[box type=”bio”] What to Learn from this Article?[/box]
Patellar dislocations are not an uncommon occurrence, however difficulty in their reduction should alert clinicians to the possibility of patella vertical axis rotation. In this scenario, multiple attempts at closed reduction should be minimized and open reduction may be the only safe option of management.
Case Report | Volume 6 | Issue 1 | JOCR Jan-Mar 2016 | Page 58-60 | Andrew Higgins, Mahdi Yacine Khalfaoui DOI: 10.13107/jocr.2250-0685.378
Authors: Andrew Higgins[1], Mahdi Yacine Khalfaoui[1]
[1] Department of Trauma & Orthopaedics, Central Manchester Teaching Hospitals.
Address of Correspondence
Dr. Mahdi Y Khalfaoui,
Department of Trauma & Orthopaedics, Trafford general hospital, Moorside Road, Davyhulme, Manchester M41 5SL. Email: mahdikhalfaoui@nhs.net
Abstract
Introduction: Acute patellar dislocation is a common injury usually associated with a significant traumatic mechanism resulting in lateral displacement. Vertical axis rotation following dislocation is a rare variant of this type of injury and can prevent closed reduction in the acute setting.
Case Presentation: A 32-year old gentleman presented with an irreducible patella dislocation following an unusual atraumatic mechanism. Following attempts at closed reduction under sedation and regional nerve block, eventual open reduction and soft tissue reconstruction was required under general anesthetic. During the open reduction procedure, it was noted that the patella had dislocated into a lateral extra-articular position and rotated around its vertical axis. Following patella reduction, the medial patellar retinaculum was repaired. Examination under anesthetic revealed satisfactory tracking of patella following repair.
Conclusion: A review of the literature suggests dislocations such as the current presentation, are extremely rare and although have been described to occur with minor trauma, have never been described to occur following a largely atraumatic event. In such cases, closed reduction may be impossible even with adequate analgesia due to patella position and soft tissue obstruction. Open reduction is essential in these situations.
Keywords: Patellar dislocation, vertical axis rotation, Patellar Reduction.
Introduction
Acute patellar dislocation is defined as the abrupt disruption in the relationship of the patella within the femoral groove. Patellar dislocation is a relatively common occurrence and is usually managed in the emergency department with closed manipulation under sedation. Reduction of acute patella dislocation seldom requires reduction under general anesthesia or open reduction. However, when the patella itself rotates around its vertical axis during dislocation, surgical intervention is usually required. We report such a case of an atraumatic patellar dislocation with vertical axis rotation.
Case Report
A 32-year old gentleman was admitted to our trauma department with a painful, immobile right knee. He sustained the injury externally rotating his knee whilst in “slight flexion” while he was moving from the driver’s seat to the passenger’s seat of his car. He had a history of two previous lateral patellar dislocations on the same knee. The first event was 15 years prior, when his knee twisted in flexed position while pushing a car. He was taken to the emergency department where it was successfully reduced under sedation. The second event was four years prior, when he sustained an injury while pushing a van, this time with the right knee fully extended. On this occasion, his patella spontaneously reduced and he did not seek any medical intervention. Our patient had no other significant past medical or surgical history and explained his right knee was completely asymptomatic prior to this current event.
