[box type=”bio”] What to Learn from this Article?[/box]
Medical and surgical treatments are the options to cure calcinosis cutis. Indications for removal include pain, infection, ulceration and functional impairment. Medical therapy though not very effective, surgical excision is the mainstay of the treatment.
Case Report | Volume 6 | Issue 3 | JOCR July-Aug 2016 | Page 78-79 | Vikram V. Kadu, K. A. Saindane, Ninad Godghate. DOI: 10.13107/jocr.2250-0685.520
Authors: Vikram V. Kadu[1], K. A. Saindane[1],[2], Ninad Godghate[1]
[1]Department of Orthopaedics, ACPM Medical College, Dhule – 424001, Maharashtra. India.
[2]Department of Orthopaedics, Suyog Accident Hospital, Dhule – 424001, Maharashtra India.
Address of Correspondence
Dr. Vikram Vilasrao Kadu,
C/O Vilas Shamrao Kadu, Plot no. 20, Kadu House, Barde layout, Friends colony, Katol Road. Nagpur – 440013. India.
E-mail: vikram1065@gmail.com
Abstract
Introduction: Calcinosis circumscripta is a form of ectopic mineralization characterized by single or multiple cutaneous nodules containing calcium salts. Calcinosis cutis circumscripta is a very rare form of idiopathic calcinosis cutis arising in the second half of life. It typically involves the extremities and is associated with prior trauma and scleroderma. We dealt with a very rare form of calcinosis cutis circumscripta in a healthy patient, for whom surgical excision revealed to be an effective and successful treatment.
Case presentation: 33-year-old male presented to OPD with swelling over the right knee joint. Clinically the swelling was adhered to skin, bony hard, tender, and movements of right knee were painful. The patient was investigated and once fit was taken for surgery. The patient was treated surgically by excising the swelling.
Conclusion: Surgical excision is the mainstay of the treatment. Indications for surgical removal include pain, recurrent infection, ulceration, and functional impairment. Following excision, however, recurrence is common.
Key words: Calcinosis cutis circumscripta, knee joint, rare
Introduction
Calcinosis cutis is an uncommon disorder caused by an abnormal deposit of calcium phosphate in the skin in various parts of the body [1]. Four main types of calcinosis cutis have been recognized according to etiology: dystrophic, metastatic, iatrogenic and idiopathic [2]. Very few cases of idiopathic calcinosis cutis have been reported in the literature [3].
Case Presentation
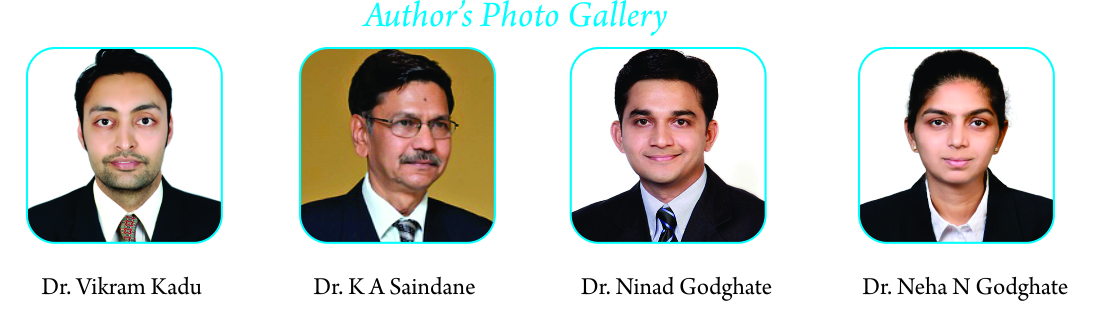
33-year-old male presented to OPD with swelling over the right knee joint [Fig. 1]. Clinically the swelling was adhered to skin, presence of hair follicles, bony hard, tender, and movements of right knee were painful. X-ray right knee joint showed a calcified mass over the anterior aspect of the knee joint [Fig. 2]. The patient was investigated and once fit was taken for surgery. The patient was treated surgically by excising the swelling. Complete excision [Fig. 3] was performed and the swelling was sent for histopathological examination. The report showed it was calcinosis cutis circumscripta [Fig. 4]. The patient was given short hinge knee brace for 2 weeks till the sutures were removed. After 2 weeks, he was allowed full weight bearing on the affected limb. At 2 yrs follow-up, patient has functional range of movement and there is no recurrence of the swelling.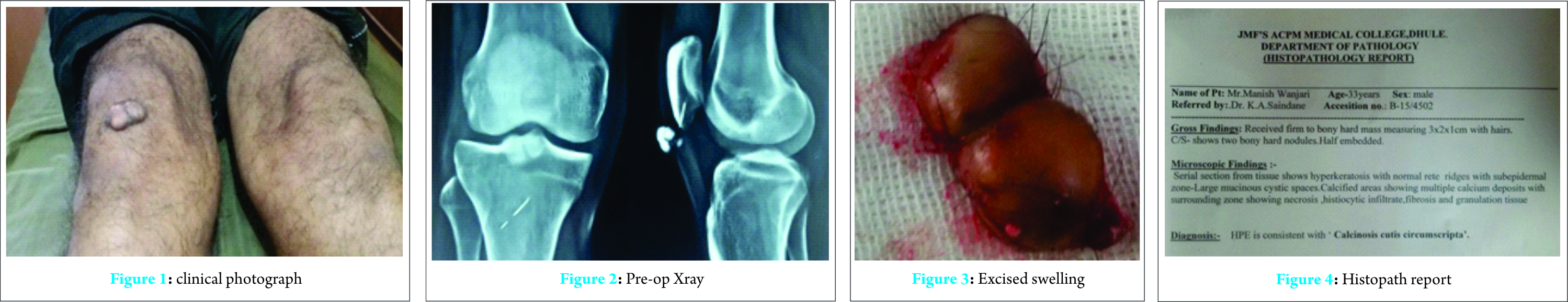
Discussion
Calcinosis cutis is a term used to describe a group of disorders in which aberrant calcium deposits form in the skin. Virchow initially described calcinosis cutis in 1855 [4]. This syndrome has been reported in both humans and animals. In humans, calcinosis circumscripta is described clinically as firm, white dermal papules, plaques, or nodules that can occur in the skin and subcutaneous tissues in hands and knees and may be associated with pressure points, tendon sheaths, and terminal phalanges. Calcinosis circumscripta in humans is more common in females than males and may be associated with various connective tissue disorders such as Reynaud’s phenomenon, scleroderma, systemic