[box type=”bio”] What to Learn from this Article?[/box]
If giant cell tumors are identified at an early stage, it is possible to ensure enblock resection and prevent its recurrence.
Case Report | Volume 6 | Issue 1 | JOCR Jan-Mar 2016 | Page 20-22 | Mihir Upadhyaya, Sachin Kale, Prasad Chaudhary, Sanjay Dhar. DOI: 10.13107/jocr.2250-0685.367
Authors: Mihir Upadhyaya[1], Sachin Kale[1], Prasad Chaudhary[1], Sanjay Dhar[1]
[1]Department of Orthopaedics, Padmashree Dr.D.Y.Patil Hospital and Research Centre, Nerul, Navi Mumbai. Maharashtra. India.
Address of Correspondence
Dr. Mihir Upadhyaya,
271, Enterprise, Forjet Hill Road, Tardeo, Mumbai- 400036. Maharashtra. India. Email – mihirace@gmail.com.
Abstract
Introduction: Giant cell tumor accounts for 5 to 9 percent of all primary bony tumors. Giant cell tumors are usually found in the long bones, most often the distal femur, proximal tibia, distal radius and rarely arising from the ribs. In this paper, we describe a case of giant cell tumor presented at an unusual location of the costovertebral junction as a dumbbell shaped tumor.
Case Report: Authors report a case of a 27 year old male patient with a giant cell tumor arising from the costovertebral junction at D7, D8, and D9 levels compressing the cord. Well-defined osteolysis with nonsclerotic borders were visualized on radiographs and CT scan images. Intermediate signal intensity on T1 sequences and central high signal and peripheral intermediate signal intensity on T2 sequences was visualized on MRI images. CT guided biopsy was reported as a moderately vascular lesion with spindle cell neoplasm suggestive of schwannoma .The cord was decompressed, tumor mass was surgically resected and stabilization with instrumentation was done. Histopatholgy was suggestive of giant cell tumor.
Conclusion: Giant cell tumor may be included in the differential diagnosis in a well-defined lytic lesion when involving the costovertebral junction presenting as a spindle cell tumor on biopsy reports.
Keywords: Giant cell tumor; Spindle cellneoplasm; Schwannoma ; Costovertebral junction.
Introduction
