[box type=”bio”] What to Learn from this Article?[/box]
Catastrophic septic arthritis of knee following Thorn prick of patella can be averted with high index of suspicion and agile action.
Case Report | Volume 6 | Issue 5 | JOCR November-December 2016 | Page 92-95 | R Sivakumar, Prahalad Kumar Singhi, M Chidambaram, V Somashekar, Vinoth Thangamani. DOI: 10.13107/jocr.2250-0685.654
Authors: R Sivakumar[1], Prahalad Kumar Singhi[1], M Chidambaram[1], V Somashekar[1], Vinoth Thangamani[1]
[1]Department of Orthopaedics, Preethi Hospitals Pvt. Ltd., Madurai, Tamil Nadu, India.
Address of Correspondence
Dr. Prahalad Kumar Singhi,
Department of Orthopaedics, Preethi Institute of Orthopaedics and Research (PRIOR), Preethi Hospitals Pvt. Limited, 120 Feet Road, Madurai, Tamil Nadu, India.
E-mail: profsivakumarspine@gmail.com
Abstract
Introduction: Sub-acute septic arthritis of knee following a thorn prick injury to patella is an uncommon condition and seen in active playful children. The child may be afraid to narrate the incident to their parents or examining doctor, so a high index of suspicion is must. The delayed presentation is inevitable. Early synovitis due to the organic biological foreign body may progress to septic arthritis, if untreated may result in knee stiffness or chronic osteomyelitis of patella.
Case Report: We report a case of thorn prick injury to the left patella in an 8-years-old boy who neglected the incident of thorn prick while playing with his peer group 10 days ago and presented with features of sub-acute septic arthritis. He was treated by arthrotomy, double inspection of the patella, removal of foreign body, synovectomy, lavage, antibiotics, and aggressive rehabilitation with an excellent outcome.
Conclusion: Sub-acute synovitis in active playful children should raise the suspicion of thorn prick even though no proper history is explained. Organic foreign body from plant materials is radiolucent and easily missed. High suspicion and timely surgical intervention, double inspection during arthrotomy identifies the foreign body. Once removed, with proper antibiotic and physiotherapy protocol followed has an excellent outcome.
Keywords: Organic thorn prick, patella, sub-acute septic arthritis of knee, double inspection.
Introduction
Foreign body patella in pediatric age group is a rare presentation. High index of suspicion is must in active playful children who present with knee swelling following a trauma. Thorn prick may be unnoticed are partially removed by the child or may conceal the history until they present with features suggestive of infection [1]. Organic foreign body, reactive synovitis, low-grade infection, sub-acute septic arthritis if still untreated may lead to chronic osteomyelitis, and knee stiffness [2].
We had one such case with presentation mimicking of septic arthritis of knee joint. On arthrotomy of the knee and double inspection of patella, a thorn remnant was identified and removed from patella, synovectomy and thorough lavage was done. Appropriate antibiotics and rehabilitation gave an excellent outcome. Arthroscopy may miss the small foreign body on the articular side and the granuloma on extra-articular side, sometimes the synovitis may obscure its vision. Arthritis following thorn foreign body is also documented in literature.
Case Report
An 8-years-old boy was admitted in our tertiary care hospital with painful swollen and stiff left knee joint for last 15 days. He sustained trivial injury and did not inform about the incident to his parents and carried his daily activities for 7 days after which he developed fever with painful swelling of the left knee. His anxious parents took the kid to local general practitioner who prescribed oral drugs for 3 days. The kid does not show a response to the oral drugs and the fever and swelling increases gradually.
Later the kid was brought to our center, on examination in the emergency room; the kid was febrile and anxious. His left knee examination shows swollen erythematous, warmth, and tender joint with fullness in suprapatellar region. Range of movements was painful and restricted. There was effusion in the joint which was clinically confirmed by positive patellar tap test. There was no evidence of any external injury to knee. Retrospective questioning following surgery he narrated an incident of thorn prick to his left knee while playing with his friends 15 days ago and he removed the broken twig of the thorn on the spot itself.
