[box type=”bio”] What to Learn from this Article?[/box]
There should be high index of suspicion of prosthetic hip infection in patients presenting with Psoas abscess and vice versa.
Case Report | Volume 6 | Issue 3 | JOCR July-Aug 2016 | Page 3-6 | G D Rajitha Gunaratne, Riaz J K Khan, Cynthia Tan2, Clayton Golledge. DOI: 10.13107/jocr.2250-0685.472
Authors: G D Rajitha Gunaratne[1], Riaz J K Khan[4],[5],[6], Cynthia Tan[2], Clayton Golledge[3]
[1] Department of Orthopaedic, Royal Perth Hospital, Perth, Australia.
[2] Hollywood Private Hospital, Perth, Australia.
[3] Department of Infectious Diseases, Sir Charles Gairdner Hospital, Perth, Australia.
[4] Department of Computer Science and Engineering, Curtin University of Technology, Perth, Australia.
[5] The University of Notre Dame, Perth, Australia.
[6] The Joint Studio, Perth, Australia.
Address of Correspondence
Dr. G D Rajitha Gunaratne,
15 Nurdi Way Riverton,
Perth. WA, 6148
Australia.
E-mail: gunaratne.rajitha@gmail.com
Abstract
Introduction: Psoas abscess is a recognized but under-diagnosed complication of prosthetic hip joint infections.
Case report: We report a case of a 68-year-old man with right and left hip arthroplasties performed 22 and 14 years ago, respectively, who presented with non-specific symptoms and was subsequently diagnosed with left psoas abscess on CT scan. Drainage of the psoas abscess was complicated by the formation of a discharging sinus connected to the left hip. He then developed an infected right thigh haematoma, which also formed a discharging sinus connecting to the right hip post-drainage. He was treated with bilateral two-stage revision total hip arthroplasties and multiple courses of prolonged antibacterial therapy. Both abscesses and hip joints cultured the same species of multi-sensitive Staphylococcus aureus. The causal link between the psoas abscess and the prosthetic hip infections is discussed, as well as the investigation and management.
Conclusion: We recommend routine exploration of the iliopsoas bursa when revision of an infected total hip arthroplasty is performed to rule out intrapelvic spread of the infection [3]. There should be high index of suspicion of prosthetic hip infection in patients presenting with Psoas abscess and vice versa. A CT scan might be warranted to rule out concomitant infection in both these patients.
Keywords: Psoas abscess, prosthetic hip joint infection, hip arthroplasty.
Introduction
The risk of prosthetic hip joint infection despite standard precautions is 0.5-2% and this number is increasing with the rise in patients requiring such implants [1, 2]. Standard precautions include laminar airflow and antimicrobial prophylaxis. Psoas abscess is an uncommon but serious complication of such infection [3, 4]. Dauchy et al [5] reports 12% concomitant psoas abscess in patients presenting with prosthetic hip infections (PHI) but suggests that it is often under-diagnosed. In general, this association is also poorly reported in the literature [3]. We describe a previously unreported case of a patient with bilateral PHIs associated with a Psoas abscess, and posit that a high index of suspicion for concomitant infection is warranted to prevent complications and delays in diagnosis [6].