Giant cell tumor (GCT) accounts for 5 to 9 percent of all primary bony tumors. Giant cell tumors are usually found in the long bones, most often the distal femur, proximal tibia, and distal radius [1–3] and rarely the ribs. Giant cell tumor of bone is a benign lesion that is usually solitary and locally aggressive. It is believed by some to be potentially malignant. It possibly is the most common bone tumor in the young adults aged 25 to 40. Giant cell tumor is found more commonly in women than men, and occurs most often during the third decade [1–3].
Case Presentation
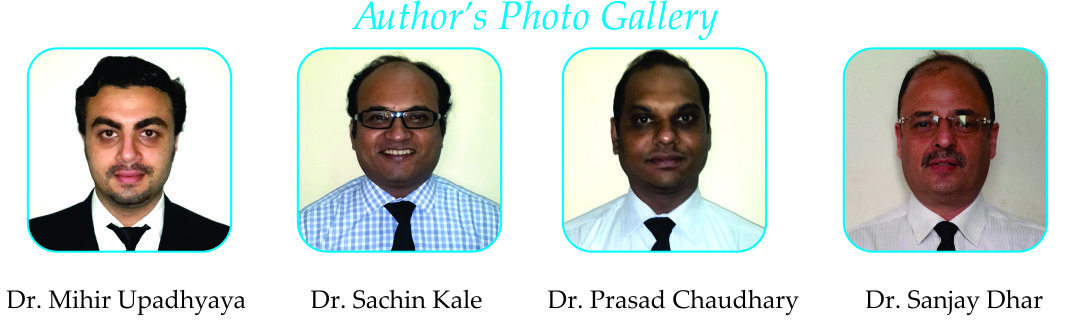
A 27 year old male presented with sudden onset bilateral lower limb weakness (Grade 4/5) of all muscle groups without bowel and bladder involvement. On examination, there was superficial and deep tenderness at the D7,D8,D9 spinous process and a palpable mass at the D7,D8, and D9 paraspinal region on the right side. Radiographs showed scoliotic deformity at upper dorsal spine and soft tissue enhancement in the right mediastinal region at the D6,D7, and D8 region in the anteroposterior view ( Fig 1). Kyphotic deformity noted at the upper dorsal spine and reduction of disc space at D7-D8 and D8-D9 level (Fig 1). Computed Tomography (CT) confirmed the presence of the lesion, which showed soft tissue density (Figs 2,3). On Magnetic Resonance Imaging (MRI), the lesion showed intermediate signal intensity on T1 sequences, while on T2 sequences a high signal center and an intermediate signal periphery were observed (Figs 4,5). 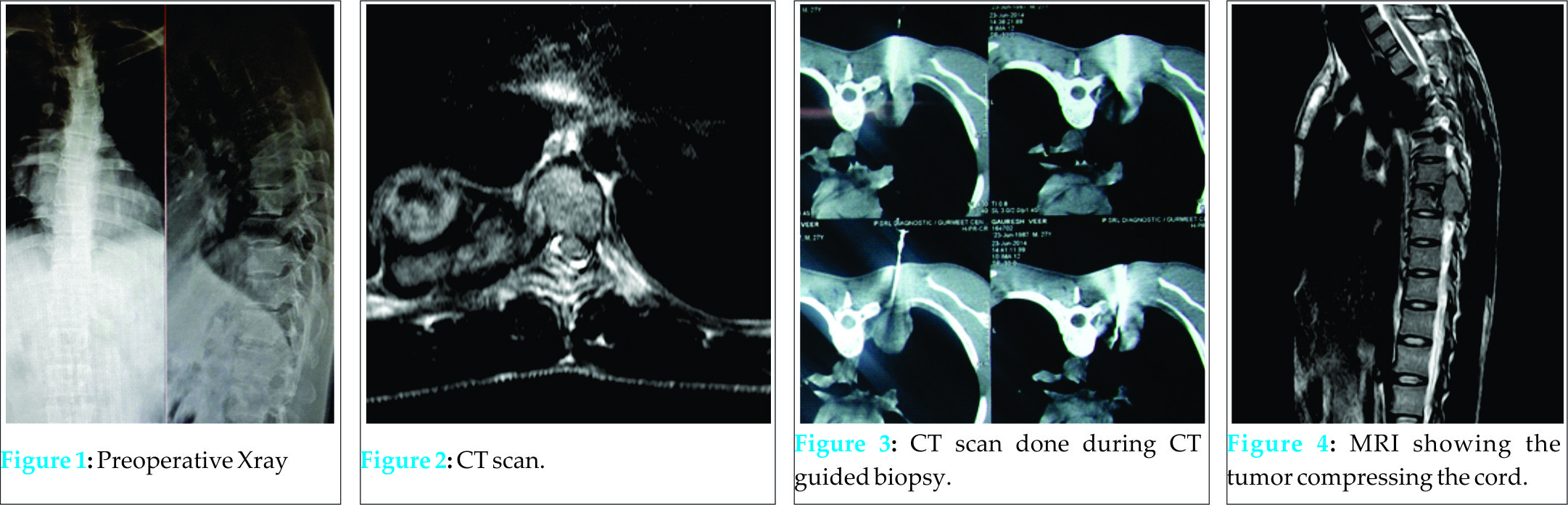 After administration of paramagnetic contrast agent, both central and peripheral-periosteal enhancement was noted. On CT guided biopsy, sections revealed spindle cell neoplasm containing siderophages. Fibromyxoid stromal matrix was seen. Lesion was moderately vascular with occasional vessels showing mild hyaline thickening of vessel wall. Focally, spindle cells showed neurogenic features suggestive of schwannoma. Laboratory tests (including serum calcium, phosphorus, acid phosphatase, and alkaline phosphatase) were unremarkable. Intraoperatively, we found a large friable tumor mass which was adherant to the pleura of the right lung arising from the D7, D8, D9 costovertebral junction compressing the spinal cord (Fig 6).
