[box type=”bio”] What to Learn from this Article?[/box]
Failed osteosynthesis after fracture patella is a difficult situation. A modified Ilizarov technique is discussed here.
Case Report | Volume 6 | Issue 1 | JOCR Jan-Mar 2016 | Page 29-32 | Mukesh Tiwari, Hemant Chaturvedi, Vaibhav Patel, Rajarshi Matti DOI: 10.13107/jocr.2250-0685.370
Authors: Mukesh Tiwari[1], Hemant Chaturvedi[1], Vaibhav Patel[1], Rajarshi Matti[1]
[1] Department of Orthopaedics, National Institute of Medical Sciences Medical college & Hospital 21/10,Madhyam Marg, Mansarovar, Jaipur, Rajsthan-302020. India.
Address of Correspondence
Dr. Hemant Chaturvedi,
Department of Orthopaedics, National Institute of Medical Sciences Medical college & Hospital 21/10,Madhyam Marg, Mansarovar, Jaipur, Rajsthan-302020. India. Email : chaturvedi.hemant26@gmail.com
Abstract
Introduction: Tumors of the medial malleolus are rare. Chondrogenic tumors of the medial malleolus are extremely rare. Chondroblastoma of the medial malleolus has not been reported previously in the English literature. The purpose is to present a rare tumor occurring at an unusual site and its successful management.
Case Presentation: We report a case of a 30 year old female with Chondroblastoma of the medial malleolus with its clinical features, radiographic features, differential diagnosis, and management at this unusual site. Treatment comprised of open biopsy followed by aggressive curettage, phenolization and bone cement. Symptoms resolved after treatment with resumption of normal activities and no signs of recurrence on 1 year follow-up.
Conclusion: This case appears to be the first reported case of chondroblastoma occurring at medial malleolus. This case report will increase the awareness of this rare tumor occurring at this unusual site thereby avoiding any chance of misdiagnosis.
Key Words: Chondroblastoma, Medial Malleolus, Tumor.
Introduction
Tumors of the medial malleolus are rare. Chondrogenic tumors of the medial malleolus are extremely rare. Chondroblastoma represents about 1% of all primary bone tumors. It is more common in males, with a male: female ratio of 2:1 and most common site is the epiphysis of long bones with proximal humerus and proximal tibia being most common sites [1-2]. Malignant transformation has been described in only a few cases. Most chondroblastomas occur during active epiphyseal plate growth, and about two-thirds in the second decade of life [3]. Most common symptoms are localized pain & swelling.
Radiographic signs of asymmetric epiphyseal destruction with bone expansion and sclerotic margins are seen. In histopathology, the predominant cells are similar to epiphyseal chondrocytes with distinct morphological features of differentiation.
To our knowledge, chondroblastoma of the medial malleolus has not been reported previously in the English literature. The purpose is to present a rare tumor occurring at an unusual site and its successful management.
Case Report
A 30 year old female, presented in the hospital OPD on 28th March, 2013 with complain of pain and swelling localized in left medial malleolus since 12 years. Pain was gradual in onset, intermittent and aggravated on walking and relieved on rest and analgesic medications. Patient was able to walk normally without limp. Patient had history of trauma to the left ankle about 12 years back. Patient had no history of fever, significant weight loss or any significant medical history. She was admitted for the evaluation and management of her complains.
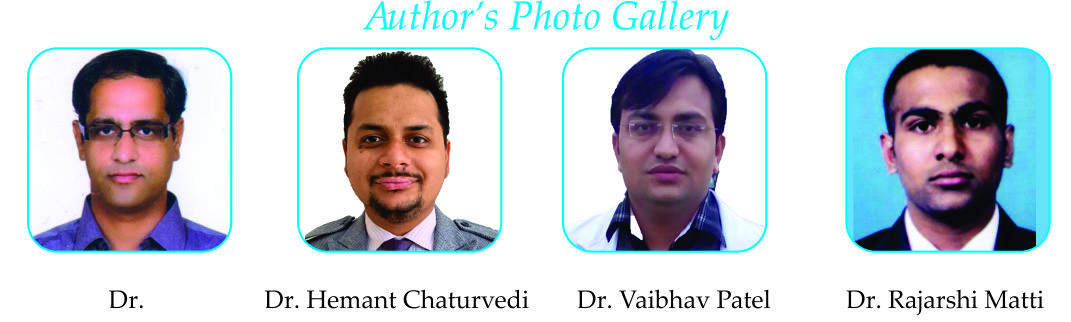
On physical evaluation, tenderness was present on left medial malleolus with a firm 3×3 cm localized swelling (Fig. 1) and normal temperature of the overlying skin. Swelling was non-compressible and non-reducible. Range of movements at left ankle joint were normal and pain free, in all planes. There were no lymphadenopathy and systemic examination was normal. The laboratory findings were within normal ranges.