Case Report
A 68-year-old man presented with sepsis and a two-month history of general malaise and 18kg weight loss. His past medical history includes elective right and left hip replacements, 22 and 14 years ago, respectively. The left hip replacement was complicated with two dislocations, which were both managed with closed reduction and no complications were reported in the right hip. This is on a background of haemachromatosis with no evidence of end organ damage, thoracic shingles with no residual post-herpetic neuralgia, well-controlled gout, osteoarthritis, and a 20-pack /year history of smoking. Physical examination revealed a tender palpable mass in the left lower quadrant. Laboratory findings were as follows: haemoglobin 7.9 g/L; white cell count 8.5 x 109/L; neutrophil 6.29 x 109/L; platelet 625 x 109/L; C-reactive protein 82mg/L. CT of the chest, abdomen and pelvis identified a large left psoas abscess as seen in (Fig. 1). The psoas abscess was surgically drained and more than one litre of pus was produced. A 24 Fr 3-way catheter was inserted for irrigation of the cavity and a Yates drain was inserted in dependent position for ongoing drainage. The cavity was irrigated with normal saline twice daily, and then reduced to once daily four days post-operatively when the runoff remained clear and there was minimal residual drainage. He was empirically treated with IV Tazocin, and then switched to IV Flucloxacillin three days post-drainage, when sample cultures grew multi-sensitive Staphylococcus aureus (Table 1). He was discharged on oral Flucloxacillin 500mg three times a day and was followed up by ‘hospital in the home’ for daily irrigation post-discharge. A CT scan was performed after removal of the catheter to demonstrate resolution of the psoas abscess (Fig. 2). Two months later, a sinus developed at the left inguinal fossa over the site of drainage. This continued to drain despite management by his general practitioner with regular dressings and several courses of oral Cephalexin 500mg BD. The patient presented again several months later with a one-week history of a painful right thigh mass, which developed after he ‘pulled’ a muscle in his thigh during physiotherapy. He also complained of mild right hip pain on movement. Ultrasound was performed with the provisional