[box type=”bio”] What to Learn from this Article?[/box]
Necrotizing fasciitis is life-threatening rare complication of plaster and apart from high index of suspicion and prompt surgical debridement, author recommends proper pre-cleaning of limb, use of sterile water and adequate wrap for gypsum plasters.
Case Report | Volume 6 | Issue 5 | JOCR November-December 2016 | Page 73-75 | Mohit J Jain, Kinjal Mavani DOI: 10.13107/jocr.2250-0685.640
Authors: Mohit J Jain[1], Kinjal Mavani[1]
[1]Department of Orthopaedics, V. S. Hospital, and N. H. L. Medical College, Ahmedabad, India.
Address of Correspondence
Dr. Mohit J Jain,
Department of Orthopaedics, “Bahaar,” Dharmnagar 1, 150 Feet Ring Road, Rajkot – 360 007, Gujarat, India.
E-mail: dr.mits4u@gmail.com
Abstract
Introduction: Abnormal morphology of the Anterior Inferior Iliac Spine is a rarely recognised but important source of extra-articular hip impingement. Chronic progressive symptoms of stiffness and limitation of hip motion with persistent groin pain may place significant restriction on activity. Concomitant femoro-acetabular impingement is often present but recognition and effective treatment of the uncommon extra-articular component is important for successful outcome.
Case Presentation: Three cases of symptomatic extra-articular hip impingement secondary to AIIS deformity and in conjunction with mild underlying femoro-acetabular impingement (FAI) are presented. They include two athletic Caucasian males aged 27 and 35-years old with a history of prior rectus tendon injury and secondary bony exostosis formation and a 53-year old Caucasian male with a non-traumatic, developmental AIIS deformity. In all cases an excellent clinical outcome with a full return to pain free activity was achieved post operation. Their clinical presentation, diagnosis and postoperative outcome at 1.5 to 2 years (mean 1.7 years) following arthroscopic AIIS resection are discussed.
Conclusion: Arthroscopic management of AIIS extra-articular hip impingement has been rarely reported and the longer-term outcome is unknown. We report the successful clinical outcome in a case series of three patients up to 2 years following arthroscopic AIIS resection. This case series demonstrates the sustainable benefits of arthroscopic correction of AIIS bony exostosis as a cause of extra-articular FAI.
Keywords: Hip Arthroscopy, Extra-Articular Hip Impingement, Anterior Inferior Iliac Spine (AIIS), Bony exostosis, Femoro-acetabular impingement (FAI)
Introduction
Femoro-acetabular Impingement (FAI) is a common cause of hip pathology characterised by post activity groin pain and joint stiffness, due to the abnormal repetitive contact between the femoral head/neck and the acetabular rim [1].
Extra-articular causes of hip impingement have been increasingly recognised with abnormal morphology of the Anterior Inferior Iliac Spine (AIIS) considered an important source. Deformity of the AIIS may arise from a developmental abnormality or from secondary ossification following an acute injury to the rectus femoris tendon or its apophysis. Open or arthroscopic resection of the AIIS deformity may be indicated for chronic symptoms of impingement [2-4].
We present a case series of three active, male patients with distinct clinical features of extra-articular AIIS impingement; the diagnosis and the mid-term post-operative outcomes at a mean of 1.7 years (1.5 – 2 years) following arthroscopic surgery, with treatment of concomitant intra-articular pathology, are discussed.
Case Series
(a) Patient 1:
A 27 year-old football player presented with a history of an acute-onset discomfort in his right thigh and hip when he went to kick a football during a competitive game. Over a 12-month period, he continued to experience sharp pain in the groin particularly with twisting and turning movements. His symptoms failed to improve with conservative treatment including reduction in intensity of sporting activities, physiotherapy and PRP injections into the rectus femoris tendon footprint on the AIIS (the main location of his pain).
Physical examination revealed restriction of flexion (110o) and internal rotation of the flexed hip (27o). Anterior groin pain developed once the hip was flexed above 60o and increased with flexion, adduction and internal rotation (FADDIR) manouevre.