Skiagrams of the left ankle with lateral (Fig. 2A) and anteroposterior (Fig. 2B) views were done. A well defined lytic lesion, spherical in shape (approximately 2 cm in diameter), was seen in the left medial malleolus. The lesion was non-expansile and eccentric without any periosteal reaction and cortex breech. Chest X-ray was also done and was normal.
MRI (Magnetic resonance imaging) of the left ankle was done. Serial T1 & T2 axial and T1 saggital, coronal scans were obtained using phased array coil. MRI (Figs. 3A and 3B) showed intramedullary lobulated cystic lesion in the medial malleolus which was subarticular without the involvement of articular surface of tibia. It was surrounded by hyperintense edema with no expansion of bone. There was no breech in the overlying cortex with no periosteal reaction or extension in the surrounding soft tissue. The articular margins of tibia were intact with no evidence of involvement of the ankle joint/talar surface giving an impression of a benign bone lesion, most likely to be chondroblastoma of left medial malleolus. Based on clinical study and radiological data, the differential diagnosis included chondroblastoma, giant cell tumor or chondromyxoid fibroma.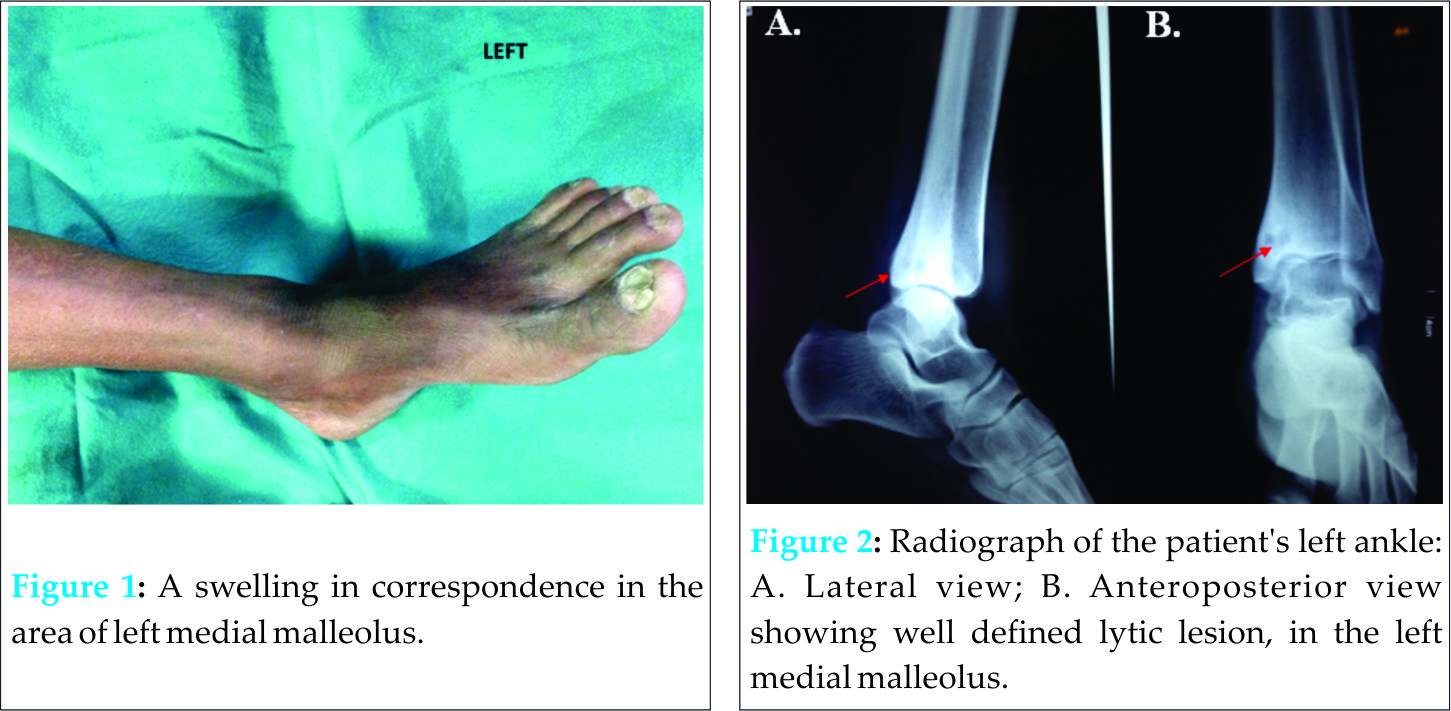
Core biopsy with Jamshedi needle was performed, which showed (Figs. 4A&B) numerous polygonal cells closely packed in sheets with rounded nuclei and abundant acidophilic cytoplasm. Large number of giant cells were scattered in between the polygonal cells. In between these cells, scanty chondroid matrix was seen. A diagnosis of Chondroblastoma was made.
