[box type=”bio”] What to Learn from this Article?[/box]
Gorham’s is a rare disease, difficult to diagnose and manage.
Case Report | Volume 5 | Issue 4 | JOCR Oct-Dec 2015 | Page 30-33 | Gedam PN, Dhamangaonkar AC, Parekh AN. DOI: 10.13107/jocr.2250-0685.339 .
Authors: Gedam PN[1], Dhamangaonkar AC[2], Parekh AN[1]
[1] Department of Orthopaedics, BYL Nair Ch. Hosp. and Topiwala National Medical College, Mumbai-400008. Maharashtra. India.
[2] Department of Orthopaedics, Lokmanya Tilak Municipal Medicl College & General Hospital, Sion, Mumbai-400022. Maharashtra. India.
Address of Correspondence
Dr. Anoop C Dhamangaonkar,
Department of Orthopaedics, Suite no. 115, First Floor, College Building, Lokmanya Tilak Municipal Medical College and General Hospital, Sion, Mumbai 400022, Maharashtra, India. Email: anoopd_7@yahoo.com
Abstract
Introduction: ‘Vanishing Bone Disease’ or Gorham’s disease is a very rare form of primary idiopathic osteolysis with only around 200 cases being reported till date. We present in this case report a ten year follow-up of a patient who had progressive osteolysis of the right shoulder girdle and eventually involved the spine inspite of supplementary calcium and bisphosphonate therapy. We also report the utility of using an intra-medullary device is to attain acceptable union in case of pathological long bone fracture in Gorham’s disease.
Case: A four year old child presented to us with a spontaneous osteolysis of the right scapula ten years ago in 2003. Within two years, the osteolysis progressed to the entire scapula, clavicle and he had a clavicular fracture. The patient was treated conservatively, oral calcium and bisphosphonate therapy was initiated after ruling out any metabolic bone disease. The patient again sustained a pathological fracture humerus five years later, which was treated with open reduction and internal fixation with an intra-medullary K wire. The fracture united without any other supplementary treatment but osteolysis continued to progressively involve the entire scapula, proximal humerus, clavicle, upper two ribs and the cervical spine.
Conclusion: Gorham’s disease is a rare disease with an unpredictable course without any satisfactory treatment. There is still a role for surgical intervention to treat long bone pathological fractures secondary to Gorham’s disease with an intra-medullary device. The fractures unite without any other supplementary radio or chemotherapy.
