[box type=”bio”] What to Learn from this Article?[/box]
Treatment of subtrochanteric fracture non unions using a proximal femur plate.
Case Report | Volume 6 | Issue 1 | JOCR Jan-Mar 2016 | Page 65-68 | Navin Balasubramanian, Ganesh Babu, Sindhuja Prakasam DOI: 10.13107/jocr.2250-0685.381
Authors: Navin Balasubramanian[1], Ganesh Babu[2], Sindhuja Prakasam[3]
[1] Department of Orthopaedics, Saveetha Medical College, Chennai. India.
[2] Department of Orthopaedics, Sri Ramachandra Medical College, Chennai. India.
[3] Department of Orthopaedics, Government Peripheral Hospital, Chennai. India.
Address of Correspondence
Dr. Navin Balasubramanian,
No 19, 21st Main Road,Anna Nagar, Chennai 600040. India. Email: drnavin_ortho@yahoo.co.in
Abstract
Introduction: Subtrochanteric fractures have a bimodal age distribution. They are mostly due to high violence trauma in the younger age group. They almost always require open reduction and internal fixation. Due to the increase in the emergence of native bone setters, these fractures are increasingly been managed by these spurious bone setters using native splints. As a result, non-union rate is high among such patients. These patients definitely need open reduction with internal fixation +/- bone grafting. The choice of implants used can be either a dynamic condylar screw plate (DCS) orproximal femoral nail (PFN).
Case series: Here we have used a surgical grade 316 L stainless steel proximal femoral anatomical locked compression plate (PF-LCP). We analyzed 13 patients with established non unions of subtrochanteric fractures treated in our centre by the use of the PF-LCP. There were 10 males and 3 females. The average age was 48.23 years. All our patients were followed up by serial radiographs at 6,12,18,24 weeks and thereafter at 6 months interval. Union was achieved in 11 out of 13 patients at 12 weeks whereas two patients had delayed union which eventually healed at 18 weeks and 24 weeks. The average Harris hip score at 1 year follow-up was excellent in eight, good in four and fair in one patient respectively.
Conclusion: We conclude that in complicated non-unions, the use of PF-LCP has a definite positive role in the management of such cases.
Key Words: Dynamic condylar screw(DCS ), Proximal femoral nail (PFN), Proximal femur LCP, Harris hip score.
Introduction
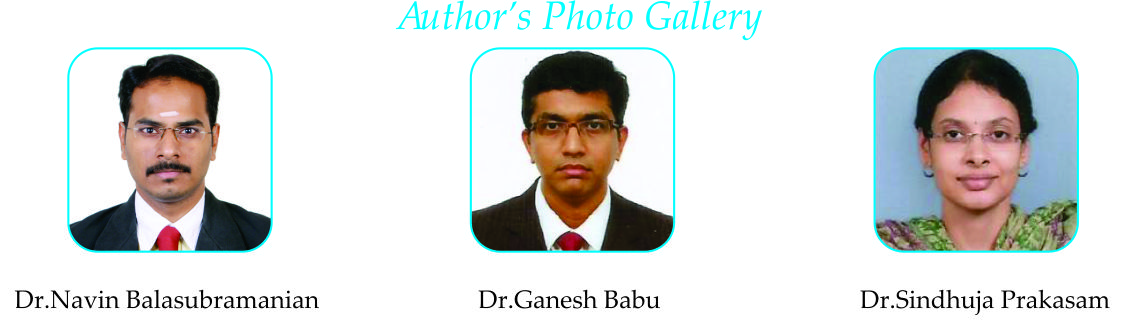