lupus erythromatosus, telangiectasia, CREST syndrome, and dermatomyositis. In addition, trauma, insect bites, metabolic calcification (e.g. renal failure), and inherited disorders (e.g., pseudoxanthoma elasticum, Werner’s syndrome, and Ehlers-Danlos syndrome) may cause calcinosis circumscripta [5]. Investigations should be done to exclude any underlying pathology. Histological examination of the lesions reveals calcium deposits in the dermis on biopsy, which may or may not be surrounded by foreign-body giant cell reaction. Alternatively, massive calcium deposits may be located in the subcutaneous tissue. Small and medium-sized blood vessels may contain calcium deposits in areas of necrosis [6]. Medical therapy of calcinosis cutis is of limited and variable benefit. If secondary to any underlying disease the cause should be treated. Intralesional corticosteroids may be beneficial. However, patients with renal insufficiency may land up in magnesium or aluminum toxicity [7]. There have been variable beneficial effects with the use of the calcium-channel blocker diltiazem over a period of at least 5 years. The therapeutic effect of this is believed to be the antagonism of the calcium–sodium ion pump [4]. Complications of calcinosis cutis include pain, cosmetic disfigurement, ulceration, and mechanical compromise. The plaques or nodules may impinge on adjacent structures such as joints, resulting in restricted mobility, and nerves, resulting in pain or paresthesia. Destruction of synovial tissue also may result. Vascular occlusion may result in gangrene. Ulceration may be complicated by bacterial infection.
Conclusion
Surgical excision is the mainstay of the treatment. Indications for surgical removal include pain, recurrent infection, ulceration, and functional impairment. Following excision, however, recurrence is common.
Clinical Message
Medical and surgical treatments are the options to cure calcinosis cutis. Medical therapy is not very effective. Surgical excision is the mainstay of the treatment.
References
1. Walsh JS, Fairley JA. Cutaneous mineralization and ossification. In: Wolff Klauss, Goldsmith LA, Katz SI, et al., eds. Fitzpatrick’s Dermatology in General Medicine. 7th ed. 2008:1293.
2. Sato K, Nakamura T, Toyama Y, Ikegami H, Kameyama K, Takayama S. Idiopathic calcinosis cutis in fingertip treated
with occlusive dressing using aluminum foil: a case report. Hand Surg. 2007;12(3):149-154.
3. Sardesai VR, Gharpuray MB. Calcinosis cutis. Indian J Dermatol Venereol Leprol. 2003;69(1):45-46.
4. Julia R Nunley, Lydia M E Jones. emedicine.medscape.com/ dermatology. Updated 27 Jan 2009.
5. Cohen 1980; Wong et al. 1986; Valdatta et al. 2003; Olsen and Chew 2006.
6. Lanka P, Lanka L.R., Ethirajan N. Idiopathic calcinosis cutis. Indian J Dermatol. 2009;54(4):388–389.[PMC free article] [PubMed]
7. Wang Wen-Jen, Lo Wen-Lin, Wong Chu-Kwan. Calcinosis cutis in juvenile dermatomyositis: remarkable response to aluminum hydroxide therapy. Arch Dermatol. 1988;124:1721–1722. [PubMed]
8. Kacerovska D, Nemcova J, Pomahacova R, Michal M, Kazakov DV. Cutaneous and superficial soft tissue lesions associated with Albright hereditary osteodystrophy: clinicopathological and molecular genetic study of 4 cases, including a novel mutation of the GNAS gene. Am J Dermatopathol. 2008 30(5):417-24.
9. Moss J, Syrengelas A, Antaya R, Lazova R. Calcinosis cutis: a complication of intravenous administration of calcium glucanate. J Cutan Pathol. 2006;33(2) :60-2.
10. Palamaras I, Kyriakis K. Calcium antagonists in dermatology: a review of the evidence and research-based studies. Dermatol Online J 2005;11(2):8.
11. Puvabanditsin S, Garrow E, Titapiwatanakun R, Getachew R, Patel JB. Severe calcinosis cutis in an infant. Pediatr Radiol. 200535(5):539-42.
| How to Cite This Article: Kadu VV, KA Saindane, Godghate N. Calcinosis Cutis Circumscripta Of Knee– A Rare Presentation. Journal of Orthopaedic Case Reports 2016 July-Aug: 6(3):78-79. Available from: https://www.jocr.co.in/wp/2016/07/10/2250-0685-520-fulltext/ |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com