[box type=”bio”] What to Learn from this Article?[/box]
Patella osteomyelitis a rare entity can also be a differential diagnosis for anterior knee pain in diabetic patients.
Case Report | Volume 6 | Issue 2 | JOCR April-June 2016 | Page 13-15 | R. Siva Kumar, Prahalad K.Singhi, M. Chidambaram, Kiran Kakkandki DOI: 10.13107/jocr.2250-0685.408
Authors: R. Siva Kumar[1], Prahalad K.Singhi[1], M. Chidambaram[1], Kiran Kakkandki[1]
[1] Department of Orthopaedics, Preethi Hospitals Pvt Ltd., Madurai, Tamilnadu. India.
Address of Correspondence
Dr. R. Siva Kumar,
Department of Orthopaedics, Preethi Hospitals Pvt Ltd. 120 Feet Road, Ganesh Nagar, Near Mattuthavani Bus Stand, Madurai, Tamilnadu. India- Pin code 625007.
E-mail: profsivakumarspine@gmail.com, docpsin2001@yahoo.co.in
Abstract
Introduction: Patella osteomyelitis is a rare entity in adults. Most often it is seen in children of five to twelve years of age because of its unique ossification and vascularity. Immuno compromised states like HIV, tuberculosis, intravenous drug abuse and trauma have been predisposing factors for adult patellar osteomyelitis. We report two cases of patellar osteomyelitis in adult diabetic women with uncontrolled glycemic levels and having no previous history of any trauma or systemic infection.
Case Report: A 43-year-old diabetic woman presented with complaints of left knee pain and swelling with no history of trauma. On examination, pointed tenderness was present over anterior aspect of patella with patellar grind test positive. Radiography and MRI revealed solitary well circumscribed patellar cyst. Lateral chondral blisters were noted while doing arthroscopy and secretions oozed out on puncturing. Curettage was carried out for the same. Culture and sensitivity revealed no growth and the patient was prescribed antibiotics for 6 weeks.
Second case was a 46-year-old diabetic lady with similar presentation. MRI additionally showed abscess in intermuscular plains around knee joint. An aspirated fluid was negative for growth of organisms. Knee arthrotomy and curettage of patellar sinus tracts was done with evacuation of intramuscular abscess. Antibiotics were given for 6 weeks. Both patients had complete relief of symptoms.
Conclusion: Patella osteomyelitis in adults is very rare. In patients with uncontrolled diabetes, vague anterior knee pain, elevated ESR and CRP, one should keep patellar subacute osteomyelitis as a differential diagnosis which can be further confirmed by X-ray, MRI or bone scan. An appropriate early treatment with antibiotics and surgical intervention can give a satisfactory result.
Key Words: Anteriorknee pain, adult diabetesmellitus, patellar osteomyelitis
Introduction
Patella is the largest sesamoid bone in our body. It appears as a cartilaginous structure at birth and starts to ossify at the age of five years. Patella osteomyelitis is a rare condition, with highest incidence found in children between ages of five to twelve years. In 1829, Thirion from Belgium was first to report a case of patella osteomyelitis [1]. Primary hematogenous osteomyelitis of patella in adults is a rare entity often seen in immunocompromised patients with predisposing factors like HIV, intravenous drug abuse, disseminated tuberculosis and trauma. With recent surge in incidence of diabetes mellitus which also produces an immunocompromised state, may predispose to a similar condition. Here, we report two cases of patellar osteomyelitis in adult diabetic women.