Routine blood examination was done, and the result was elevated total count (16.1×103), differential count (polymorphs – 73%, lymphocytes – 20%, and basophile – 07%). Erythrocyte sedimentation rate was – 28 mm/h and C-reactive protein positive. Hemoglobin was – 10.3 g/dl. Plain radiography of the left knee joint shows no obvious bony injury except for soft tissue swelling (Fig. 1). Magnetic resonance imaging (MRI) of the left knee joint was advised which was reported as extensive synovitis with effusion and thickened suprapatellar plica and multiple enlarged inguinal and popliteal lymph nodes with larges measuring 1.5 cm × 1.0 cm.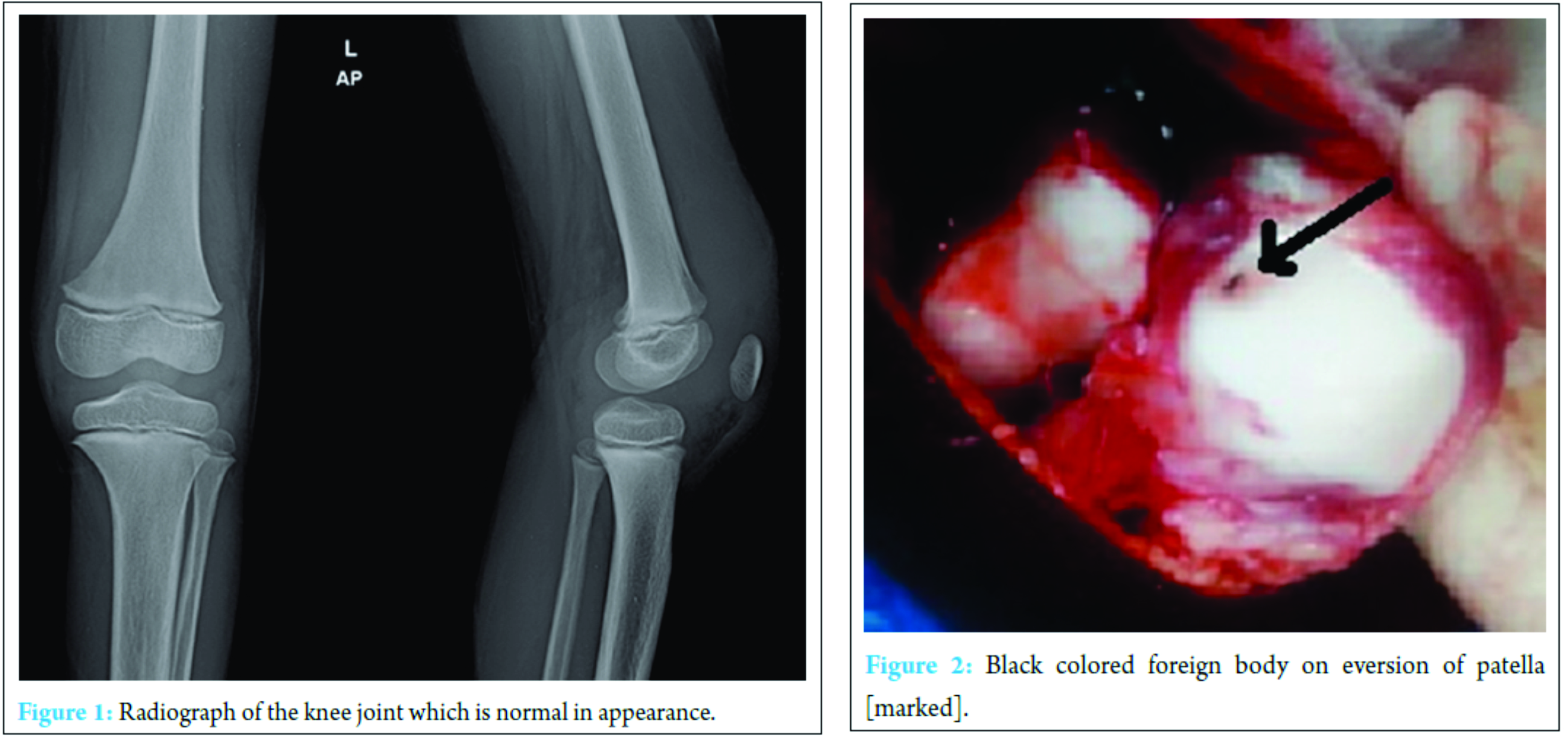
The suspicion of septic arthritis was raised. Knee arthrocentesis was done under sterile precautions, seropurulent fluid was aspirated was sent for analysis and culture and sensitivity. The kid was put on intravenous antibiotics and planned for knee arthrotomy and debridement.