After administration of paramagnetic contrast agent, both central and peripheral-periosteal enhancement was noted. On CT guided biopsy, sections revealed spindle cell neoplasm containing siderophages. Fibromyxoid stromal matrix was seen. Lesion was moderately vascular with occasional vessels showing mild hyaline thickening of vessel wall. Focally, spindle cells showed neurogenic features suggestive of schwannoma. Laboratory tests (including serum calcium, phosphorus, acid phosphatase, and alkaline phosphatase) were unremarkable. Intraoperatively, we found a large friable tumor mass which was adherant to the pleura of the right lung arising from the D7, D8, D9 costovertebral junction compressing the spinal cord (Fig 6).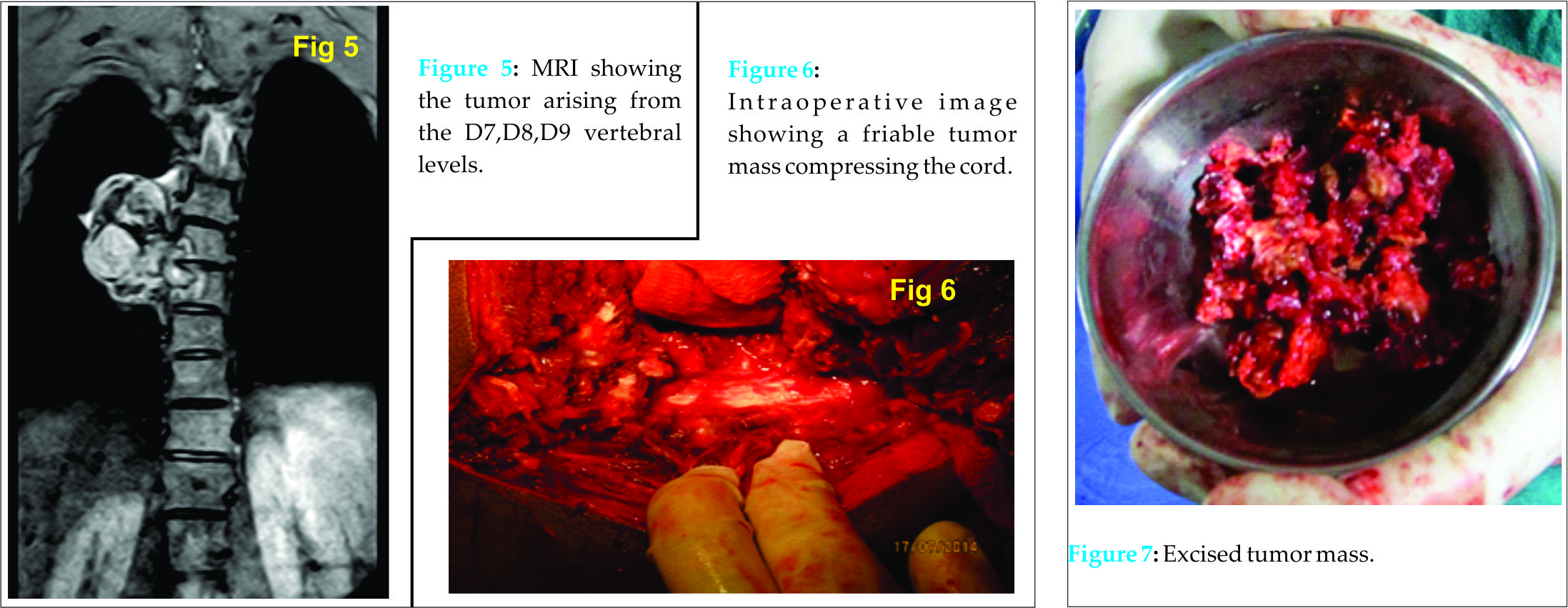 Using a right transthoracic (single staged combined anterior and posterior) approach, en bloc tumor resection (Fig 7) of size (5cm x 5cm) with partial excision of the affected 7th,8th and 9th rib was done followed by stabilization with heartshield cage and sublaminar wires (Fig 8). Intraoperatively samples of the tumor mass with the affected ribs were sent for histopathological examination which showed polygonal stromal cells, osteoclastic giant cells and many hemosiderin laden macrophages on high power view (Fig 9). Postoperatively patient’s neurological status improved.