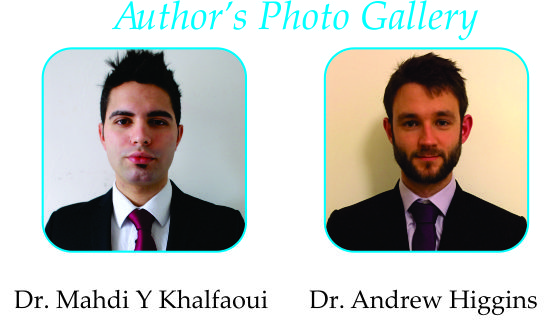
On examination, there was an obvious deformity suggesting lateral displacement of the patella with a sulcus in the skin evident over the femoral groove. Furthermore, the knee was held fixed in 15 degrees of flexion. Due to patient positioning difficulties we were unable to obtain true AP and lateral views on X-ray. The radiographs demonstrated a laterally displaced and a mal-rotated patella in the vertical plane (see Figs. 1 and 2). A manipulation under sedation was attempted unsuccessfully. A further attempt of reduction under a femoral nerve block had again been unsuccessful. 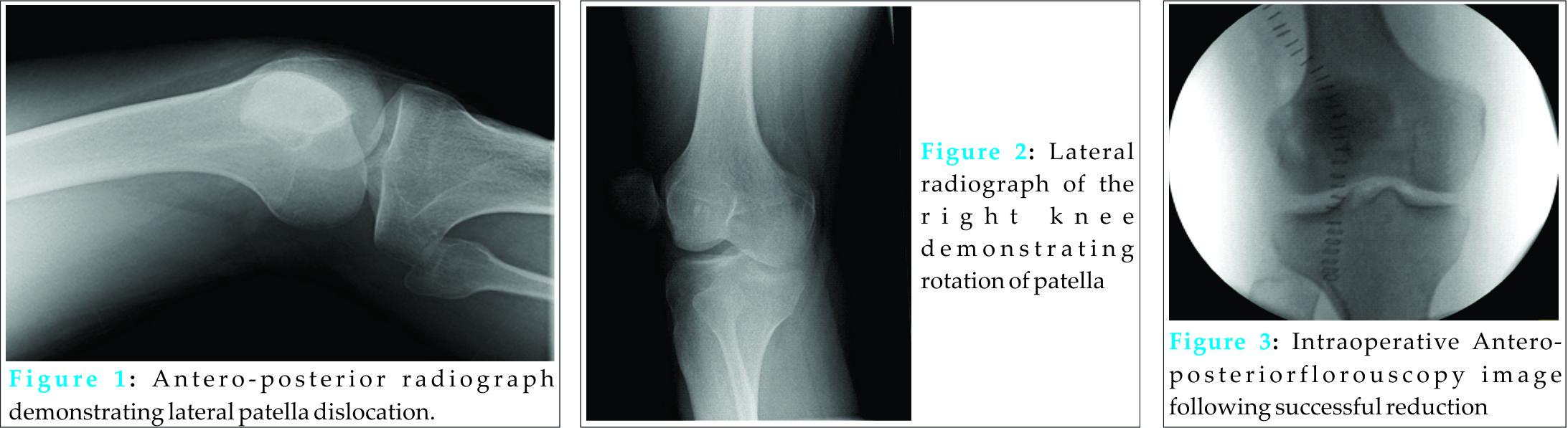
Our patient was subsequently taken to theatre where one final attempt of closed reduction was carried out under general anaesthetic and muscle relaxation. Ultimately, this failed and an open reduction was performed. The patient was positioned supine and an anterior midline skin incision was used. Complete rupture of the medial patellofemoral ligament (MPFL) was identified with the patella situated lateral to the lateral femoral condyle, everted by approximately 100 degrees. There were no visible deficiencies of the femoral condyles or the patellar articular surface. The patella was carefully reduced by direct manipulation. Following manipulation, the knee joint was washed out with normal saline and the medial patella retinaculum was repaired. After the repair, patella tracking was satisfactory with full range of flexion and extension.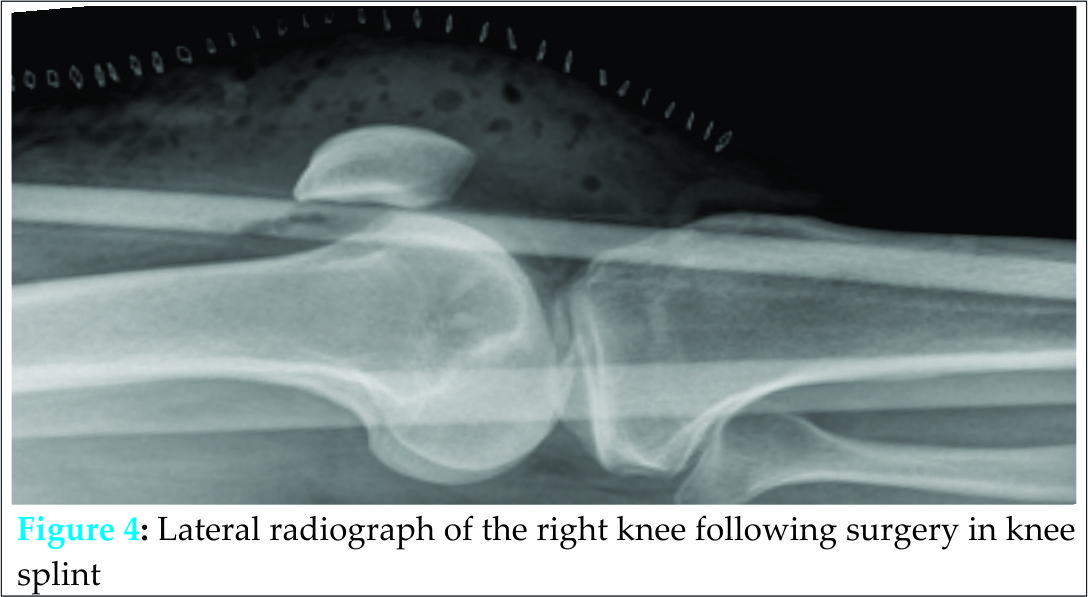
Post-operative radiographs confirm the patella in a satisfactory position in the antero-posterior and lateral planes (see Figs. 3 and 4). The patient was placed in an extension splint for comfort purposes immediately post-operatively. No weight bearing restrictions were applied. Early mobilization was encouraged after 5 days and the patient was referred for early physiotherapy. At 3 months follow-up, our patient had no further episodes of dislocation, full range of knee extension and flexion, and normal patella tracking. A hypermobility assessment at this stage revealed a Beighton score of 2 with extension beyond 10 degrees of both elbows only.
Discussion