Peritrochanteric fractures include either inter-trochanteric or sub-trochanteric fractures. While inter-trochanteric malunite frequently, subtrochanteric fractures most often end in non-unions. The main reason for non-union is soft tissue interposition. The interposing soft tissues along with the displacement means that these fractures necessitate open reduction. Also to complicate matters, there has been a surge in the number of traditional bone setters who use native splints with massages. Hence, the frequency of non-union subtrochanteric fractures has increased in the recent past. The implant of choice has traditionally been either DCS plates or PFN. In our study we have used the PF-LCP [Fig 1.a & 1.b].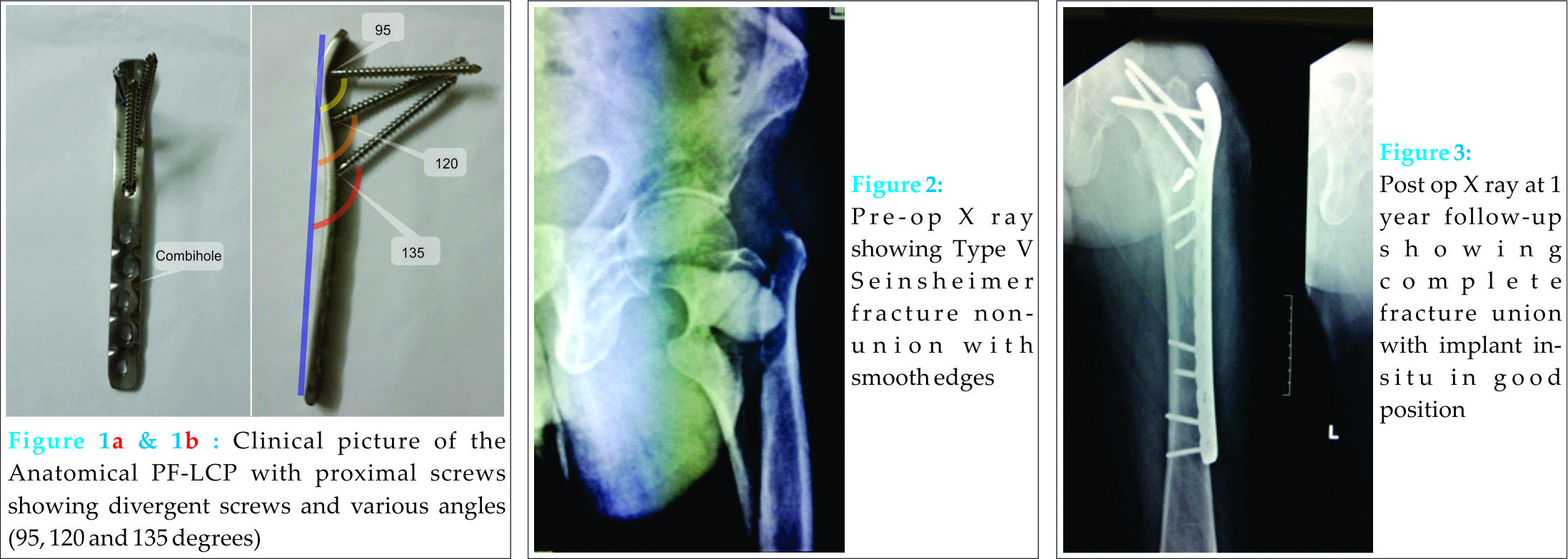
Case Report
We analyzed 19 consecutive patients with non-unions of subtrochanteric fractures who presented to our clinic. The study was conducted between 2009 to 2014. Six patients were lost to follow-up and were excluded from the study. We have included 13 patients in this study. There were 10 males and 3 females with an average age of 48.23 years. Informed consent was obtained prior to surgery in all of them. We used the Seinsheimer classification system to group patients (Table 1). The patients were operated on a fracture table with traction. The standard lateral approach was used. The length of the incision varied depending on the need for each case. All patients underwent open reduction with removal of interposing fibrous tissue, freshening of the edges and anatomical reduction. The PF-LCP was used with proximal 6.5 mm locking cancellous screws and distally using both cortical and locked screws. All surgeries were done under image intensifier. Primary bone grafting was done in two patients (Seinsheimer type IV ) i.e patients S. No. 2 and 12 [Table No. 2] to maintain poesteromedial cortical contact. Wound closure and suture removal done as per standard guidelines. All patients were started on non-weight bearing walking for 6 weeks. Then weight bearing was started as tolerated. Eleven out of 13 patients started full weight bearing by 12 weeks with 2 patients walking full weight bearing at 18 and 24 weeks respectively. The functional assessment was done using the modified Harris Hip Score and results were tabulated (Table 2). Serial radiographs were taken at 6,12,18,24 weeks follow-up and thereafter at 6 months interval.
