[box type=”bio”] What to Learn from this Article?[/box]
Peri-prosthetic TB infection is uncommon especially in a patient with no known history of the disease.The atypical nature of the infection, means it can be easily missed. However, if diagnosed early the prognosis is considerably better, and the implants can be retained, sparing the patient of a major revision surgery.
Case Report | Volume 6 | Issue 1 | JOCR Jan-Mar 2016 | Page 23-25 | Tadros B.J, Stafford G H DOI: 10.13107/jocr.2250-0685.368
Authors: Tadros B.J[1], Stafford G.H[1]
[1]Department Of Orthopaedics, Elective Orthopaedic Centre, Epsom General Hospital, Dorking Road, Epsom, KT18 7EG, Surrey, UK.
Address of Correspondence
Dr. Baha John Tadros,
Junior Orthopaedic Fellow, Elective Orthopaedic Centre, Epsom General Hospital, Dorking Road, Epsom, KT18 7EG, Surrey, UK. Email: b_tadros@yahoo.com
Abstract
Introduction: Tuberculosis (TB) still remains a common problem in the UK and, with the increasing number of patients being offered arthroplasties; periprosthetic involvement is not uncommon anymore. However, the diagnosis of TB infected arthroplasties still remains difficult and misdiagnosis is common, therefore delaying treatment.
Case Report: We describe a 36-year old Caucasian female with no known history of TB who presented with hip pain thought to be due to femoro-acetabular impingement (FAI). In the course of 18 months, the patient had been investigated extensively; including steroid injection, hip arthroscopy (including synovial biopsies), and eventually a total hip arthroplasty. During arthroplasty, further extensive biopsies were performed which raised the suspicion of TB on histology. Further synovial biopsies obtained arthroscopically were microbiologically positive for TB (PCR). The patient was sent to an infectious disease specialist. It appeared that the patient had TB in the past, of which she was unaware.
Conclusion: We hypothesise that the immunosuppressant effects of the steroid injections she received reactivated her TB.
Keywords: Mycobacterium Tuberculosis, Arthroplasty, Steroids, Peri-prosthetic infection.
Introduction
Tuberculosis (TB) still remains a common problem in the UK, with an incidence of 12.3/100,000 in 2013 according to a government report [1]. Osteo-articular TB has been well documented, accounting for 35% of extra-pulmonary TB [2]. However, TB infecting joint arthroplasties is not common. Although, there are numerous case reports regarding this subject, but diagnosis remains a challenge for the surgeon, especially if the patient reports of no past history of the disease.
Case Report
A 36-year old Caucasian woman from New Zealand developed sudden- onset right groin and hip pain when she was at a music festival in June 2012. She also reported night pain and an inability to bear weight on that leg; examination revealed a globally tender hip and restricted range of motion. An MRI scan was performed which showed a very large joint effusion and intense bone marrow oedema within the central portion of the acetabulum. A stress fracture was suspected and a CT scan was done which showed a cortical defect correlating with the area of maximum bone marrow oedema. The patient was desperate to be out of pain so an ultrasound-guided steroid injection was given which gave her relief for a few weeks. She was reviewed again in January 2013; at this point the pain had come back and she was using crutches to mobilize. A further MRI was performed demonstrating persisting joint effusion, florid synovitis and an evident labral tear (Fig 1).
She was referred to an orthopaedic surgeon with a special interest in young adult hip pathology. On further questioning, she ascertained of a childhood history suggestive of developmental dysplasia and had worn a Pavlik-type splint as a baby. She was otherwise fit and healthy with insignificant medical history.
As a cause of the labral tear seen on MRI, she was suspected of having femoro-acetabular impingement (FAI) with a cam deformity seen on three-dimensional computerised tomography (CT). Given this and the fact that she had had a good, although temporary relief, following intra-articular hip injection, she was scheduled for a hip arthroscopy later that month.
A hip arthroscopy was performed in January 2013 and intra-operative findings included stigmata of FAI, but a florid synovitis. A labral debridement, synovial biopsy and partial synovectomy, excision of a cam impingement lesion were performed and the patient was discharged on the same day with no recorded complications (Fig 2).