Patellar dislocations can vary widely in their pattern of presentation however vertical axis rotation complicates only a small number of these cases. In 1844, Cooper described the earliest case of patellar dislocation with vertical axis rotation [1]. Since then, only a handful of case reports describing vertical axis rotation of the patella have been published with the majority describing the location of the patella within the femoral trochlea (intra-articular) [2-11]. Our case is rare as our patient had a less common variant of extra-articular patellar dislocation complicated by vertical axis rotation and by the fact, that the causative mechanism was largely atraumatic.
Previous descriptions postulate that the prominence of the lateral femoral condyle acts as a pivot point, which can cause the patella to rotate around on its vertical axis [11]. In this case, however, the patient denies any trauma, and instead describes externally rotating the leg whilst extended as the mechanism of injury. It is almost certain that the previous dislocations in our patient’s case had resulted in significant damage of the MPFL. With the patient reporting his injury taking place with the knee “slightly” flexed, the function of the MPFL in this case as the primary medial restraint during the first 20 degrees of flexion was likely to be inadequate. Previous authors have described similar cases of extra-articular lateral patellar dislocation with vertical axis rotation and have noted in their subsequent reviews of the limited literature that intra-aritcular dislocations were usually related to far more significant trauma than extra-articular dislocations [3-10]. This was also the finding in a previous report highlighting the relative minor force resulting in an extra-articular dislocation [4]. We feel this may be an indication of the chronic deficiency in the MPFL likely contributing to cases of extra-articular dislocation. On reviewing the previous cases of extra-articular dislocation in the literature, none had described a completely atraumatic mechanism and none had discussed previous dislocations or previous surgical history in their patients.
Detailed imaging can be difficult to obtain in the acute scenario; however in these cases CT imaging may clarify patella position and demonstrate mechanical engagement of the patella on the lateral femoral condyle. In one case report, CT imaging was utilized and confirmed avulsions of the vastusmedialis muscle and medial crus of the patella tendon with resultant impaction of the medial border on the patella onto the lateral femoral condyle [5]. In this case, imaging led to the decision for open reduction being required, minimizing further attempts at closed reduction which could in theory result in further damage.