Keywords: Gorham’s; spontaneous; osteolysis; progressive; fracture.
Introduction
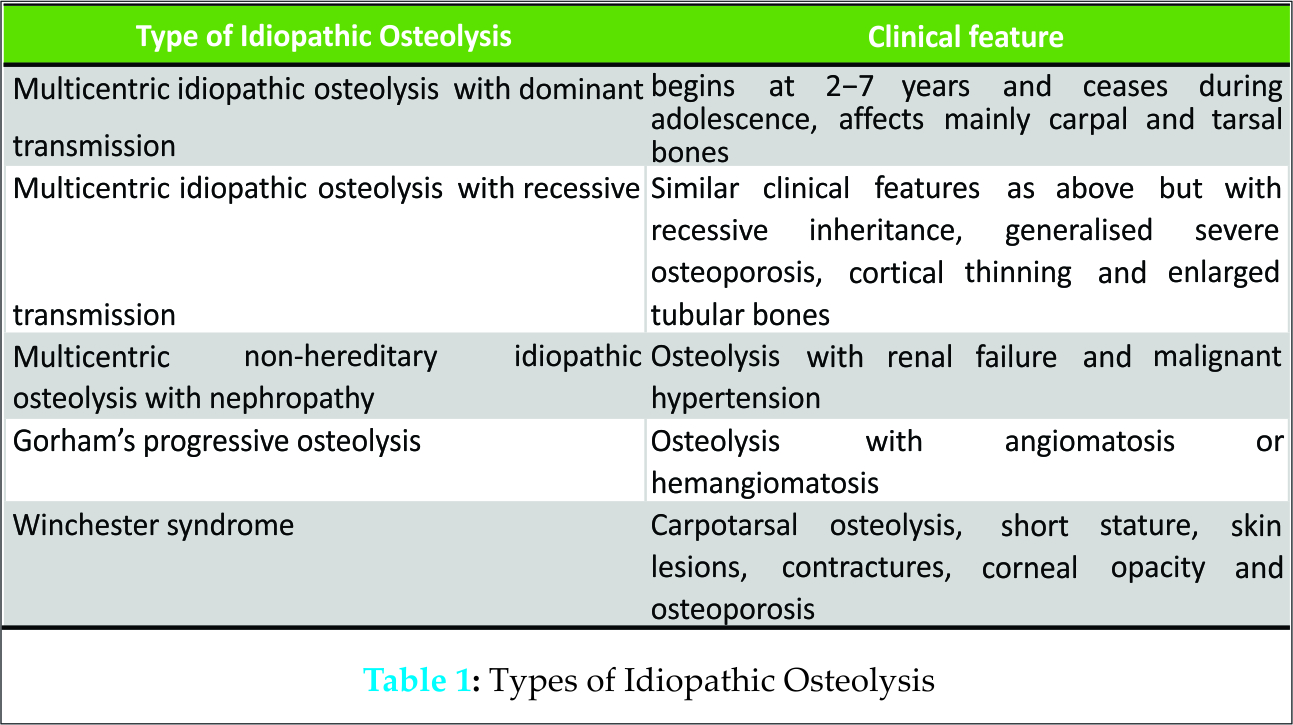
Primary idiopathic osteolysis is characterized by spontaneous resorption of bone without any known causative factors. There were initially four different types described by Torg et al.[1] Later, a fifth type too was described [2]. Gorham’s disease one of the five types of primary idiopathic osteolysis [Table 1].
The disease was first described by Jackson in 1838 [3,4]. In 1955, Gorham and Stout [5] tabulated 24 previously reported cases and the condition then came to be known as Gorham’s disease [3,4]. Various other names have been described in the literature; those most commonly used are “vanishing bone disease”, “phantom bone disease” and “disappearing bone disease” [6]. We present a ten-year follow-up of a four year old child with progressive Gorham’s disease of the right shoulder girdle with a pathological fracture which united after an intramedullary fixation without any supplementary treatment modality.
Case Report
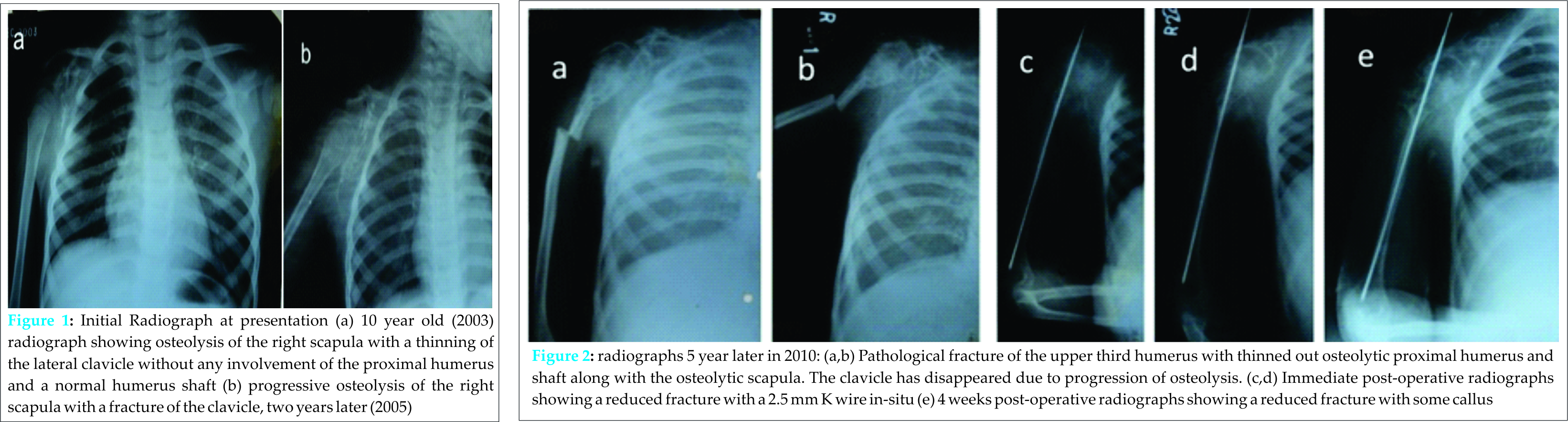
A four year old male patient presented with dull pain at the right shoulder region and inability to abduct the right shoulder in 2003. There was no history of trauma at that time. The radiograph showed osteolysis of the scapula, with some thinning of the lateral third of the clavicle, without the involvement of proximal humerus (Fig.1a). Two years later, in 2005, the patient had pain over the right clavicular region. The radiograph showed a fracture of the right-sided clavicle with progressive osteolysis of the scapula but the proximal humerus was normal (Fig.1b). The patient was treated conservatively with a clavicular brace. A complete laboratory work-up was done to rule out any metabolic bone disease and all test reports were normal. There was a clinical suspicion of this case being an example of Gorham’s disease. The patient was advised radiotherapy, but the patient refused the same considering his young age. However, the child was kept on oral calcium and oral bisphosphonate (alendronate 1mg/kg) therapy. The patient did not follow-up till 2010, when the patient presented with a fracture of upper third shaft of humerus following a trivial fall.