Results
Eleven out of the 13 fractures united at 12 weeks follow-up. Two patients (Case no. 2 and 12) had delayed unions which healed eventually at 18 and 24 weeks respectively. They were both Type IV Seinsheimer fracture pattern with loss of posteromedial cortical contact. They were primarily grafted and this could be a possible reason for the delayed union. There was one patient who had one case of wound dehiscence which required secondary suturing under local anaesthesia (Case no.9). We did not have any patient with infection. There was no case of implant breakage or pull out. At one year follow-up, all our patients were ambulatory full weight bearing, walking without any aid and were doing well. The functional assessment showed excellent results in eight [Fig.2,3 & 4], good in four and fair in one patient respectively. We do not routinely advise or perform implant removals for any of our patients due to social and financial constraints.
Discussion
The conventional and preferred treatment of sub trochanteric fractures has been intra medullary devices. They are load sharing devices which allow early weight bearing walking. The earlier used proximal femoral side plates namely DCS and the newly introduced PF-LCP have their own advantages in select cases.
Shukla et al [1] reviewed 60 patients treated with IM nailing and reported a union rate of 95 %. They also reported a higher malunion and non-union rate in those patients treated by closed reduction than those treated by open reduction (3 and 1 in open versus 6 and 2 in closed reduction group). They also concluded that the complication rate was higher in those fractures fixed in Varus (> 10 degrees) at the fracture emphasizing that correct anatomical alignment is of paramount importance in achieving union. In our study, all our patients underwent open reduction and anatomical reduction was achieved in all our patients. Hence, we had a comparable union rate with no varus collapse or implant failure.
Bartonincek et al [2] used the double angled blade plate with valgus osteotomy in his series of 15 patients and achieved a union rate of 93.33% which is comparable to our study. One patient had an implant failure due to a repeat fall and required revision surgery. The average Harris hip score improved from 73 pre-operatively to 92 following surgery. In our study, the average Harris Hip score following union was 89 which is comparable. We did not have any patient with complaints of limb length discrepancy.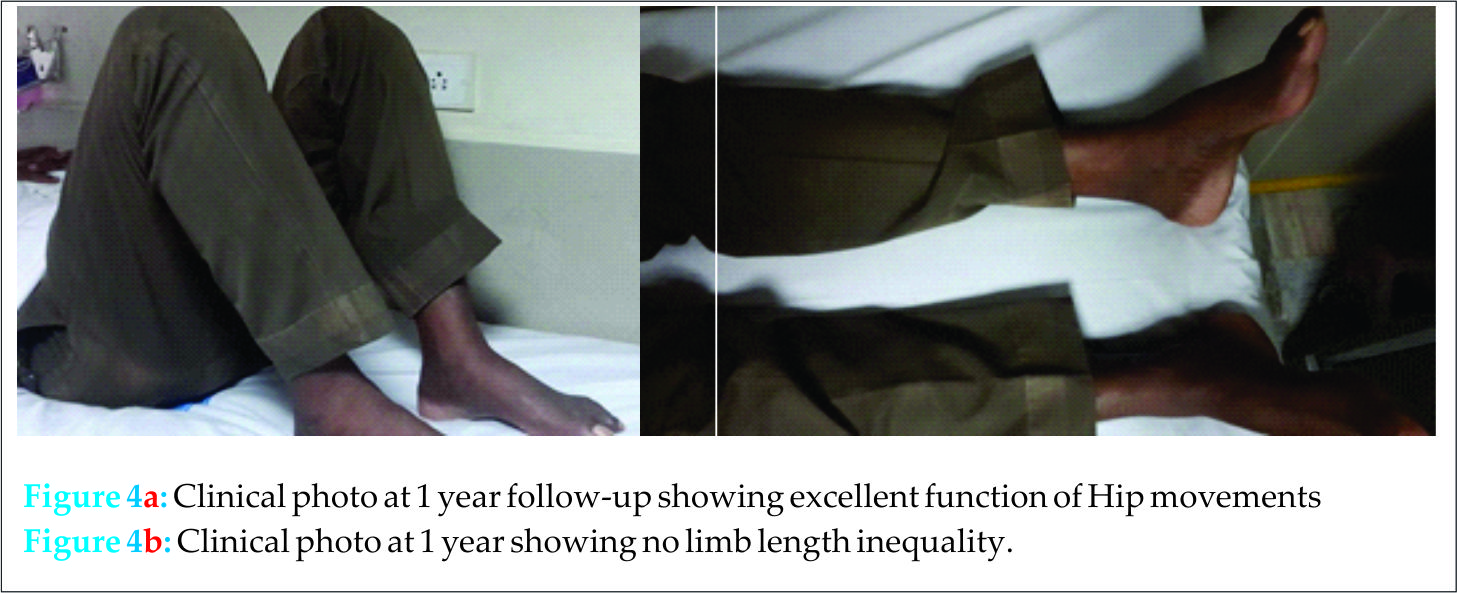
Pelet et al [3] compared gamma nail versus side plate and reported 100 % healing with gamma nail with 2 failures in the side plate group. They concluded that gamma nail allows early weight bearing walking. In our study however though we have used only anatomical PF-LCP and achieved comparable union rates. However weight bearing was delayed till about 12 weeks in 11 out of 13 patients (radiological union).
