 50% of the total number, while S2 anomalies account approximately for one third of cases; anomalies of other roots are rare. Multiple malformations may be frequent and the majority of them occur on the left side [5].
According to Cannon et al [2], there are three fundamental types of nerve root anomalies
Type I: conjoined (or confluent) type, in which 2 roots
share a common sleeve that originates from the dura mater
Type II (anastomotic type) in which a normal root bifurcates abnormally after it leaves the dura and branches out to the next caudal nerve
Type III (transverse type) in which the nerve root leaves
The dural sac at almost a right angle.
Nerve root anomalies may cause symptoms at more than one level as a result of pressure by, for example, a herniated intervertebral disc. Pressure on an abnormally situated nerve root may also give an incorrect indication of the level of disc herniation. The anomalous roots occupy most of the space in the vertebral canal so that even slight bulging of an intervertebral disc or swelling of a root may cause symptoms.
Conclusion
The diagnosis of a conjoined nerve root anomaly has several points of significance. If not correctly interpreted, it could be mistaken for a herniated disc. The spine surgeons should be aware of these anomalies. If not correctly diagnosed, it can result in wrong level of surgery with a poor outcome. If approached with limited exposure, it could further result in serious damage to the anomalous roots. Raynolds (1954) has shown that sectioning some of these anomalous roots may result in irreversible motor or sensory loss. We conclude that correct diagnosis of root anomalies is important for the patient, any misinterpretation could lead to catastrophic consequences.
Clinical Message
.All surgeons operating on spine should be aware of the anomalies of nerve roots which sometimes can be missed on MRI, and misinterpretation as herniated disc can lead to devastating results especially during limited approach to spine.
References
1. Epstein JA, Carra R. Ferrar J, Hyman RA, Khan A. Conjoined lumbosacral nerve roots; Management of herniated discs and lateral recess stenosis in patients with this anomaly. J Neurosurg 1981;55:585-589.
2. Cannon BW, Hunter Se, Picaza JA. Nerve-root anomalies in lumbar disc surgery. J Neurosurg 1962;19:208-214.
3. Ethelberg S, Riishede J. Malformations of lumbar spinal roots and sheaths in the causation of low back ache and sciatica. J Bone Joint Surg B 1952;34:442-446.
4. Rask MR. Anomalous lumbosacral nerve roots associated with spondylolisthesis. SurgNeurol 1977;8:139-140.
5. Artico M, CarloiaS, PiacentiniM,. FerrettiG, . DazziM, Franchitto S et al. Conjoined lumbosacral nerve roots: observations on three cases and review of the literature. Neurocirugía 2006; 17:54-59
6. Kadish LJ, SimmonsEH. Anomalies of the lumbosacral nerve roots. An anatomical investigation and myelographic study. J Bone Joint Surg B 1984;66:411-416.
| How to Cite This Article: Bansal SS, Jokhi VH, Ponde SV, Sonawane C, Chavhan A. Conjoint Lumbosacral Nerve Root- A Case Report. Journal of Orthopaedic Case Reports 2015 Oct-Dec;5(4): 14-16. Available from: https://www.jocr.co.in/wp/2015/10/01/2250-0685-334-fulltext/ |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com