Patient was then taken up for surgery under spinal anaesthesia and curettage and phenolization with bone cementing was done and curette material sent for biopsy and confirming the diagnosis. Follow-up of the patient was done at 6 weeks, 3 months, 6 months and 9 months and 1 year following the curettage. Pain and swelling at the left medial malleolus resolved and range of movements at ankle joint were normal and no signs of recurrence were seen on radiology after 1 year of follow-up.
Discussion
Chondroblastoma is a rare tumor. It occurs in the second decade of life in upto 95% of cases, with a male: female ratio of 2:1 [4]. Chondroblastoma has a predilection for the epiphysis or apophysis of the distal femur, proximal humerus, proximal tibia. 10% of chondroblastomas affect the small bones of the hands and feet with talus and calcaneum being the most common sites [5,6]. This paper presents, a case of chondroblastoma of the medial malleolus. The successful treatment comprised of aggressive curettage, phenolization, and bone cementation.
Pain and localized swelling, usually of several months duration are the main and presenting complaints in patients with chondroblastoma [7] as was also seen in this patient. Joint effusion is seen in approximately one-third of the patients [4] because of occurrence of the tumor in the vicinity of the joint, hence misdiagnosing it as an inflammatory joint disease. Atalar et al. [2] reported a case, which was misdiagnosed initially with a juvenile rheumatoid arthritis, and was administered anti-inflammatory therapy for 1 year before being diagnosed correctly. This patient also has 12 years of interval between initial symptom of pain and swelling to suspicion and confirmed diagnosis of chondroblastoma, thereby supporting the opinion that this form of bone tumor is frequently misdiagnosed [2].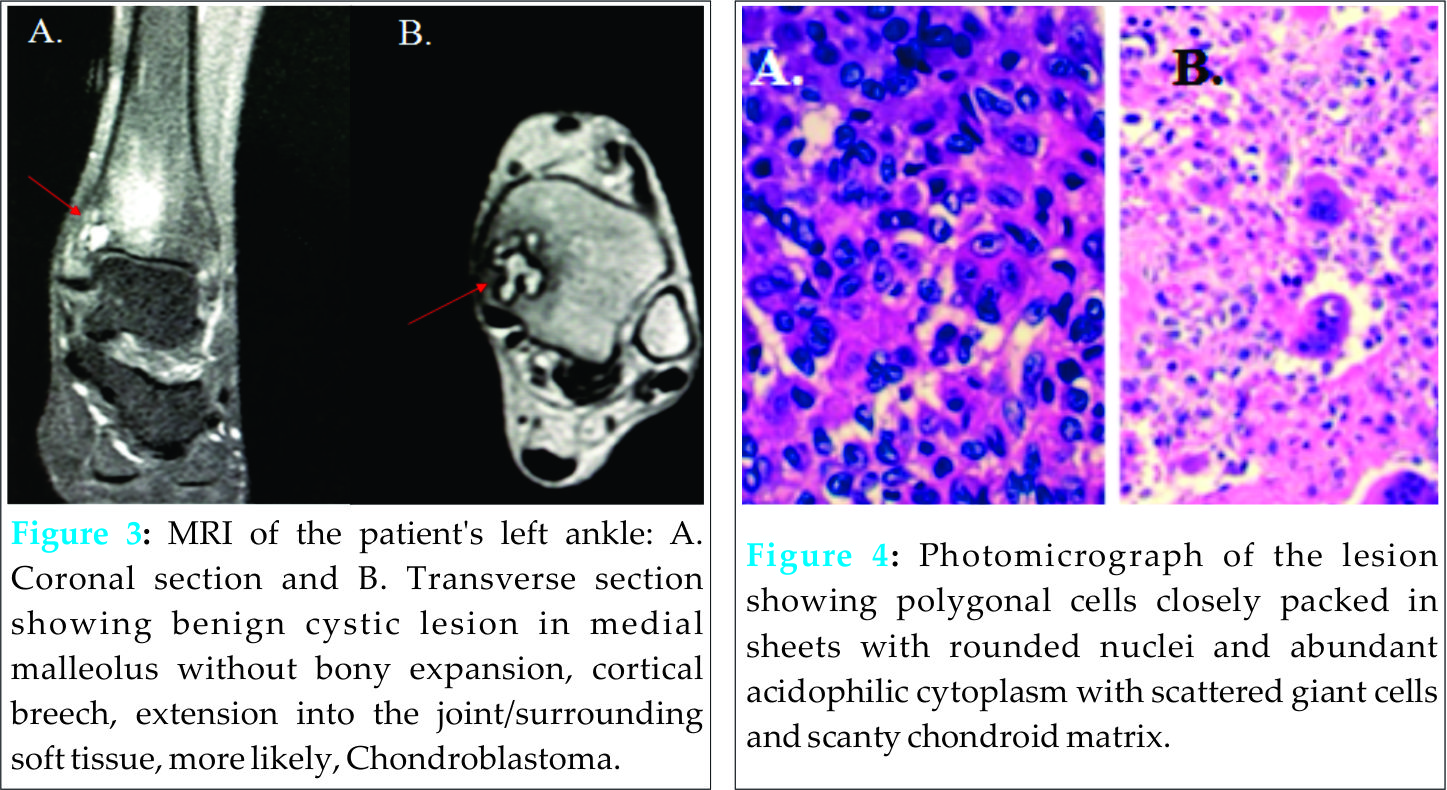
On radiological examination, the lesion is usually eccentrically located [8], well defined, lytic, radiolucent, with a thin sclerotic border, exhibiting a geographical pattern of bone destruction. [9] Cortical expansion and periosteal reaction can be seen which is uncommon in benign bone tumors. Annual chest X-Rays must be done for 5 years after treatment, for pulmonary metastasis, which is seen in 1 to 3% of patients. [1]
Chondroblastoma exhibit a distinctive feature on MRI scans which is a predominant low-to-intermediate signal intensity on T1-weighted images with heterogeneous intermediate signal on T2-weighted images, with only scattered foci of high signal intensity [10]. Focal lobules of low, intermediate, and high signal intensity most likely correspond to calcification, chondroid matrix, and fluid in the lesion. MRI can reveal a extension of tumor into the soft tissues which is usually rare and may also reveal an effusion of the joint.