Liporace et al [4] reported a case report of using a femoral fixator distractor over a IM nail to achieve length in a patient with limb length discrepancy. In our study, we were able to restore limb length to within 0.5 cm of the opposite normal side in all our patients.
Giannoudis et al [5] reported a new “Diamond” concept of treating non union subtrochanteric fractures using local injection of growth factor (rhBMP-7), RIA (Reamer irrigator Aspirator) and mesenchymal growth factors (MSC). He concluded that in addition to the above, preventing varus malalignment at the fracture is the keystone to allow fracture healing and prevent implant failure.
Muller et al [6] reported a careful usage of additional circlage wiring to provide stability to the fracture site treated by IM nail. He however cautioned against the use in all patients. He reported a 90% reduction in failure of fracture fixation in his series. In our study, we ensured anatomical reduction along the posteromedial cortex was achieved to prevent varus collapse at the fracture leading to implant pull out.
Pugh et al [7] compared first generation nails to second generation nails and preliminary reports by them suggested a slight biomechanical advantage for the second generation nail over the first generation nails. In our study, we have obtained results which are comparable to the IM nail with fewer complications.
O’Malley et al [8] showed in 46 patients of unstable trochanteric fractures treated by intra medullary devices that there was on an average a 7 mm lateral shift of the distal femoral shaft (i.e “Wedge effect”). As a result all of those patients had a varus malignment (Neck –Shaft angle of 129 degrees versus 133 degree in the opposite normal hips) but the fracture eventually united. In our study, we ensured a near anatomical neck shaft angle and supported the postero-medial cortex with graft when required (Case no.2 & 12) to ensure that no varus collapse occurs.
Seyham et al [9] compared the outcomes of proximal fractures using PFNA and Intertan nails and concluded that the rate of proximal screw back-out and varus collapse was significantly higher in the PFNA than in the Intertan group. In our study, we did not report any varus collapse or implant pull out in any of our cases.
Niu et al [10] conducted a survey among AAOS members about the preferred choice of implant for proximal femur fractures. He concluded that although both Intramedullary devices and plate fixation devices produced equal results with regard to fracture healing, the implant of choice in the current scenario is the IM device due to ease of surgery and biomechanical stability over the plate devices. In our study however, we have shown that in select complicated cases, these newer PF-LCP have proved to be as efficient and stable as IM devices.
Muller et al [11] showed by a comparative study between PFN and DHS, a significantly higher rate of screw cut-out was seen in DHS group compared in the PFN group. The PF-LCP that we have used in our study has the advantage of having three locked screws in place of one DHS screw at 95,120 and 135 degrees to offer increased stability with a negligible cut out risk.
In our study, we did not include a control group treated by either a PFN or DHS implant. However, we compared our results with the results of other authors [3, 7 , 9 , 10] who used either PFN or DHS as the standard implant of choice for such fractures. The results in our study show promising outcomes in favour of the PF-LCP, but our study group is small (13 patients) and we need to have a bigger study group and include more patients.