diagnosis of a haematoma. Incision and drainage was performed where 450 ml of pus was drained. Cultures grew the same strain of Staphylococcus aureus as from the left psoas abscess (Table 1). A sinus formed on the right thigh also, which continued to discharge pus following the procedure. During this admission a sinogram was performed to investigate the persisting sinus from the left psoas abscess drainage site and revealed that it was communicating directly with his left total hip replacement. Interestingly he did not complain of any left hip symptoms. Radiograph of the left hip showed a small lucency at the tip of the prosthesis and below the medial calcar; the prosthesis was otherwise well fixed.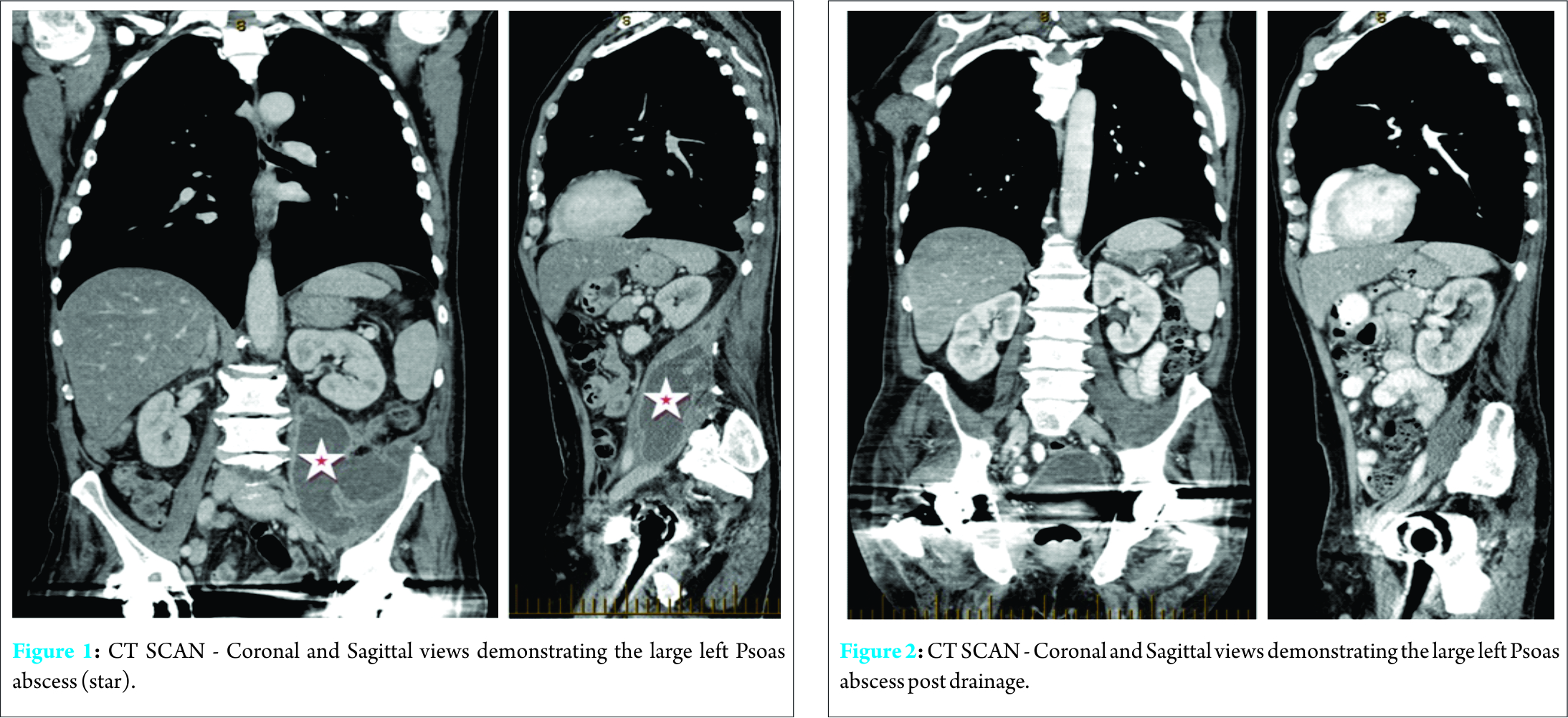
First stage revision of the left hip was performed through a posterior approach with extraction of the infected hip replacement and thorough debridement. Antibiotic impregnated (4g Vancomycin) cement spacer was inserted. Post-operatively, he was treated empirically with IV Vancomycin. The same strain of Staphylococcus aureus was isolated from left hip fluid (Table 1), and microbial sensitivity results directed the change of the antimicrobial regimen to IV Flucloxacillin. This was later changed to a two-week course of oral Dicloxacillin and Rifampicin upon normalisation of the inflammatory marker, CRP to 8.
Second stage revision of the left hip was performed three months after the first stage using the posterior approach. No sign of infection was noted in the left hip and this was confirmed with culture results (Table 1). MRI of the right hip was performed to investigate the persistent discharge from the right thigh sinus and a fluctuant right buttock mass noted during theatre. A prominent anterolateral right thigh sinus, which extended into the right hip joint could be seen. There was a large erosion posteroinferomedial to the right acetabulum, likely extending from the joint, and a very large posterior collection, mostly deep to the right gluteus maximus. Under local anaesthesia and ultrasound guidance, the right buttock collection was accessed with an 18G needle but only a small amount of blood could be aspirated. The aspirate was sent for culture; no pathogen was grown. This was most likely to represent a solidified uninfected haematoma.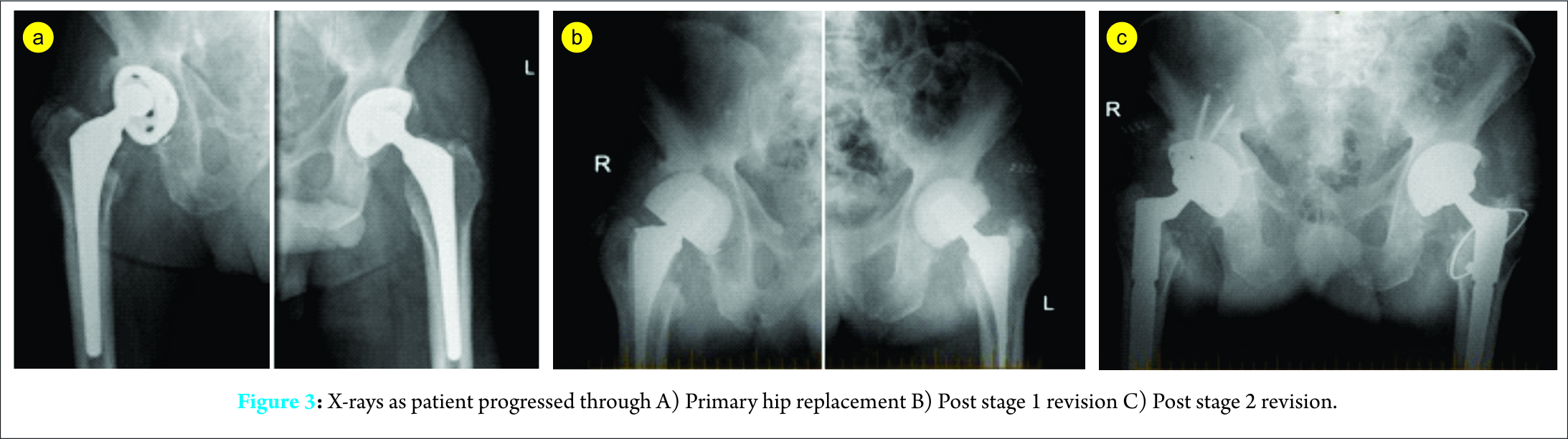