Review of an x-ray series of the right hip including AP pelvis, Dunn and False Profile views revealed a large bony exostosis extending antero-inferiorly from the anterior inferior iliac spine (AIIS) (Figure 1a). The hip joint was in good condition however evidence of mixed FAI was present; a crossover sign was present on the AP pelvis view with a lateral centre-edge angle of 34o; a pincer deformity was clearly observed on the false profile views and an anterior labral tear was evident on MR arthrography of the hip. There was no significant CAM deformity observed at the femoral head neck region with an alpha angle of 53o measured on the Dunn view.
The patient underwent arthroscopy of his right hip through standard anterolateral and modified mid anterior portals and an anterolateral pincer deformity was removed using a 4mm mechanical burr under image intensifier guidance. The torn labrum was repaired using two suture anchors and an inter-portal capsulotomy was repaired using three fibrewire stitches. The large extra-capsular bony exostosis was located using image intensifier guidance. The instruments were then re-positioned adjacent to the exostosis which was subsequently removed using a 5.5mm mechanical burr.
At three months post-surgery the patient was able to run with an increased stride and freedom of hip movements. Improvements were observed in flexion by 3 o (110 o to 113 o) and internal rotation by 11 o (27 o to 38 o). Post-operative x-rays revealed complete removal of the large bony AIIS exostosis on all views, with a decrease in the lateral centre edge angle by 9o (34o to 25o) with reversal of the crossover sign evident on the AP pelvis view (Figure 1b). Optimal resection of the pincer deformity was evident on the false profile view.
Improvements, at 1.5 year post-operation, were observed across a range of validated health questionnaires: modified Harris Hip Score: 68 (pre-op) – 100 (post-op); UCLA activity rating: 9 (pre-op) – 10 (post-op); Short Form-36: 64.8 (pre-op) – 97.5 (post-op); WOMAC osteoarthritic index: 28 (pre-op) – 0 (post-op).
(b) Patient 2:
A 35 year old physically active male, presented with chronic anterior groin pain for over 5 years. Despite receiving extensive physiotherapy, he had responded poorly with a continued decline in his level of activity due to recurrent symptoms. The patient recalled an injury to his proximal thigh when he was 18 years of age, which settled well with rest and physiotherapy.
Physical examination revealed significant restriction of hip flexion to 112o and internal rotation was limited to 18o (with the hip flexed to 90o); FADDIR testing resulted in pain particularly in the anterolateral region of the joint.
X-rays of the right hip revealed mixed pincer and CAM impingement in a good quality joint with a large exostosis of the anterior inferior iliac spine (AIIS) originating at the footprint of the direct tendon of rectus femoris. A loss of lateral head-neck offset was evident on AP Pelvis x-rays with an alpha angle of 65o (an alpha angle of 45o was observed on the Dunn view); lateral centre-edge angle (CEA) of 40o was measured and a crossover sign observed; a pincer deformity was evident on the false profile views. MRA scans identified an anterior labral tear in the right hip.
The patient underwent arthroscopy of his right hip with removal of the pincer and lateral CAM deformities. The labrum was found to have a chondrolabral detachment antero-laterally, which was repaired using two suture anchors. The AIIS deformity was located using x-ray guidance and a complete resection of the exostosis, which was rigidly attached to the pelvis, was performed using a 5.5mm mechanical burr (Figure 2a-c).
Post-operative x-rays demonstrated an improvement in the lateral CEA by 6o (40o to 34o) and alpha angle by 8o (65o to 57o). Complete resection of the pincer deformity (false profile view) (Figure 2d and 2e) and the AIIS bony exostosis (all views) was observed.
At 18 months post-operation the patient was pain free: the range of hip flexion improved by 10o (112o to 122o) and internal rotation (of the flexed hip) by 12 o (18o to 30o). UCLA improved from 7 (pre-op) – 9 (post-op); WOMAC: 7 (pre-op) – 3 (post-op); the mHHS: 100 (pre-op) – 100 (post-op) and SF-36: 92 (pre-op) – 91 (post-op) remained largely unchanged.