Using a right transthoracic (single staged combined anterior and posterior) approach, en bloc tumor resection (Fig 7) of size (5cm x 5cm) with partial excision of the affected 7th,8th and 9th rib was done followed by stabilization with heartshield cage and sublaminar wires (Fig 8). Intraoperatively samples of the tumor mass with the affected ribs were sent for histopathological examination which showed polygonal stromal cells, osteoclastic giant cells and many hemosiderin laden macrophages on high power view (Fig 9). Postoperatively patient’s neurological status improved.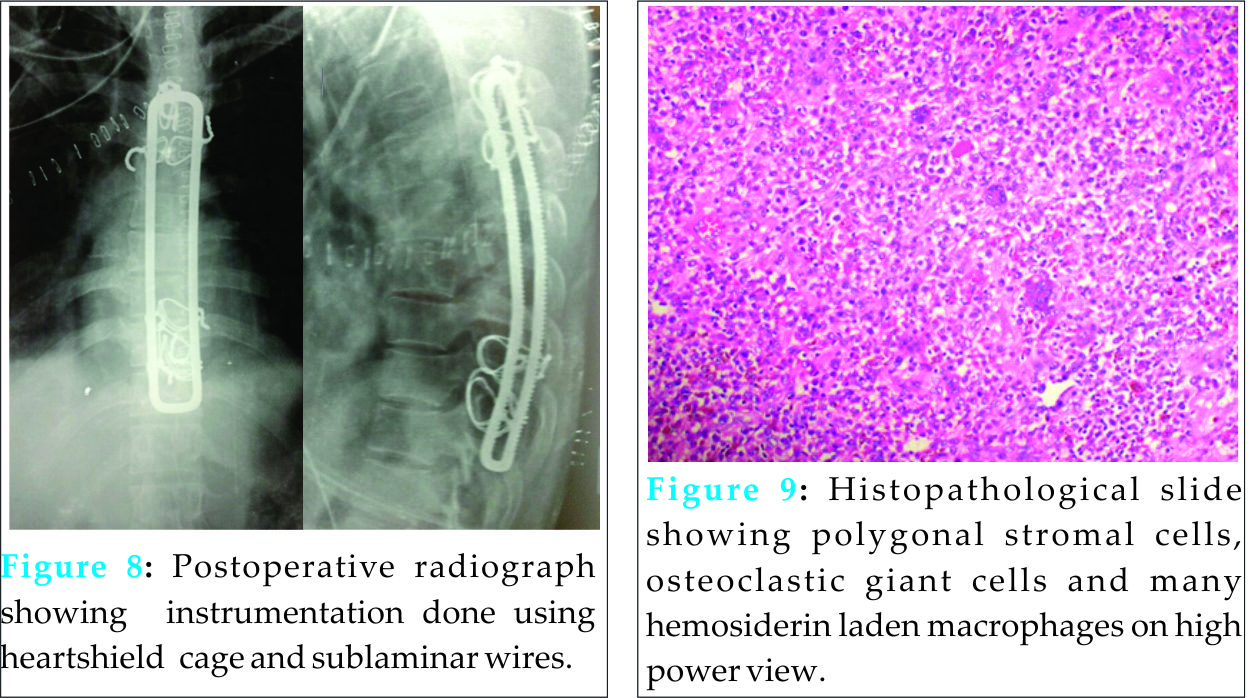
Discussion
Giant cell tumors are benign, though aggressive neoplasms accounting for 5 to 9 percent of all primary bony tumors [1]. Giant cell tumors are usually found in the long bones, most often the
distal femur, proximal tibia, and distal radius [3]. GCT rarely arises in ribs (<1% in most series) [1, 2]. The posterior parts of the rib (head and tubercle) are most commonly affected, while involvement of the nonepiphyseal portions is very rare. Few case reports have been published with involvement of the anterior middle part of the rib by GCT [4–8]. The studied tumors were generally large with exophytic soft tissue component, causing a palpable lump or compressing and displacing adjacent organs (lung, liver, and breast). On radiographs, GCT of the rib presents as a lytic lesion that may be eccentric and has well-defined, nonsclerotic margins. The lesion causes cortical thinning or even breakthrough and bone expansion [9]. CT clearly demonstrates the osseous lysis caused by the tumor. Matrix calcification is rare. Nevertheless, peripheral calcifications, internal septa (which can also be calcified), and cystic components have been described [4–7]. Disruption of the cortex and extension in the soft tissues can also be appreciated. MRI accurately delineates the tumor, demonstrates the involvement of the adjacent structures, and is helpful for the surgical planning. On the other hand, the MRI features of GCT are not specific. Signal intensity is usually low or intermediate on T1W sequences and high on T2W sequences [9]. Inhomogeneous appearance is common, with signal voids (due to calcifications, hemosiderin, or vascular channels) and intensities indicative of hemorrhage at various stages [4, 7, 9]. Fluid-fluid levels are less common than in aneurysmal bone cyst [9] . The number of GCTs of the ribs imaged with MRI is limited. Most of them are larger lesions with a more inhomogeneous appearance due to degeneration and haemorrhage. On bone scintigraphy, GCT is usually associated with markedly increased radionuclide activity and with a diffuse or “doughnut” pattern. These findings cannot facilitate either detection or characterization of GCT [10]. On FDG-PET, and contrary to the majority of benign bone tumors, GCT is associated with a high standardized uptake value (SUV), which does not differ significantly from the corresponding value of osteosarcoma [11]. Serum acid phosphatase has been found to be increased in many cases of GCTs. It was therefore suggested that serum acid phosphatase could be used as a “tumor marker” for GCT and for monitoring treatment response and disease recurrence. It was also demonstrated that the level of this enzyme is correlated with the size of GCT [14]. In our case, serum acid phosphatase was normal preoperatively and remained at the same level postoperatively and during follow-up.