Case 1:
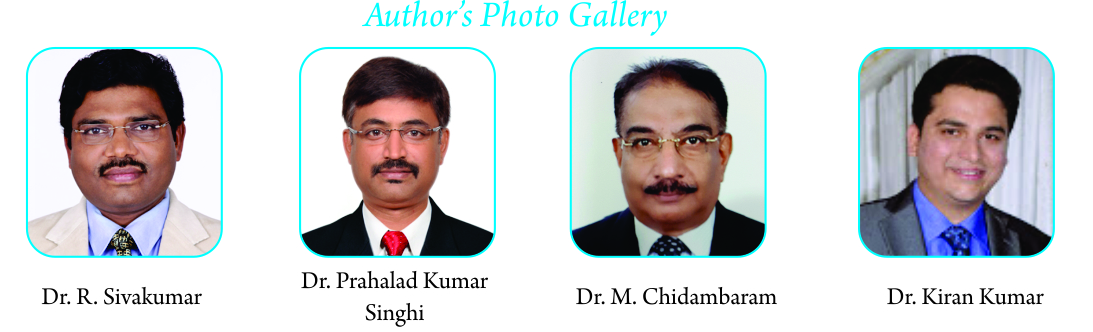
A 43-year-old lady presented to us with complaints of severe left anterior knee pain and swelling with no history of any trauma. Patient has been taking treatment with her family physician for past six weeks with no relief of symptoms but aggravation of symptoms for past few days. On examination patient was having low grade fever and rest of vitals were normal. No history of any other joint involvement, activities of daily living were affected and because of the knee pain, unable to squat and walk pain free. Patient is a known case of diabetes on medications but with uncontrolled glycemic levels. Local examination revealed local rise of temperature, minimal effusion, no discoloration of skin or any signs of trauma, point tenderness over the anterior aspect of patella, patella grind test positive and knee range of movements painful and restricted, no instability present. Investigations revealed uncontrolled sugars (fasting & postprandial and glycosylatedhemoglobin), elevated ESR 82mm at 1sthour and CRP2.9mg/L. X-ray showed solitary localized, well circumscribed patellar cyst (Fig. 1, 2) and MRI (Fig. 3, 4) confirmed it. Knee aspiration was sterile. Patient was subjected to knee arthroscopy where chondral blister was present on lateral facet of patella (Fig. 5, 6). On probing secretion oozed out, which was sent for culture and sensitivity. Curettage and thorough lavage was given. Culture reports had no growth but few pus cells were noted. Intravenous clindamycin and amikacin were given for seven days followed by oral clindamycin for next five weeks. Patient was immobilized in long knee brace with isometric and intermittent ROM exercises. Patient has excellent relief of symptoms and on further physiotherapy regained complete pain free range of movements in next four weeks.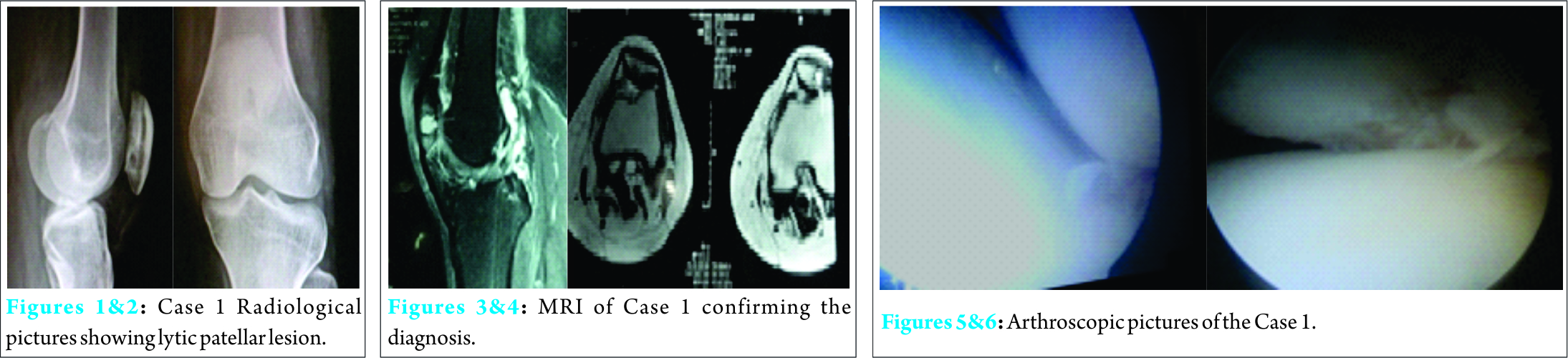
Case 2:
A 46-year-old diabetic lady with knee pain on and off for past few months, presented with severe anterior knee pain, swelling over knee and distal thigh, inability to walk, squat and complete restriction of knee movements. Patient was having high grade fever with chills and rigor. On examination, local warmth, pre patellar swelling with extension in to distal thigh and minimal joint effusion present. Tenderness over patella, patella grind test positive, ROM was painful and restricted terminally (50 – 1000) and no instability was noted. Blood test revealed uncontrolled sugars, elevated ESR (82mm at the end of 1 hour), CRP (12.8mg/dl). Radiograph had a lytic lesion (Fig. 7, 8) in patella which was identified retrospectively. MRI showed an abscess involving intermuscular plains of quadriceps encircling the distal femur and posterior compartmental muscles of leg with osteomyelitis of patella (Fig. 9). No evidence of osteomyelitis in femur and tibia. Knee aspiration was sterile. Venous Doppler study was done to rule out DVT. Patient was started on intravenous antibiotics, but had no relief of pain, so subjected to surgical intervention, knee arthrotomy with incision and drainage of abscess in quadriceps muscle was done. On patellar eversion chondral blister was seen, curettage and debridement was done. Tissue sent for histopathological examination revealed necrotic and granulation tissue consistent with osteomyelitis, tuberculosis was ruled out but no specific organism was identified. Patient had significant relief of symptoms with intravenous antibiotics for two weeks and oral antibiotics for four weeks. Patient was immobilized in long knee brace with isometric and intermittent ROM exercises. An adequate glycemic control was achieved with appropriate insulin and antidiabetic drugs.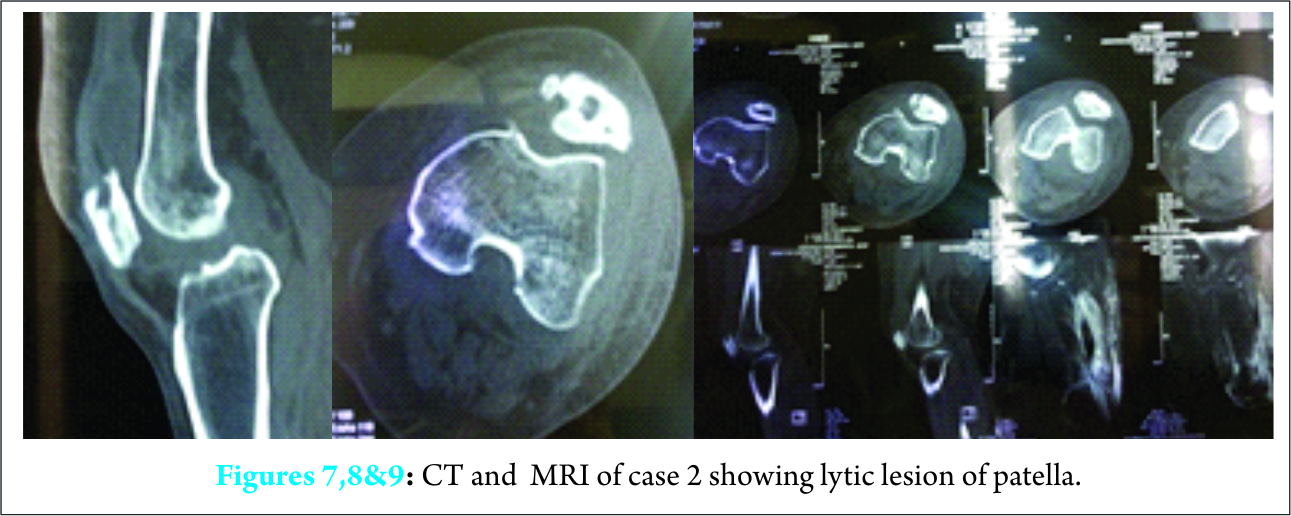
Discussion