(c) Patient 3:
A 53 year-old physically active groundskeeper, presented with a 5-year history of progressive, chronic hip and groin pain, particularly upon forward bending or twisting and turning movements. There was a failure to improve with physiotherapy and conservative treatment measures.
Physical examination revealed limited range of hip movement with restriction in flexion (106o) and internal rotation of the flexed hip (28o); a catching sensation and increased groin pain resulted upon FADDIR manoeuvre.
X-rays demonstrated an area of dense ossification from the rectus femoris origin on the anterior inferior iliac spine (AIIS) forming a large exostosis over the front of the hip. The quality of the hip joint was good, however evidence of mixed CAM and pincer impingement was evident: On an AP pelvis view, a crossover sign was observed with a lateral centre edge angle of 33o, an Alpha angle of 57o and 50o was measured on the AP and Dunn views, respectively and a pincer deformity was clearly observed on the false profile view. An MR hip arthrogram revealed a small, degenerative anterior labral tear.
The patient underwent arthroscopy of the right hip. The labrum was degenerative with an intra-substance tear anteriorly. Using a (5.5mm) mechanical burr, the localised pincer deformity beneath the AIIS was removed and the femoral head-neck offset was improved; the labrum was repaired using two suture anchors.
A large 4cm hardened exostosis originating from the AIIS was resected using the mechanical burr. The exostosis was found to be relatively mobile and not fixed to the AIIS footprint on the pelvis.
Postoperative x-rays demonstrated an improvement in alpha angle by 9 o (57o to 48o: AP Pelvis) and by 4o (50o to 46 o: Dunn view) and the lateral CEA by 8 o (33o to 25o). Complete resection of the AIIS bony exostosis (all views) and pincer deformity (false profile) was observed (Figure 3), with reversal of the crossover sign also evident (AP pelvis).
At two years post-surgery the patient remained fully engaged in physical activity free from pain with excellent outcome: mHHS – 93 (pre-op), 100 (post op); UCLA 8 (pre-op), 9 (post op); SF-36 – 77.1 (pre-op), 93 (post-op); WOMAC – 37 (pre-op), 2 (post op).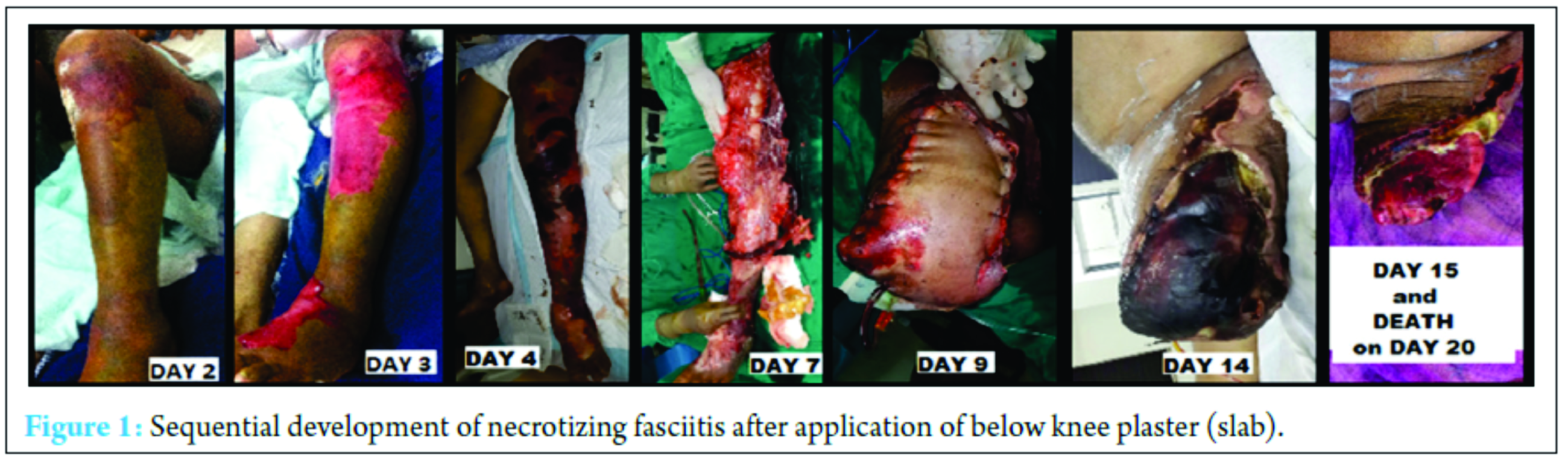
Discussion
Abnormal morphology of the anterior inferior iliac spine (AIIS) is recognised as a source of extra-articular hip impingement [2-4]. In patients presenting with AIIS impingement, there is often a history of previous trauma to the rectus femoris muscle or tendon during their adolescence. In most cases, a single explosive contraction of the rectus femoris during hyperextension of the hip joint at the same time as flexion of the knee results in apophyseal avulsion or tearing of the rectus femoris tendon [5-7]. Athletes who participate in particular impact sports that involve kicking, rapid twisting and turning or running/acceleration at high speed are at higher risk from this injury [5-7].