Operative findings
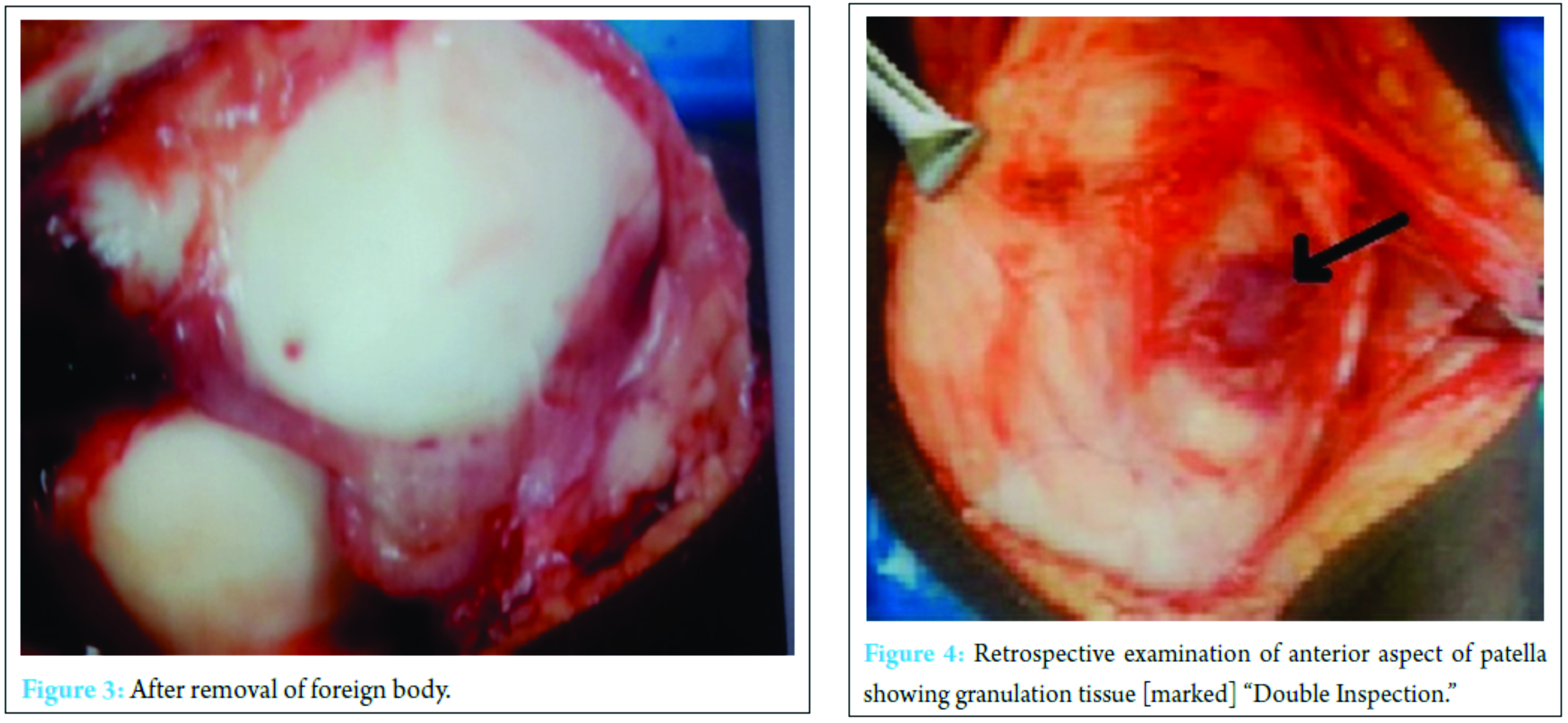
Under appropriate anesthesia after preparing, painting and draping the left knee, under tourniquet, through an anterior midline linear incision with medial parapatellar arthrotomy knee joint was opened. Seropurulent fluid was found, with extensive reactive synovitis. Near total synovectomy removing abnormal looking tissue was done specimen sent for histopathological examination. On everting the patella a black spot (Fig. 2) was noted on the articular surface on further tracing it was a foreign body appeared to be a piece of thorn and was removed. On retrospective inspection of the anterior surface of patella, an area of redness was seen appeared to be like a foreign body granuloma (Fig. 3). The tract was curetted (Fig. 4). No articular cartilage affection noticed. Through saline wash given and wound closed in layers over a negative suction draining tube. Intraoperative knee movements were found to be full.
The knee was immobilized in tube slab for 5 days and later started on continuous passive mobilization of knee according to pain tolerance. Culture and sensitivity were negative, histopathological report showed nonspecific synovitis. 1 week of intravenous antibiotics augmentin 30 mg/kg body weight/day (combination of amoxicillin and clavulanate potassium) with metronidazole 30 mg/kg/day, the kid responded well and got discharged with oral antibiotics (augmentin 375 mg a combination of amoxicillin and clavulanate potassium) for next 4 weeks. Complete range of motion was achieved by 6 weeks. At the end of 1 year follow-up he is completely asymptomatic, performing all his normal routine activities with no residual deformity or recurrence of any infection.
Discussion
Thorn prick injury to knee is a rare case presentation. It can be considered as a differential diagnosis in acute painful monoarticular arthritis in active playful child. Although the kid gives the history of removing the pricked thorn, it is just a partial broken thorn that gets out. The remnant thorn in patella causes the foreign body reaction and sub-acute septic arthritis features. Foreign body synovitis may also mimic acute septic arthritis [1].