It is difficult to be absolutely sure why attempts at closed reduction had failed in our particular case, but this is likely to be multifactorial. Vertical axis rotation results in impaction of the lateral edge of the patella on the lateral femoral epicondyle which may result in a corresponding femoral defect resulting in a lodging effect. Furthermore patient factors, namely obesity and large muscle mass around the knee made manipulation technically difficult in our case. Open reduction under general anaesthetic is rarely necessary for routine patellar dislocations however there are some obvious advantages. These include; the possibility of direct visualisation of the obvious damage to the soft tissue structures contributing to or resultant from the dislocation. In our case it was likely the MPFL had been damaged previously and repair is likely to help in restoring central patella tracking and overall stability. In this case, the patient was noted as having a shallow trochlea which might have accounted for his increased tendency to dislocations. Direct visual inspection may also help determine patients who are at risk of recurrent dislocations due to factors relating to their bony morphology and allow the surgeon to plan further management accordingly. Lastly, visualisation of the articulating surfaces allows the surgeon to identify and address any osteochondral defects and corresponding loose bodies which may otherwise have contributed to long term future problems requiring eventual surgical intervention.
Conclusion
From our experience with this case, difficulty in reducing a dislocated patella should alert surgeons to the possibility of an extra-articular dislocation with possible vertical axis rotation. In these scenarios, multiple attempts at reduction can be ineffective despite good tolerance from the patient. We were able to achieve adequate analgesia and sedation using local and regional anaesthesia, without successful reduction of the dislocation. Although some authors have demonstrated successful closed reduction with the use of local anaesthetic and muscle relaxants, this is not always effective. Furthermore, attempted closed reduction under general anaesthesia in our case was also unsuccessful, demonstrating how closed reduction can be futile in certain cases. We would recommend a low threshold for open reduction in such cases by a specialist knee surgeon who may assess and reconstruct damaged soft tissue damage in one operation minimizing future sequelae.
Clinical Message
Vertical axis rotation is a rare entity complicating patella dislocations. In this rare event, multiple failed reductions may be the only indicator of this complication. Radiographs in the acute setting can be difficult to obtain and interpret. Emergency physicians should be aware of this complication and refer to the relevant specialist for open reduction under general anaesthesia in order to minimize patient discomfort and potential articular surface damage.
References
1. Cooper A. A treatise on dislocations and fractures of the joints Lea & Febiger, Philadelphia. 1844; 178.
2. Corso SJ, Thal R and Forman D. Locked Patellar Dislocation With Vertical Axis Rotation: A Case Report. Clinical orthopaedics and related research 1992;279: 190-193.
3. Yang C, Gong Y, Wen X et al. Extra-articular patellar dislocation with vertical axis rotation. The Knee 2011;18(6):512-513.
4. Sherman SC & Yu A. Patellar dislocation with vertical axis rotation. Journal of Emergency Medicine 2004;26(2):219-220.
5. Hackl W, Benedetto KP, Fink C et al. Locked lateral patellar dislocation: a rare case of irreducible patellar dislocation requiring open reduction. Knee Surgery, Sports Traumatology, Arthroscopy 1999;7(6): 352-355.
6. Gidden DJ & Bell KM. An unusual case of irreducible intra-articular patellar dislocation with vertical axis rotation. Injury 1995;26(9):643-644.
7. Rollinson PD. Vertical intercondylar dislocation of the patella. Injury 1988;19(4): 281–282.
8. Alioto RJ &Kates S. Intra-articular vertical dislocation of the patella: a case report of an irreducible patellar dislocation and unique surgical technique. J Trauma 1994; 36(2):282–284
9. Singletary EM & Dobson J. Intercondylar dislocation of the patella with vertical axis rotation. Am J Emerg Med. 1999;17(1):76–77.
10. Gamble D, Otto Q, Carrothers AD et al. Patella Dislocation with Vertical Axis Rotation: The “Dorsal Fin” Patella. Case reports in orthopedics, 2015.
11. Meta M, Graham D, Tetsworth K. Irreducible lateral patella dislocation with associated rotation. Australia International Journal of Medicine and Medical Sciences. 2012;2(2): 065-068.
| How to Cite This Article: Khalfaoui MY, Higgins A. Khalfaoui MY, Higgins A. Atraumatic Extra-articular Patellar Dislocation With Vertical Axis Rotation: A Case Study. Journal of Orthopaedic Case Reports 2016 Jan-Mar;6(1): 58-60. Available from: https://www.jocr.co.in/wp/2016/01/02/2250-0685-378-fulltext/ |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com