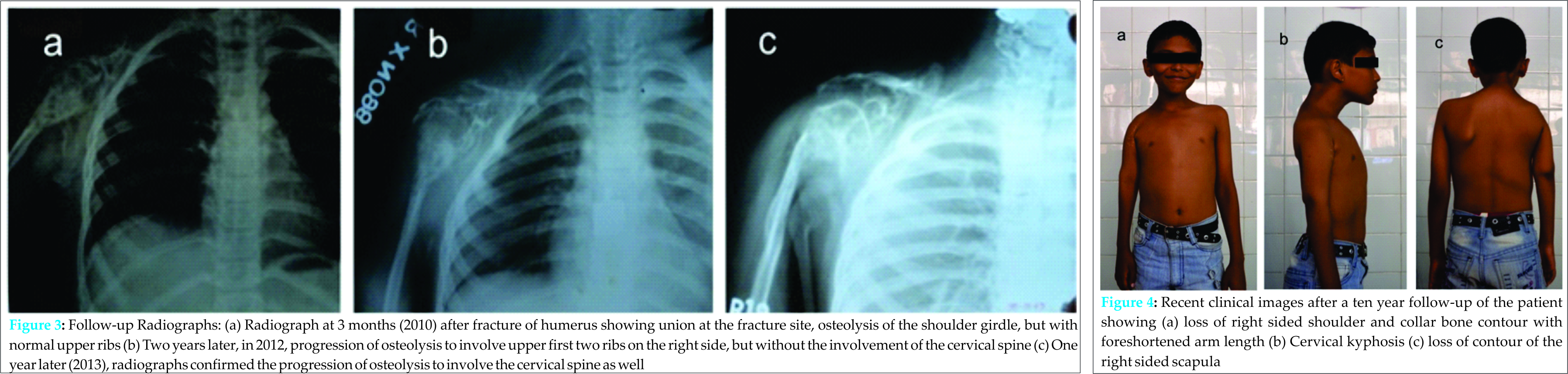
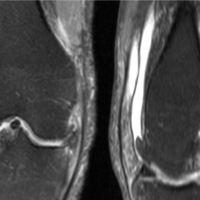
The radiographs confirmed the site of the fracture with progression of osteolysis with disappearance of the clavicle and involvement of the proximal humerus and thinning of the humerus shaft (Fig. 2a,b). The patient then underwent an open reduction and internal fixation with a long percutaneous K-wire (Fig. 2 c,d,e) and the patient was given a U slab, which was later was converted to a U cast. A biopsy was sent for histopathology, since a sufficient bone tissue could be sampled at this stage. Histopathology showed presence of edematous bony tissue with an abundance of inflammatory cells with a great number of thick-walled blood vessels and no evidence of malignancy. This confirmed the case to be Gorham’s disease. Due to the pin tract infection, the wire was removed after 2 months but immobilization was continued for another month. The fracture united after 3 months (Fig. 3a).