The injury responds well to non-operative treatment including rest, NSAIDS and physiotherapy with a predicted timeline to full recovery expected anywhere from three weeks to four months [8]. However where heterotopic ossification of the injured soft tissues or mal-union of the avulsed fragment becomes a source of chronic or delayed symptoms, surgical intervention may be indicated for relief of symptoms [5,9].
Abnormal morphology of the AIIS leading to extra-articular impingement may occur as a developmental anomaly without prior injury and may occur from traction hypertrophy by prolonged and excessive strain on the rectus femoris tendon; a retroverted acetabulum with excessive anterior pelvic tilt and following acetabular orientation surgery [4, 10].
In rarer circumstances and less well reported is the presence of the developmental anomaly known as the ‘pelvic digit’ which may contribute to impingement-like symptoms and should be considered in instances of pain and functional impairment in the absence of any history of trauma [11,12].
In our case series, patients 1 and 2 were involved in high impact sports involving sprinting and forceful kicking motions. These athletes were able to identify a specific instance where injury to the rectus femoris was likely to have occurred. In both cases a classical pattern of acute injury followed by a chronic or delayed increase in symptoms from extra-articular impingement was evident.
In contrast, patient 3 had no history of trauma but developed a chronic progressive increase in symptoms. A distinct, symptomatic bony projection with a pseudo-articulation with the pelvis was observed, which may represent a developmental abnormality such as a pelvic digit or non-traumatic ossification.
Patients with symptomatic AIIS impingement will generally present to the clinic with limitation of hip movement and associated anterior groin pain. Pain may be present on palpation of the AIIS and rectus tendon origin. Clinical signs may be subtle and similar to that of CAM/pincer FAI, as such an intra-articular injection of local anaesthetic may help differentiate the source of the primary symptoms [3,4].
Imaging is an important resource in helping to confirm the diagnosis: AP pelvis, false profile and Dunn x-rays should be utilised to assess the hip joints for the presence of CAM/pincer deformity and abnormal AIIS morphology [13]. A CT scan in addition will provide a more detailed 3D image analysis and measures of femoral and acetabular version [14]. MR Arthrography will provide information on the presence and location of articular cartilage and labral pathology [15].
While the development of large exostosis in each of our cases was likely the primary cause of impingement-like pain and discomfort, the co-existence with intra-articular abnormalities may have been a contributing factor in each case. An arthroscopic technique was therefore utilised in this case series to perform the AIIS deformity resection and to treat the concomitant FAI and associated intra-articular pathology.
Good outcome following open AIIS resection for impingement was originally described by Pan et al [2]. A number of authors have reported good outcome following the arthroscopic resection of AIIS deformity in conjunction with treatment of intra-articular pathology [3,4,9,14].
At a mean of 1.7 years (1.5 – 2.0) following impingement deformity correction, all patients in our series reported excellent functional results, improved range of hip motion, were asymptomatic, with full participation in training and recreational fitness re-established.
Conclusion
Abnormal morphology of the AIIS may result in symptomatic extra-articular hip impingement and may coexist with intra-articular bony and soft tissue hip pathology.