The literature search revealed patellar osteomyelitis is a rare condition and is predominantly seen in the age group of 5 to 12 year. Patella is a cartilaginous structure with limited blood supply till the age of 5 year. Ossification begins from the age of 5 year with rich vascularisation till the age of 12 and is completed by the age of 15, beyond which the vascularity again diminishes and hence explains higher incidence of osteomyelitis between 5 to 12 year of age and decreased incidence in adults. The cartilage layer which is resistant to infection is thick in children and hence infection remains confined to patella without extending into the knee joint. Whereas in adults cartilage gets thinned out and may lead to septic arthritis of knee. Also lack of periosteum over patella explains absence of periosteal reaction which is typical of osteomyelitis at any other site. The sympathetic reaction would produce a sterile knee effusion. Rocher’s (1923) [2]series most of the patients were between five and fifteen years, only one of his patients was infant and none adult. Moore (1938) [3] suggested that the rarity of the disease under the age of five was explained by the fact that before that age the patella is cartilaginous. Ropke (1904) [4] showed by injection experiments that until the age of about four years the patella is largely a cartilaginous mass, the very little blood supply. Vascularisation then proceeds with ossification, small vessel passing into the patella from a plexus on its anterior surface. Vascularisation reaches the maximum at twelve. Very few cases of adult patella osteomyelitis have been notified in the literature. History of trauma can predispose to it, can also be as a sequalae to infected prepatellar bursitis [5]. Staphylococcusaureus is found to be most common organism in hematogenous osteomyelitis [6] followed by tubercular etiology. Immunocompromised states like HIV, intravenous drug abuse, patient on chemotherapy for malignancies are more prone for patellar infections [6-8]. Pseudomonas osteomyelitis was reported in intravenous drug abuse by Munddj et al in 1981[8]. In our cases study even though no organisms were identified, tuberculosiswas ruled out and so non-specific organism should have been an etiology and in our patients gradual onset and progressive symptoms were again suggestive of subacute nature of the infection which is more common in diabetic patient. But till now no cases of patellar osteomyelitis in diabetes have been reported in literature. The author believes that immune compromised states which exist in patient with uncontrolled diabetes mellitus are also prone to develop such infections. Few studies have been conducted on immunological function in relation to increased susceptibility to infections in diabetes mellitus [10]. Bybee and Rogers additionally had shown that phagocyte functional defect was not confined to ketoacidosisbut also occurred in poorly controlled diabetics [11]. Good control of diabetic state reversed the phagocyte defect. Another interesting observation, which suggests the possibility of genetic determination of the phagocyte defect, by Molenaar [12]. Serum factors played an important role in the phagocyte function of the diabetics; certain serum factors may competitively bind neutrophil receptors thereby preventing complement mediated phagocytosis [13]. Elimination of circulating immune complexes is also poor amongst diabetics. Chemotaxis of neurophils was found to be less in diabetics in a well controlled study of Mowat and Baum [14]. Cell mediated immunity (CMI) is a very important arc of host immunity. Assessment of lymphocyte transformation in response to phytohaemagglutinin showed a decrease in diabetics with poor control [15]. So a high index of suspicion is necessary. Supportive blood investigations, X-rays, MRI and bone scan confirm the diagnosis. When diagnosed early an arthroscopic evaluation can be diagnostic and therapeutic [16] but incases where there is a well set infection with abscess extending into quadriceps muscle an open procedure in indicated. Needle aspiration and lavage technique has been reported in a paper with satisfactory outcome. Most of the time cultures remain sterile, particularly in diabetic patients. So empirical broad spectrum antibiotics will give satisfactory results. Immobilization with knee brace and isometricand intermittent ROM exercises will avoid knee stiffness.