The patient underwent first-stage revision of the right hip two months later. The hip joint was exposed from the posterior approach. Copious amounts of pus was seen and drained. Following thorough debridement, antibiotic impregnated (4g Vancomycin) cement spacer was again inserted. Treatment with IV Vancomycin and oral Ceftriaxone was commenced post- operatively. All specimens collected from the right hip grew the same strain of Staphylococcus aureus as before (Table 1), and IV Flucloxacillin 2g TDS was commenced according to susceptibility results. This was switched to oral antibiotics upon discharge. Eight weeks later when the patient was off antibiotics and his CRP normalized he underwent second stage revision of the right hip. Once again no sign of infection was noted in the joint. He was on IV Flucloxacillin postoperatively, which were ceased when intraoperative samples did not culture any pathogens (Table 1).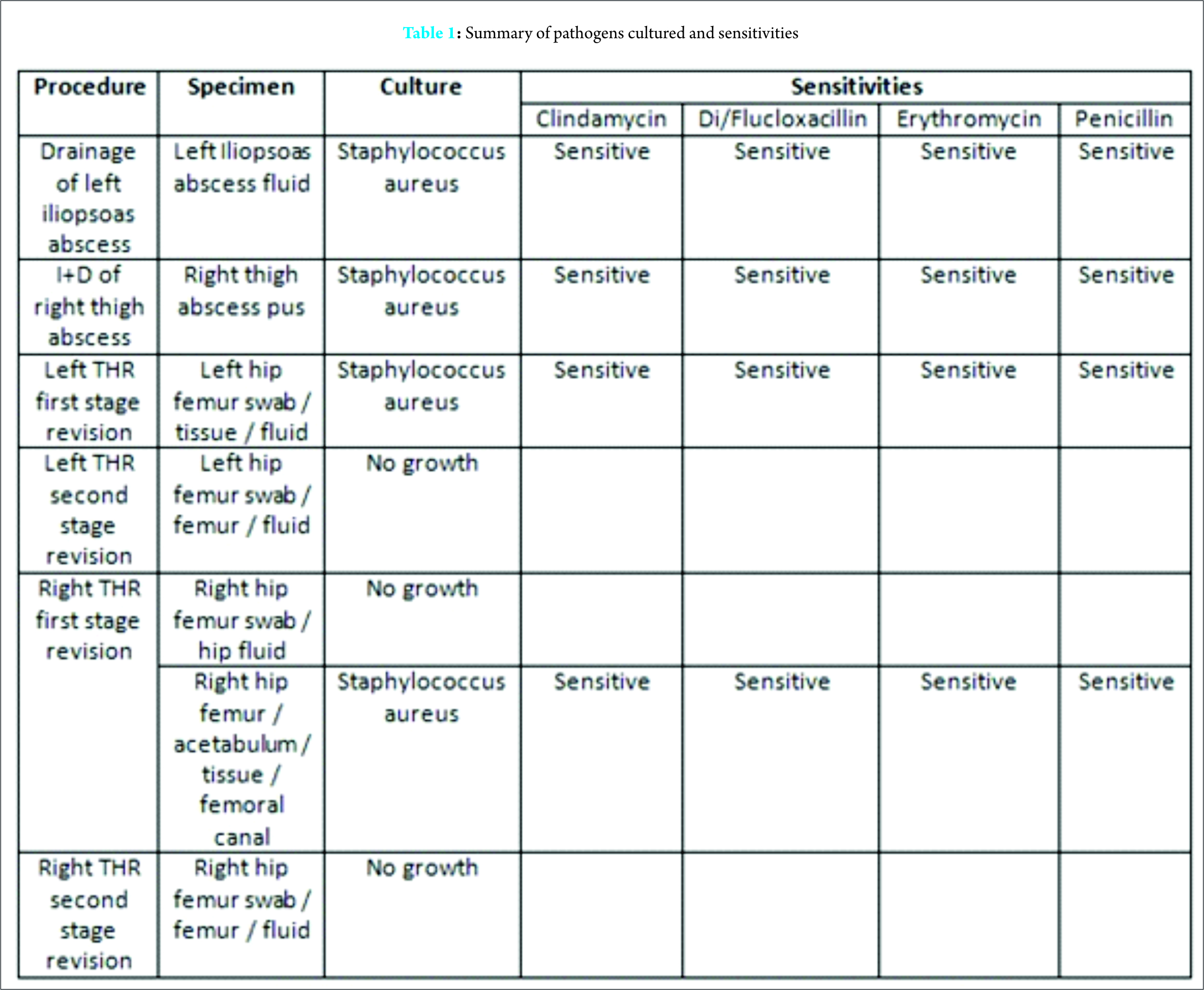
The patient received a period of inpatient rehabilitation and was discharged 13 days after surgery. Upon follow-up at six months, he remained clinically well and was mobilizing with two crutches. Pathology results were also unremarkable with normal infective and inflammatory markers. Image 3 shows the X-rays as the patient progressed through the various stages.
Discussion
This patient presented with non-specific symptoms, which is typical of a psoas abscess [4]. Since the possibility of concomitant PHI was not explored early, this lead to a delay in diagnosis of several months and the patient had more procedures than possibly required. Mortality in primary psoas abscesses is 2.4% and in secondary abscesses is 19% [7]. Mortality in untreated patients approaches 100% [4]. Primary psoas abscesses are thought to originate from distant sources via haematogenous or lymphatic spread, whereas secondary psoas abscesses arise from connecting sources of infection [4, 8]. The psoas muscle arises from the transverse processes and the lateral aspects of the vertebral bodies between the twelfth thoracic and the fifth lumbar vertebrae. The iliacus muscle joins the psoas to insert via a common tendon into the lesser trochanter of the femur. This tendon runs anterior to the hip joint capsule. The