The histopathological examination of chondroblastoma lesion, described according to the World Health Organisation [11] is “a relatively benign tumor, which is characterised by highly cellular and relatively undifferentiated chondroblast-like cells which are rounded or polygonal with distinct outlines and multi-nucleated osteoclast-type giant cells arranged singly or in groups.” Cartilaginous intercellular matrix with areas of focal calcification is typical-Chicken wire calcification. Biopsy of the lesion is mandatory to confirm the diagnosis.
As far as differential diagnosis of chondroblastoma is concerned, conditions mimicking chondroblastoma radiologically include bone abscess, giant cell tumor, chondromyxoid fibroma, osteoblastoma, enchondroma, intraosseous ganglion, clear cell chondrosarcoma, osteonecrosis while conditions mimicking chondroblastoma pathologically include giant cell tumor, enchondroma, clear cell chondrosarcoma and conventional chondrosarcoma. More clearly demarcated margins of the lesion on radiography and presence of chondroblasts and hyaline matrix on histopathological examination in this patient, excluded osteoclastoma as diagnosis. Epiphysis is a rare site for osteoblastoma and enchondroma, thereby excluding both. Younger age of this patient at the time of onset of symptoms, excludes clear cell chondrosarcoma as diagnosis which commonly affects middle aged patients. Young age of the patient at the time of onset of symptoms with location in proximity to the articular surface rules out the diagnosis of intraosseous ganglion. Absence of the classical radiological signs of osteonecrosis like crescent sign and typical MRI findings in this patient excludes osteonecrosis. Absence of the myxoid component on histopathological examination rules out chondromyxoid fibroma.
A standard curettage procedure combined with cryosurgery is associated with least recurrence rate. Various other surgical techniques, including open and endoscopic curettage, marginal resection, curettage with fat implantation, resection with radiofrequency ablation, and osteochondral autograft transfer are available now a days [12-14]. Reconstruction of bone defect as a result of surgery is another important question, which can be done with bone cement, and bone grafts. The most common method for reconstruction after curettage is bone autograft harvested from either iliac crest or fibula with advantages of improved rate of graft incorporation and lack of immunogenic concerns [2].