Conclusion
Subtrochanteric fracture non unions are increasingly common in our day to day practice. Although the gold standard remains intramedullary devices for such fractures, we have concluded from our study that the Anatomical Proximal Femur Locked plates (PF-LCP) is able to provide comparable results with those of IM devices. The potential advantages of this implant over the other side plates are as follows:
Three locked screws in the proximal fragment at various angles namely 95, 120 and 135 degrees providing multi planar stability [Fig. 1 & Fig.2 ] No loss of bone as no reaming is done as with DCS screws Anatomical so no pre-contouring is required Provision of combi hole to use either locking or cortical screw to achieve plate to bone contact distally. Can be safely used with fracture extension into Greater Trochanter (entry point for nail). We therefore conclude that PF-LCP is a valuable tool in the arsenal of every orthopaedic surgeon. We believe that with the right patient selection, this implant provides a similar result and outcome to that offered by intramedullary devices.
Clinical Message
Sub-trochanteric non unions are not uncommon as was once reported. Although the conventional and current implant of choice is Intramedullary nailing (IM/IL nail) following open reduction, the use of the PF-LCP has produced results similar to those of IM nails. Hence, for the appropriate patient choice, the PF-LCP is a newer and proven implant to use for excellent outcomes.
References
1. Shukla S, Johnston P, Ahmad MA, Wynn-Jones H, Patel AD, Walton NP. Outcome for traumatic subtrochanteric femoral fractures fixed using cephalo-medullary nails. Injury2007;38(11): 1286-93.
2. Bartonicek J, Skala-Rosenbaum J, Dousa P. Valgus intertrochanteric osteotomy for malunion and nonunion of trochanteric fractures. J Orthop Trauma. 2003;17(9):606-12.
3. Pelet S, Arlettaz Y, Chevalley F. Osteosynthesis of per- and subtrochanteric fractures by blade plate versus gamma nail. A randomized prospective study. Swiss Surg. 2001;7(3):126-33
4. Liporace FA, Yoon RS. Fixator assisted femoral lengthening following intramedullary exchange nailing for subtrochanteric non-union. J Orthop Trauma. 2015; 9.
5. Giannoudis PV, Ahmad MA, Mineo GV,Tosounidis TI,Calori GM, Kanakaris NK. Subtrochanteric fracture non-unions with implant failure managed with the “Diamond” concept. Injury 2013;44(1):76-81.
6. Muller T, Topp T, Kuhne CA, Genhart G, Ruchholtz S, Zettl R. The benefit of wire circlage stbilisation of the medial hinge in intramedullary nailing for the treatment of sub trochanteric femoral fractures: a biomechanical study. Int Orthop. 2011;35(8):1237-43.
7. Pugh KJ, Morgan RA,Gorczyca JT, Pienkowski D. A mechanical comparison of subtrochanteric femur fracture fixation. J Orthop Trauma 1998;12(5):324-9.
8. O’Malley, Kang KK, Azer E, Siska PA, Farrell DJ,Tarkin IS. Wedge effect following intramedullary hip screw fixation of proximal femur fracture. Arch Orthop Trauma Surg. 2015.
9. Seyham M, Turkmen I, Unay K, Ozkut AT. DO PFNA devices and Intertan nails both have the same effects in the treatment of trochanteric fractures ? A prospective clinical study. J Orthop Sci. 2015.
10. Niu , Yang A, Harris AH, Bishop J. Which fixation device is preferred for surgical treatment of trochanteric hip fractures in the United States? A survey among Orthopaedic Surgeons. Clin Orthop Relat Res. 2015.
Muller F, Galler M, Zellner M, Bauml C, Fuchtmeier B. The fate of proximal femur fractures in the 10th decade of life. An analysis of 117 consecutive patients. Injury 2015 Jul
| How to Cite This Article: Balasubramanian N, Babu G, Prakasam S. Treatment of Non Unions of Subtrochanteric Fractures Using an Anatomical Proximal Femur Locked Compression Plate – A Prospective Study of 13 Patients. Journal of Orthopaedic Case Reports 2016 Jan-Mar;6(1): 65-68. Available from: https://www.jocr.co.in/wp/2016/01/02/2250-0685-381-fulltext/ |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com