Conclusions
The remarkable features in our case of GCT are (a) The unusual location of the lesion arising from the costovertebral junction (b) Tumor mimicking a schwannoma and performing an en bloc resection of the tumor using a transthoracic approach (combined anterior and posterior approach single stage) and resection of the affected ribs and stabilization of the spine with instrumentation. Despite the multimodality imaging approach, the findings in this case of GCT were atypical and could not establish a preoperative diagnosis. Although remote, the possibility of a giant cell tumor may be included in the differential diagnosis when a well-defined lytic lesion involving the costovertebral junction is reported as a spindle cell tumor on CT guided biopsy.
Clinical Message
A detailed clinical assessment and meticulous preoperative planning help in enbloc excision of GCT of spine, reduction of the retro-fragments and prevention of recurrence.
References
1. Jeffreys TE. Synovial chondromatosis. J Bone Joint Surg 1967;3:530-534.
2. Miligram JW. Synovial osteochondromatosis. J Bone Joint Surg 1977;59(A):792.
3. Yu GV, Zema RL, Johnson RWS. Synovial Osteochondromatosis. A case report and review of the literature. J Am Podiatr Med Assoc Journal 2002;92:247-54.
4. Von Schroeder HP, Axelrod TS. Synovial osteochondromatosis of the distal radio-ulnar joint. J Hand Surg(Br).1996;21(1):30-2.
5. Batheja NO, Wang BY, Springfield D, Hermann G, Lee G, Burstein DE, Klein MJ. Fine-needle aspiration diagnosis of synovial chondromatosis of the tibiofibular joint. Ann DiagnPathol 2000;4(2):77-80.
6. Bryan AW, Dean-Yar T, Christina MW. Metacarpophalangeal joint synovial osteochondromatosis: A case report. Iowa Orthop J 2008;28:91–93.
7. Taglialavoro G, Moro S, Stecco C, Pennelli N. Bilateral synovial chondromatosis of the first metatarsophalangeal joint: A case report. Reumatismo 2003;55(4):263-6.
8.Felbel J, Gresser U, Lohmoller G, Zollner NFamilial chondromatosis combined with dwarfism. Hum Genet 1992;88:351–354.
9. Boya H, Pinar H, Ozcan O. Synovial osteochondromatosis of the suprapatellar bursa with an imperforate suprapatellarplica.Arthroscopy 2002;18(4):E17.
10. Paraschau S, Anastasopoulos H, Flegas P, Karanikolas A. Synovial chondromatosis: A case report of 9 patients. E E X O T 2008;59(3):165-9.
11. Kawasaki T, Imanaka T, Matsusue Y. Synovial osteochondromatosis in bilateral subacromialbursae. Rheumatol 2003;13:367-70
12. Carey RP. Synovial chondromatosis of the knee in childhood. A report of two cases. J Bone Joint Surg Br 1983;65(4):444-7.
13. Kistler W. Synovial chondromatosis of the knee joint: a rarity during childhood. Eur J PediatrSurg 1991;1(4):237-9.
14. Ogilvie-Harris DJ, Saleh K. Generalized synovial chondromatosis of the knee: A comparison of removal of the loose bodies alone with arthroscopic synovectomy. Arthroscopy 1994; 10(2):166-70.
15. Valmassy R, Ferguson H. Synovial Osteochondromatosis: A brief review. J Am Podiatr Med Assoc 1992;82:427-31.
16. Heather S, Paula S, Andrew B, Tania P. A case report of bilateral synovial chondromatosis of the ankle. Chiropractic & Osteopathy 2007;15:18.
| How to Cite This Article: Upadhyaya M, Kale S, Chaudhary P, Dhar S. Giant Cell Tumor Presenting as A Spindle Shaped Tumor Arising From the Costovertebral Junction at D7,d8,d9 Levels. Journal of Orthopaedic Case Reports 2016 Jan-Mar;6(1): 20-22. Available from: https://www.jocr.co.in/wp/2016/01/02/2250-0685-367-fulltext/ |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com