tendon is separated from the hip capsule by the iliopsoas bursa. A psoas abscess infrequently extends to the thigh and hip joint within the sheath [9]. The iliopsoas bursa is the largest synovial bursa in the body [10,11] and a cadaver study found it communicating with the hip joint in 14% of cases [11]. This bursa can also interact with the pseudocapsule formed after prosthetic implantation [12]. Thus, the hip joint can be infected by direct spread via this bursa. Whether the infected left total hip arthroplasty in this case was a cause or a consequence of the psoas abscess is open to debate. We believe the left PHI was most likely a consequence of the psoas abscess due to the lack of hip symptoms, also the pre and post psoas abscess drainage CT scans did not demonstrate any obvious involvement of the hip joint (Fig. 1, 2). Thus, the hip joint could have been infected by direct spread via iliopsoas bursa. We believe the right hip infection occured via haematogenous spread and this eventually led to formation of an abscess in the thigh and buttock via the acetabular defect. Sinuses formed post incision and drainage and continued to discharge, as the sources of infection were not addressed. The same pathogen was identified in both hips and abscesses; Staphylococus aureus. PHIs are categorized into early-onset (<3months after surgery), delayed-onset (from 3 to 12 months after surgery), and late-onset (>12 months after surgery) according to the timing of symptom onset after implantation [13]. Late-onset cases such as this one typically occur from haematogenous seeding. Staphylococus aureus is common in late onset PHIs and is also isolated in 90% of primary psoas abscesses [6]. Treatment of PHIs generally involves both surgical and antibiotic therapy [14]. A two-stage procedure is the most common surgical approach and is associated with the highest success rates [15]. This patient had a two-stage revision of both hips. This procedure consists of removal of the infected prosthesis and debridement of soft tissue and bone. An antibiotic infused joint spacer is then inserted while the patient receives parenteral antibiotics with activity against the infecting organism(s), usually for four to six weeks. A new prosthesis is reimplanted following completion of antibiotic therapy [15].