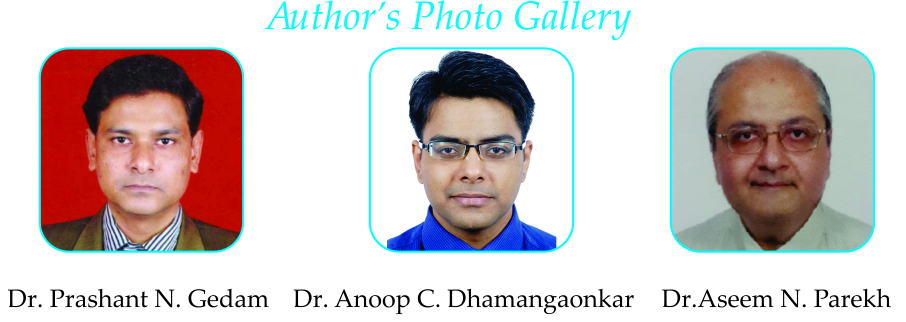
After two years in 2012, the patient came for a follow-up. The radiographs at this time showed progression of osteolysis with scalloping of the upper two ribs in addition to that of the shoulder girdle. However, the cervical spine was unaffected (Fig. 3b). A year later, in 2013, the patient presented back with a wasted shoulder girdle without any active movements at the shoulder and a cervical kyphosis and terminal restriction of movements of the cervical spine (Fig. 4 a,b,c). The radiographs confirmed the presence of progressive osteolysis of the proximal humerus, scapula, clavicle, upper ribs and an involvement of the cervical spine (Fig 3c). There was no evidence of any neurological deficit. After this, the patient was lost to follow-up.
Discussion
Gorham’s disease is a rare form of primary idiopathic osteolysis. Only around 200 cases of Gorham’s disease have been reported till date. Gorham’s disease is differentiated from other types of primary osteolysis by being a monocentric benign vascular tumor causing osteolysis, not having any predilection for carpo-tarsal area, not having a hereditary pattern nor any associated nephropathy [7]. It can occur at any age. Though the exact trigger for the disease is not understood, the pathological process is well understood. It is a non-neoplastic vascular tissue similar to haemangioma or lymphangioma that replaces the bone.
It was thought that trauma initiates local vascular granulation tissue that brings about osteolysis by hyperemia, change in the pH, mechanical forces, increased activity of osteoclasts or mononuclear perivascular cells, deranged osteoblastic function and increased IL-6 activity. There is minimal new bone formation. In later stages, osseous tissue is spontaneously replaced by fibrous tissue.
Gorham’s disease has an unpredictable natural history. It may spontaneously arrest or worsen progressively until all osseous tissue disappears. Osteolysis may be restricted to just one bone or it may spread to contiguous bones. The disease is biphasic in that there are episodes of active osteolysis, followed by asymptomatic, latent periods. The onset is insidious, with dull pain in the affected area. At first, the disease presents as radiolucent foci which look like patchy osteoporosis. This osteolysis progressively increases with further loss of bone mass. The ends of the affected bones shrink producing a “sucked candy” appearance. Gorham’s disease is known to cause deformity but may be life threatening due involvement of viscera or chest resulting in chylothorax [5] or after involvement of spine, though the involvement of the spine is extremely rare [4]. The diagnosis of Gorham’s disease is based on clinical, radiological and histological findings. In 1983, Heffez, et al. proposed the following diagnostic criteria for Gorham’s disease [8]:
1. Presence of angiomatous tissue on biopsy
2. Absence of cellular atypia
3. Minimal or no osteoblastic response and absence of dystrophic calcification.
4. Evidence of local progressive osseous resorption
5. Non-expansile, non-ulcerative lesion
6. Absence of visceral involvement
7. Osteolytic radiographic pattern
8. Negative hereditary, metabolic, neoplastic, immunologic, or infectious etiology
Our case was diagnosed of being Gorham’s disease based on the above mentioned criteria. The differential diagnosis includes Langerhans cell disease, skeletal angiomas, essential and hereditary osteolysis which may be ruled out by radiographic studies and proper blood tests including serum complement levels, tests for vasculitis, parathyroid hormone levels, 24-hour urinary proteins and electrophoresis of plasma proteins [9].