Conclusion
Patella osteomyelitis is a rare condition in adults, commonly seen in children. Adults with risk factors like intravenous drug abuse, HIV infection, and trauma have been common cause mentioned in the literature. Recent surge of diabetes mellitus which also produce an immuno compromised state and more prone for such infections which may have an atypical presentation, so one should have an high index of suspicion to reach the diagnosis and intervene early to have a satisfactory outcome.
Clinical Message
Atypical Anterior knee pain with poor glycemic control in a diabetic patient, a high index of suspicion toward subacute patellar osteomyelitis will enable early diagnosis and treatment and avoid complications.
References
1. THIRION ( 1829) : Successful Extirpation of the right patella for Caries (Abstract) Lancet, ii,399
2. ROCHER, H.L. (1923): Ost # {233} omy# {233d} elitelarotule. Journal de M#{233} decine de Bordeaux, 95, 921.
3. MOORE, T. (1938): Acute Osteomyelitis of the Patella, Lancet, I, 552.
4. ROPKE, W.(1904) : ZurKenntniss der Tuberculose and Osteomylitis der Patella. Archly f # {252K} Rlinischechirurgie, 73, 492.
5. Evans DK. Osteomyelitis of the patella. J.Bone Joint Surg Br 1962; 44; 319
6. Kochar VL, Srivastava KK. Unusual lesions of the patella. IntSurg 1976;61: 37-9
7. Mund DJ, MeiseAD.Pseudomonas Osteomyelitis of the patella.N Y State J Med 1981 ;81:213-14
8. Parker Vail T, Urbaniak JR. Hematogenous Osteomyelitis of the patella associated with human immunodeficiency virus Orthopaedic Review Vol XX 1991;9:788-90
9. Joseph J. Angella, MD ‘Osteomyelitis of Patella’. American Journal of Diseases of Children 1967: 113 (5), pp 590-593.
10. CE Prasad et al, Immunodeficiencies in diabetes and mycobacterial infections, INT.J. DIAB. DEV. COUNTRIES (1999), VOL.19
11. Bybee JD., Rogers DE. The phagocytic activity of polymorphonuclear leucocytes obtained from patients with diabetes mellitus, Jour Lab Clin Med. 1964,64;1.
12. Molenaar DM., Plaumbo PJ., Wilson WR., Ritts RE Jr. Leucocyte chemotaxis in diabetic patients and their nondiabetic first degree relatives. Diabetes.1976. 25,Suppl. 2;280.
13. Saeed FA., Castle GA. Neutrophil chemiluminiscence during phagocytosis is inhibited by abnormally elevated levels of acetoacetate,implications for diabetic susceptibility to infection. ClinDiag Lab Immunol. 1998. 5;5;740-3.
14. Mowatt AG., Baum J. Chemotaxis of polymorphonuclear leucocytes from patients with diabetes mellitus. N Engl J Med 1871. 284; 621-626.
15. Sheddon WH., Bauer H In Joslin’s Diabetes Mellitus 11 edition, Lea &Febiger, Philadelphia, 1871, 622.
| How to Cite This Article: Kumar RS, Singhi PK, M Chidambaram, Kakkandki K. Case Report of Two Cases of Patella Subacute Osteomyelitis in Diabetic Women A Rare Entity. Journal of Orthopaedic Case Reports 2016 April – June;6(2): 13-15. Available from: https://www.jocr.co.in/wp/2016/04/01/2250-0685-408-fulltext/ |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com