The patient was seen 6 weeks after the procedure and reported an overall improvement in pain and mobility, but was still using crutches outdoors. The synovial biopsies were reported as showing marked acute and chronic villous inflammation with no specific evidence of infection. She was then offered another intra-articular steroid injection intra-articular steroid injection to help alleviate persisting pain so she may better perform her physiotherapy. This injection was given in March 2013.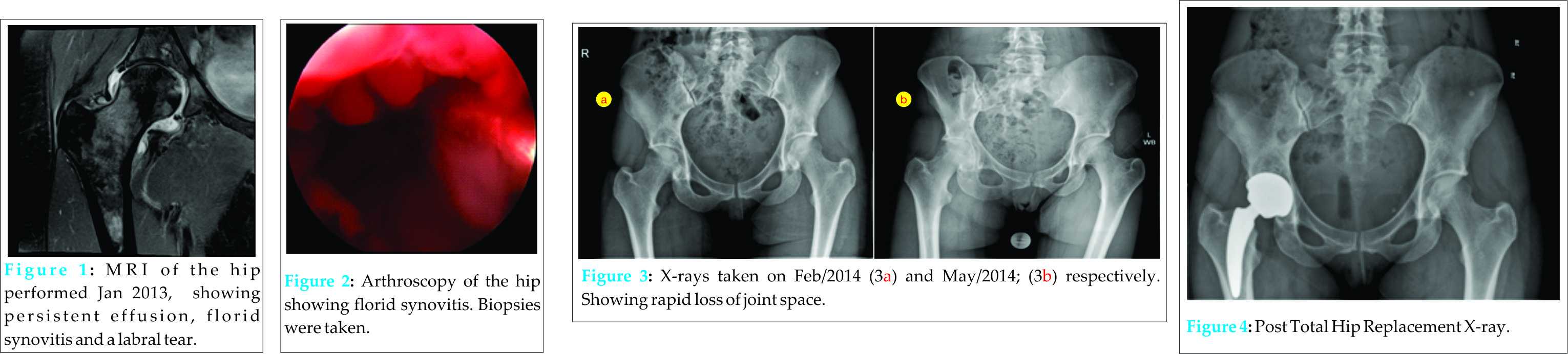
In July 2013 she was reviewed again. Her pain was not significantly better and so a repeat MRI scan was performed. This was reassuring from a labral perspective but showed persistent synovitis. She was therefore referred to a rheumatologist to exclude an inflammatory cause.
The rheumatologist arranged an inflammatory / extended immune screen for the patient and the results were as follows: ESR 9 mm/hr, CRP < 5mg/l, and negative for rheumatoid factor, ANA, anti-CCP, double stranded DN, and ENA series. That day she reported recent onset pleuritic chest pain so a chest X-ray and subsequent CT scan were arranged. The CT showed bilateral pulmonary nodules and LUL bronchogram, but nothing more specific. Bronchial washings revealed no necrosis or malignant cells present.
The decision was then made to aspirate the hip joint and perform a further course of steroid injection under ultrasound guidance; this was undertaken in February 2014. Pre-injection aspirates were sent to microbiology, results showed no pus cells and no growth, even on enrichment cultures.
The patient was then reviewed again in May 2014. She reported that she experienced three weeks of relief following the injection, but the pain had then deteriorated to a point that it had become unbearable. X-rays taken on the day showed significant deterioration of the hip joint with degenerative changes (Fig 3) (Initial and new X-rays). She was therefore offered a total hip replacement (THR) to alleviate her pain, which was performed, in June 2014 (MiniHip ceramic-on-ceramic) (Fig 4). Further synovial biopsies were taken intra-operatively and sent to histology as the surgeon still felt a high likelihood of inflammatory arthropathy.
The patient had an uneventful recovery, and was discharged on June 2014. Histology results showed a markedly thickened synovium with numerous granulomas, both caseating and non-caseating. Stains for fungi and acid-fast bacilli were negative but the appearance was suggestive of TB. She enjoyed an excellent recovery from her THR, delighted to be without pain for the first time in two years. However, the biopsy results were discussed and she was referred to an infectious diseases specialist with an interest in TB, who felt that this diagnosis should be proven prior to commencing treatment.
She, therefore, underwent a second hip arthroscopy with further biopsies synovial debridement and thorough washout three-months post THR. Thirty millilitres of light green, milky fluid was aspirated prior to the arthroscopy on which the four-week aspirate cultures were positive for TB. Polymerase Chain Reaction (PCR) performed on the synovial biopsies was also positive. She is currently being treated with implant-retaining anti-tuberculous therapy.