Biofilms have been shown to have an important pathogenic role with Staphylococcal infections [15]. Antimicrobial therapies against organisms within a biofilm are often unsuccessful unless the biofilm is physically disrupted or removed by surgical debridement [15]. Rifampicin is useful however, as it has an increased propensity to penetrate biofilm [15]. Accordingly, in this case surgical debridement was used to disrupt the biofilm and rifampicin was used as an antimicrobial agent. The infection was controlled by drainage of the abscesses followed by the two-stage revision of the hips. Further, specific antibiotic therapy was guided by cultures and an infectious disease specialist.
Conclusion
As demonstrated in this case, we recommend routine pre-operative imaging or exploration of the iliopsoas bursa when revision of an infected total hip arthroplasty is performed to rule out intrapelvic spread of the infection [3]. There should be high index of suspicion of PHI in patients presenting with psoas abscess and vice versa. A CT scan to rule out concomitant infection might be warranted in both these patients.
Clinical Message
There should be high index of suspicion of PHI in patients presenting with psoas abscess and vice versa. A CT scan to rule out concomitant infection might be warranted in both these patients.
References
1. Widmer AF. New developments in diagnosis and treatment of infection in orthopedic implants. Clin Infect Dis. 2001 Sept; 33(2): 94-106.
2. Berbari EF, Hanssen AD, Duffy MC et al. Risk factors for prosthetic joint infection: case-control study. Clin Infect Dis. 1998;27(5):1247-54.
3. Buttaro M, Gonzalez Della Valle A, Piccaluga F. Psoas abscess associated with infected total hip arthroplasty. J Arthroplasty 2002;17(2):230-4.
4. Ricci MA, Rose FB, Meyer KK: Pyogenic psoas abscess: worldwide variations in etiology. World J Surg. 1986;10(5):834-43.
5. Dauchy FA, Dupon M, Dutronc H, De Barbeyrac B, Lawson-Ayayi S, Dubuisson V, et al. Association between psoas abscess and prothetic hip infection: a case control study. Acta Orthopaedica 2009; 80:198-200.
6. Qureshi N, O’Brien D, Allcutt D: Psoas abscess secondary to discitis: a case report of conservative management. J Spinal Disord. 2000;13(1):73-6.
7. Mallick IH, Thoufeeq MH, Rajendran TP. Iliopsoas abscesses. Postgrad Med J. 2004;80(946):459-62.
8. Sadat-Ali M, Al-Habdan I, Ahlberg A: Retrofascialnontuberculous psoas abscess. Int Orthop. 1995;19:323-26.
9. Simons GW, Sty JR, Starshak RJ: Retroperitoneal and retrofascial abscesses: a review. J Bone Joint Surg Am. 1983;65(8):1041-58.
10. Yang SS, Bronson MJ: Cystic enlargement of the iliopsoas bursa causing venous obstruction as a complication of total hip arthroplasty: a case report. J Arthoplasty 1993;8(6):657-61.
11. Chandler S B. The iliopsoas bursa in man. Anatomical Record. 1934;58(3):235 – 240.
12. Steinbach L S, Schneider R, Goldman A B, et al. Bursae and abscess cavities communicating with the hip: diagnosis using arthrography and CT. Radiology 1985;156:302-3.
13. Zimmerli W, Trampuz A, Ochsner PE. Prosthetic-joint infections. N Engl J Med. 2004;351(16):1645-54.
14. Lentino JR. Prosthetic joint infections: bane of orthopedists, challenge for infectious disease specialists. Clin Infect Dis. 2003;36(9):1157-61.
15. Berbari E, Baddour LM, Sexton DJ et al: Treatment of prosthetic joint infections. Up to date Sep 19, 2013.
| How to Cite This Article: Gunaratne GDR, Tan C, Golledge C, J Khan RJK. Bilateral prosthetic hip joint infections associated with a Psoas abscess. A Case Report. Journal of Orthopaedic Case Reports 2016 July-Aug;6(3):3-6. Available from: https://www.jocr.co.in/wp/2016/07/10/2250-0685-472-fulltext/ |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com