Cartilaginous patella in infants undergoes ossification after the age of 5 years with rich vascularization until the age of 12 years and is completed by the age of 15 years, beyond which the vascularity again diminishes. The thick cartilage in children is resistant to infection, so the infection remains confined to patella for some time before extending into the knee joint. The sympathetic reaction would produce a sterile knee effusion. Whereas in adults cartilage gets thinned out may lead to septic arthritis of knee.
Suspicion is very important in diagnosing septic arthritis due to foreign body. In most of the cases as it is difficult to appreciate the entry wound, careful inspection of the joint during arthrotomies [2] for loose body or foreign body lodged in surrounding soft tissues or bones around like patella or femur and tibia is very important.
Arthroscopy can be an alternative method for joint lavage and foreign body removal [3, 4, 5]. The main pitfall in arthroscopy in such cases is a high possibility of missing the foreign body, or plica reaction causing poor visibility and leaving the thorn in situ and therefore incomplete treatment.
Double inspection of the joint on opening, before and after wash should be kept as a mandatory to avoid consequence. Imaging modality employed here, MRI has also missed the foreign body. Extraarticular foreign body may be sometime missed and hence delay in diagnosis [6].
Foreign body may be an inorganic or organic biological material which can cause a low-grade infection (anaerobic bacterial or fungal). Organic or biological foreign body is considered highly inflammatory due to its inherent alkaloid, oils, and resins composition which are toxic to humans [7, 8, 9]. Complications associated with improper removal and inadequate treatment is bursitis, acute, and sub-acute synovitis which may end up with septic arthritis. Infectious cases may have dormant presentation that is atypical for septic arthritis.