Discussion
The hip is the second most commonly affected bony site after the spine [3] by extra-pulmonary TB. It can mimic other pathologies, which was clear in our case report, leading to misdiagnosis and a delay in treatment [4].
Two patterns have been described in the literature regarding peri-prosthetic tuberculous infections with no previous history of TB, the first being diagnosed more than 6 weeks following arthroplasty and thought to be due to either a hematogenous spread from a distant focus or a reactivation of a locally dormant infection. The second pattern described is when the infection is first recognized at the time of arthroplasty [5]. Our patient falls under the second category. With regards as to what reactivated the infection, we can only presume it was the intra-articular steroid injections she received prior to her arthroplasty.
Systemic corticosteroid therapy is one of the major risk factors for TB [6], but TB affecting a native joint due to an intra-articular steroid injection is rare and has only been described a few times in the literature. [7, 8, 9, 10, 11]
Histological and microbiological examination of synovial fluid and tissue remains the mainstay for diagnosis of TB in joints, but it can take up to 8 weeks with a positive result provided in 50-80% of cases [12].
Acid-fast smears lack sensitivity and cannot distinguish M.tuberculosis from other mycobacteria, but in conjunction with PCR it can provide a rapid and specific identification of M. tuberculosis complex organisms [13].
Spinner et al have reported favourable outcomes with implant-retaining anti-tuberculous therapy if the infection is detected early [5].
Conclusion
We hypothesise that the immunosuppressant effects of the steroid injections she received reactivated her TB. She had no signs of active TB and no history of the disease which therefore delayed diagnosis and treatment.
Clinical Message
Our case report has shown how difficult it can be to diagnose TB in a patient with no known history of the disease. The surgeon must keep an open mind and an index of suspicion to this possibility.
References
1. Tuberculosis in the UK: annual report. Public Health England. 2014.
2. Golden M P: Extrapulmonary Tuberculosis: An Overview. Am Fam Physician. 2005 ;72(9):1761-1768.
3. Babhulkar S, Pande S.Tuberculosis of the hip. Clin Orthop Relat Res 2002;398:93–99.
4. Stanish W, Hyndman j, Forsythe M. Skeletal tuberculosis: the great imitator. J Bone Jt Surg Br 1977;59B:511.
5. Spinner RJ, Sexton DJ, Goldner RD, Levin LS. Periprosthetic infections due to Mycobacterium tuberculosis in patients with no prior history of tuberculosis. J Arthroplasty 1996;11:217-22.
6. Bass J B Jr, Farer LS, Hopewell PC, O’Brien R, Jacobs RF, Ruben F et al. Treatment of tuberculosis and tuberculosis infection in adults and children. American Thoracic Society and The Centers for Disease Control and Prevention. Am J Respir Crit Care Med. 1994;149(5):1359-74.
7. Courtman NH, Weighill FJ.Systemic tuberculosis in association with intra-articular steroid therapy. J R Coll Surg Edinb 1992;37:425.
8. H¨attenschwiler A, Furrer J, G¨ Unthard HF, Schulthess G. Unexpected complication in an elderly lady suffering from rheumatoid arthritis. Schweiz Rundsch Med Prax 2004;93:372–6.
9. Harrison W, Johnson-Lynn S, Cloke D & Candal-Couto J. Presentation of Mycobacterium tuberculosis following subacromial corticosteroid injection. Shoulder & Elbow 2013;5(4).
10. Peterson CA. Tuberculous arthritis following intraarticular steroids. J Bone Joint Surg Am 1976;58:279.
11. Meir Marmor. Tuberculosis Infection Complicating Total Knee Arthroplasty . The Journal of Arthroplasty 2004;19(3):397-400.
12. J. de Haan, A.W.J.Vreeling, G.G. Van Hellemondt. Reactivation of ancient joint tuberculosis of the knee following total knee arthroplasty after 61 years: a case report. The Knee 2008;15:336-338.
13. Wobeser W L, Mel Krajden et al. Evaluation of Roche Amplicor PCR Assay for Mycobacterium tuberculosis. Journal of Clinical Microbiology 1996;34(1):134-139.
| How to Cite This Article: Tadros BJ, Stafford GH. Young Adult Hip: Reactivation of dormant, previously undiagnosed Mycobacterium Tuberculosis infection following intra-articular steroid injection. Journal of Orthopaedic Case Reports 2016 Jan-Mar;6(1): 23-25. Available from: https://www.jocr.co.in/wp/2016/01/02/2250-0685-368-fulltext/ |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com