The non-surgical treatment modalities include chemotherapy, radiation therapy, bisphosphonates, calcium supplements, interferon, vitamins, calcitonin, antibiotics, antivirals, antifungals and embolization [10-12]. Surgical intervention has been recommended for patients with Gorham’s disease of the spine along with a neurodeficit or deformity. However, no treatment modality has proven to give satisfactory results. But the results of surgical stabilization were poor in most cases due to the resorption of the graft [3]. There is currently no single recommendation in contemporary English literature regarding whether to operate or conserve a pathological fracture, and what implant to use in case of a long bone pathological fracture after Gorham’s disease. Also, whether or not to initiate radiotherapy or chemotherapy in a child remains a clinical dilemma. All these issues were debated in our case. Operating on the pathological fracture was considered since we could retrieve a substantial sample for biopsy and also stabilize the fracture by some kind of internal splint. Plating was not an option considering the poor bone quality. There have been reports of implant failure after plating [13]. While putting in an intra-medullary implant, there was room only enough for a 2.5mm thick K wire to be accommodated and the fracture eventually united. The treatment options for spinal stabilization procedure and radiotherapy were, however, turned down by the patient’s guardians.
Conclusions
Gorham’s disease is a rare disease and must be diagnosed early. The progression of Gorham’s disease is unpredictable with regards to location and duration of spread and also response to calcium and bisphosphonate therapy. There is still a role for surgical intervention to treat long bone pathological fractures secondary to Gorham’s disease with an intra-medullary device. The fractures unite without any other supplementary radio or chemotherapy. There is a need for further research to have effective and predictable results in Gorham’s disease.
Clinical Message
Gorham’s disease is a rare clinical entity of primary idiopathic progressive osteolysis and must be diagnosed early but the clinical course of the disease is unpredictable. Utility of calcium and bisphosphonate therapy is questionable. There is still role of internal fixation of pathological fractures of long bones and fractures unite without any supplementary radio or chemotherapy.
References
1. Torg JS, DiGeorge AM, Kirkpatrick JA Jr, Trujillo MM. Hereditary multicentric osteolysis with recessive transmission: a new syndrome. J Pediatr 1969;75:243-52.
2. Macpherson RI, Walker RD, Kowall MH. Essential osteolysis with nephropathy. J Can Assoc Radiol1973;24:98-103.
3. Aizawa T, Sato T, Kokubun S. Gorham disease of the spine: a case report and treatment strategies for this enigmatic bone disease. Tohoku J Exp Med 2005;205:187-96.
4. Ruggieri P, Montalti M, Angelini A, Alberghini M, Mercuri M. Gorham-Stout disease: the experience of the Rizzoli Institute and review of the literature. Skeletal Radiol 2011;40:1391-7.
5. Gorham LW, Stout AP. Massive osteolysis (acute spontaneous absorption of bone, phantom bone, disappearing bone); its relation to hemangiomatosis. J Bone Joint Surg Am 1955;37:985-1004.
6. Patel DV. Gorham’s disease or massive osteolysis. Clin Med Res 2005;3:65-74.
7. Hardegger F, Simpson LA, Segmueller G. The syndrome of idiopathic osteolysis. Classification, review and case report. J Bone Joint Surg Br 1985;67:88-93.
8.Heffez L, Doku HC, Carter BL, Freeney JE. Perspectives on massive
osteolysis: report of a case and review of literature. Oral Surg Oral Med Oral Pathol. 1983; 55: 331 – 343.
9.Johnson PM, McClure JG. Observations on massive osteolysis: a re- view of the literature and report of a case. Radiology. 1958; 71: 28
– 42.
10. Paley MD, Lloyd CJ, Penfold CN. Total mandibular reconstruction for massive osteolysis of the mandible. Br J Oral and Maxillofac Surg. 2005; 43: 166 – 168.
11. Vinée P, Tanyü MO, Hauenstein KH, Sigmund G, Stöver B, Adler CP. CT and MRI of Gorham syndrome. J Comput Assist Tomogr. 1994; 18: 985 – 989.
12. Yoo SY, Hong SW. Chung HW, Choi JA, Kim CJ, Kang HS. MRI of Skeletal Radiol. 2002; 31: 301 – 306.
13. Baba AN, Bhat YJ, Paljor SD, Nazir A, Khan NA. Gorham’s disease of Femur. Indian J Orthop. 2011 Nov;45:565-8.
| How to Cite This Article: Gedam PN, Dhamangaonkar AC, Parekh AN. A Rare Case of Progressive Gorham’s Disease of Right Shoulder Girdle and Cervical Spine in A Child: 10 Year Follow-up and A Review of Literature. Journal of Orthopaedic Case Reports 2015 Oct-Dec;5(4): 30-33. Available from: https://www.jocr.co.in/wp/2015/10/01/2250-0685-339-fulltext/ |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com