In earlier days organic foreign body was believed to be aseptic and treated with removal of the foreign body and affected synovial tissues. However, in 1977, Sugarman et al. reported the first positive synovial fluid culture with growth of Staphylococcus albus, Streptococcus hemolyticus, and Gram-negative rods after thorn prick injury. Histopathological examination of the granuloma around the foreign body shows the formation of multiple granulomata with multinucleated giant cells, hyperemia and hypertrophic synovitis, and granulation tissue in additional to small fragments of birefringent vegetable material.
The differential diagnosis would include reactive or transient synovitis, monoarticular rheumatoid arthritis, acute septic arthritis, hemophilia, leukemia, or pigmented villonodular synovitis should be considered. The inflammatory reaction to foreign body thorn may also simulate bone or soft tissue tumors.
Synovial reaction due to irritation by foreign body may stimulate an acute septic arthritis and should be kept in mind, as intravenous antibiotics and or an arthrotomy and debridement without removal of the foreign body does not cause complete resolution of the symptoms.
Conclusion
Thorn prick injury to patella is rare; it produces reactive synovitis if unintervened may lead to septic arthritis. Timely surgical intervention Arthroscopic or open arthrotomy synovectomy with lavage and removal of the foreign body is key.
Double inspection, inspection of articular, and extraarticular surface of patella.
Appropriate antibiotics and post-operative rehab will give an excellent outcome and avoids complications like knee stiffness or osteomyelitis.
Clinical Message
High index of suspicion, proper history, timely surgical intervention, double inspection, appropriate antibiotics, and post-operative rehab can give an excellent outcome even in cases of sub-acute septic arthritis of knee following organic thorn prick injury to patella in pediatrics patients.
References
1. O’Connor CR, Reginato AJ, DeLong WG Jr. Foreign body reactions simulating acute septic arthritis. J Rheumatol 1988;15(10):1568-1571.
2. Kratz A, Greenberg D, Barki Y, Cohen E, Lifshitz M. Pantoea agglomerans as a cause of septic arthritis after palm tree thorn injury; Case report and literature review. Arch Dis Child 2003;88(6):542-524.
3. Taskiran E, Toros T. Chronic synovitis caused by a date palm thorn: An unusual clinical picture. Arthroscopy 2002;18(2):E7.
4. Eiskjaer S, Larsen ST. Arthroscopy of the knee in children. Acta Orthop Scand 1987;58(3):273-276.
5. Birr R, Wuschech H, Kündiger R, Heller G. Complications in 4,000 arthroscopies. Beitr Orthop Traumatol 1990;37(11-12):
620-626.
6. Pai VS, Tan E, Matheson JA. Box thorn embedded in the cartilaginous distal femur. Inj Extra 2004;35(5-6):45-47.
7. Stevens KJ, Theologis T, McNally EG. Imaging of plant-thorn synovitis. Skeletal Radiol 2000;29(10):605-608.
8. De Champs C, Le Seaux S, Dubost JJ, Boisgard S, Sauvezie B, Sirot J. Isolation of Pantoea agglomerans in two cases of septic monoarthritis after plant thorn and wood sliver injuries. J Clin Microbiol 2000;38(1):460-461.
9. Karshner RG, Hanafee W. Palm thorns as a cause of joint effusion in children. Radiology 1953;60(4):592-595.
| How to Cite This Article: Sivakumar R, Singhi PK, Chidambaram M, Somashekar V, Thangamani V. A Sub-acute Septic Arthritis of the Knee; a Sequelae to Thorn Prick Injury of Patella: A Case Report. Journal of Orthopaedic Case Reports 2016 Nov-Dec;6(5):100-103.. Available from: https://www.jocr.co.in/wp/2016/11/10/2250-0685-654-fulltext/ |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com