Advantages of bone cement for reconstruction of bone defect includes immediate weight-bearing without risk of fracture, and an improved clinical and radiographic follow-up which is observed in this patient also. Also, the bone graft is associated with longer surgical time, donor morbidity and may resorb, thereby making it difficult for differentiation of the graft from a tumor recurrence [15].
Conclusion
This case appears to be the first reported case of chondroblastoma occurring at the medial malleolus. This case report will increase the awareness of this rare tumor occurring at unusual site thereby avoiding any chance of misdiagnosis. Aggressive curettage, phenolization and bone cement are preferred treatment methods. In this case, successful treatment consisted of an open biopsy followed by curettage, phenolization, and bone cement without any recurrence at 1 year follow-up.
Clinical Message
Though medial malleolus is an extremely rare site for an uncommon tumor as Chondroblastoma, it should be considered as an important differential diagnosis for a swelling occurring at the medial malleolus, thereby avoiding any chance of misdiagnosis and should be managed promptly by a thorough clinical and radiological examination and confirmation of the lesion by an open biopsy followed by curettage, phenolization, and bone cement for successful outcomes.
References
1. Kyriakos M, Land VJ, Penning HL, Parker SG: Metastatic chondroblastoma. Report of a fatal case with a review of the literature on atypical, aggressive, and malignant chondroblastoma. Cancer 1985, 55:1770–1789.
2. Atalar H, Basarir K, Yildiz Y, Erekul S, Saglik Y: Management of chondroblastoma: retrospective review of 28 patients. J Orthop Sci 2007, 12:334–340
3. Huvos A. G., Marcove R. C. Chondroblastoma of bone. A critical review. Clin. Orthop., 1973, 95, 300-302.
4. Schajowicz, Gallardo H. Epiphysial chondroblastoma of bone. A clinico-pathological study of sixty-nine cases. J Bone Joint Surg Br. 1970; 52:205-226
5. Davila JA, Amrami KK, Sundaram M, et al. Chondroblastoma of the hands and feet. Skeletal Radiol 2004;33:582–587
6. Kricun ME, Kricun R, Haskin ME. Chondroblastoma of the calcaneus: radiographic features with emphasis on location. Am J Roentgenol 1977;128:613–616.
7. Erickson JK, Rosenthal DI, Zaleske DJ, et al. Primary treatment of chondroblastoma with percutaneous radiofrequency heat ablation: report of three cases. Radiology 2001;221: 463–468.
8. Plum GE, Pugh DG. Roentgenologic aspects of benign chondroblastoma of bone. Am J Roentgenol 1958;79:584–591.
9. Hudson TM, Hawkins IF Jr. Radiological evaluation of chondroblastoma. Radiology 1981;139:1–10.
10. Jee, Park YK, McCauley TR, Choi KH, Ryu KN, Suh JS,Suh KJ, Cho JH, Lee JH, Park JM, Lee YS, Ok IY, KimJM. Chondroblastoma: MR characteristics with pathologic correlation. J Comput.Assist.Tomogr. 1999; 23:721-726
11. Fletcher CDM, Unni KK, Mertens F. Pathology and genetics of tumors of soft tissue and bone. Oxford: IARC Press, 2002.
12. Lin PP, Thenappan A, Deavers MT, Lewis VO, Yasko AW: Treatment and prognosis of chondroblastoma. Clin Orthop Relat Res 2005, 438:103–109.
13. Anderson AF, Ramsey JR: Chondroblastoma of the talus treated with osteochondral autograft transfer from the lateral femoral condyle. Foot Ankle Int, 2003, 24:283–287.
14. Sterling G, Wilson A: Chondroblastoma of the talus: a case report.J Foot Ankle Surg, 2002, 41:178–182
15. Sessions W, Siegel H, Thomas J, Pitt M, Saidalnaief N, Casillasjr M: Chondroblastoma with associated aneurysmal bone cyst of the cuboid.J Foot Ankle Surg, 2005, 44:64–67.
| How to Cite This Article: Tiwari M, Chaturvedi H, Patel V, Matti R. Chondroblastoma of the Medial Malleolus: A Case Report of A Rare Tumor at an Extremely Uncommon Site. Journal of Orthopaedic Case Reports 2016 Jan-Mar;6(1): 29-32. Available from: https://www.jocr.co.in/wp/2016/01/02/2250-0685-370-fulltext/ |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com