This case series demonstrates the sustainable benefits of arthroscopic correction of AIIS bony exostosis as an uncommon cause of extra-articular FAI.
Clinical Message
This article demonstrates three distinct clinical presentations of extra-articular hip impingement from abnormal morphology of the AIIS (one post-traumatic case with a failure of conservative management, the second also a post traumatic case with a delayed return of symptoms 5 years later and the third from a developmental non-traumatic source). Excellent post-operative results can be expected utilising an arthroscopic technique for resection of the bony deformity with a full return to normal activity up to two years post surgery. The article highlights the need for a high index of suspicion in diagnosis and treatment of active patients with hip and groin pain so that extra-articular sources for impingement are not overlooked.
References
1. Ganz R, Parvizi J, Beck M, Leunig M, Nötzli H, Siebenrock KA. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res. 2003;(417):112–20.
2. Pan H, Kawanabe K, Akiyama H, Goto K, Onishi E, Nakamura T. Operative treatment of hip impingement caused by hypertrophy of the anterior inferior iliac spine. J Bone Joint Surg Br. 2008;90(5):677–9.
3. Hetsroni I, Larson CM, Dela Torre K, Zbeda RM, Magennis E, Kelly BT. Anterior inferior iliac spine deformity as an extra-articular source for hip impingement: a series of 10 patients treated with arthroscopic decompression. Arthroscopy. 2012;28(11):1644–53.
4. Larson CM, Kelly BT, Stone RM. Making a case for anterior inferior iliac spine/subspine hip impingement: three representative case reports and proposed concept. Arthroscopy. 2011;27(12):1732–7.
5. Rajasekhar C, Kumar KS, Bhamra MS. Avulsion fractures of the anterior inferior iliac spine: the case for surgical intervention. Int Orthop. 2001;24(6):364–5.
6. Gallagher JR. FRACTURE OF THE ANTERIOR INFERIOR SPINE OF THE ILEUM: SPRINTER’S FRACTURE. Ann Surg. 1935;102(1):86–8.
7. Mader TJ. Avulsion of the rectus femoris tendon: an unusual type of pelvic fracture. Pediatr Emerg Care. 1990;6(3):198–9.
8. Yildiz C, Yildiz Y, Ozdemir MT, Green D, Aydin T. Sequential avulsion of the anterior inferior iliac spine in an adolescent long jumper. Br J Sports Med. 2005;39(7):e31.
9. Matsuda DK, Calipusan CP. Adolescent femoroacetabular impingement from malunion of the anteroinferior iliac spine apophysis treated with arthroscopic spinoplasty. Orthopedics. 2012;35(3):e460–3.
10. Siebenrock KA, Steppacher SD, Haefeli PC, Schwab JM, Tannast M. Valgus hip with high antetorsion causes pain through posterior extraarticular FAI. Clin Orthop Relat Res. 2013;471(12):3774–80.
11. Maegele M. Pelvic digit as a rare cause of chronic hip pain and functional impairment: a case report and review of the literature. J Med Case Rep. 2009;3:139.
12. Sullivan D, Cornwell WS. Pelvic rib. Report of a case. Radiology. 1974;110(2):355–7.
13. Tannast M, Siebenrock KA. Conventional radiographs to assess femoroacetabular impingement. Instr Course Lect. 2009;58:203–12.
14. Hetsroni I, Poultsides L, Bedi A, Larson CM, Kelly BT. Anterior inferior iliac spine morphology correlates with hip range of motion: a classification system and dynamic model. Clin Orthop Relat Res. 2013 Aug;471(8):2497–503.
15. Blankenbaker DG, De Smet AA, Keene JS, Fine JP. Classification and localization of acetabular labral tears. Skeletal Radiol. 2007 May;36(5):391–7.
| How to Cite This Article: Jain MJ, Mavani K. Lethal Necrotizing Fasciitis Triggered by Plaster: Case Report and Review of Literature. Journal of Orthopaedic Case Reports 2016 Nov-Dec;6(5):73‑75. Available from: https://www.jocr.co.in/wp/2016/11/10/2250-0685-640-fulltext/ |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com