[box type=”bio”] What to Learn from this Article?[/box]
To recognize a holistic approach, inclusive of social issues, must always be taken when considering mechanical joint and neurological pathology.
Case Report | Volume 7 | Issue 3 | JOCR May – June 2017 | Page 45-49| Delran Anandkumar, Ananthakrishnan Raghupathi, Ragai Gadelrab. DOI: 10.13107/jocr.2250-0685.800
Authors: Delran Anandkumar[1], Ananthakrishnan Raghupathi[2], Ragai Gadelrab[2]
[1] Department of Orthopaedics, Kettering General Hospital, Kettering, UK.
[2] Department of Orthopaedics, Newham University Hospital, London, UK.
Address of Correspondence
Dr. Delran Anandkumar,
Department of Orthopaedics, Kettering General Hospital,
Rothwell Road, Kettering, NN16 8UZ, UK.
E-mail: delran.anandkumar@nhs.net
Abstract
Introduction: The current method in dealing with pediatric hip pathologies is to avoid joint replacement unless absolutely necessary. This decision is typically made on a scientific basis. However, this is not necessarily the correct approach in all cases as demonstrated in the following case report where social issues is an extremely important variable to be considered when deciding on surgical intervention.
Case Report: This case report is the first of its kind to highlight the pathology mentioned and the social determinants that were a causative agent in its development. This case revolves around a 46-year-old Caucasian gentleman who presented in clinic enquiring about the possibility of a hip arthroplasty. He aimed to improve his ability to work after the cessation of state benefits. A retrospective look at his history indicated a number of social factors lead to poor outcomes and the resulting downward spiral causing his current presentation. The effect of social circumstances on the medical and surgical outcomes is highlighted in this report with a look into avascular necrosis and resulting natural arthrodesis. Both of these presentations were secondary to chronic and untreated childhood osteomyelitis of the right hip in conjunction with poliomyelitis development. The dual involvement of poliomyelitis and osteomyelitis to the hip joint no doubt had a massive impact on final pathology and is a rarely documented phenomenon. From an early age, this patient has faced difficulties integrating in society by factors that were out of his control. By the time he was old enough to lead an independent life, the damage had been inflicted both medically and psychologically through his earlier ordeals.
Conclusion: By writing this up, it is hoped that clinicians will recognize the debilitating holistic effect that mechanical joint pathologies and neurological deficiencies can have on patients’ lives with the view to reopen the discussion on when it is appropriate to surgically intervene in hip pathologies in children and especially where osteomyelitis and poliomyelitis are involved.
Keywords: Poliomyelitis, osteomyelitis, avascular necrosis, osteoarthritis, arthrodesis, social implications, neurological impacts.
Introduction
This report aims to discuss a rare case along with mitigating circumstances that resulted in the unusual pathology. The learning points and impact on current orthopedic practices shall also be discussed.This report aims to discuss a rare case along with mitigating circumstances that resulted in the unusual pathology. The learning points and impact on current orthopedic practices shall also be discussed.
Case Report
Mr. J is a 46-year-old gentleman requesting re-exploration of his health issues due to the recent withdrawal of his benefits. He has had pain and loss of mobility in the right hip and back (since childhood) which have impaired his ability to work for long periods of time.In 1971 when the patient was 3 years old, he stood on a rusty nail. His right leg became infected, developing osteomyelitis while also concurrently developing poliomyelitis. Neglect by his parents meant this was ignored and normal medical interventions did not take place allowing chronic infection to set in the background of poliomyelitis. This ultimately resulted in avascular necrosis (AVN) of the right hip. Subsequent treatment failed to eradicate the infection.Consequent natural arthrodesis at the right hip joint led to a loss of mobility and altered gait. Mechanical problems include a shortened right leg, atrophy of the abductors and quadriceps (due to immobility), pain in the right hip joint, and spinal hernia.
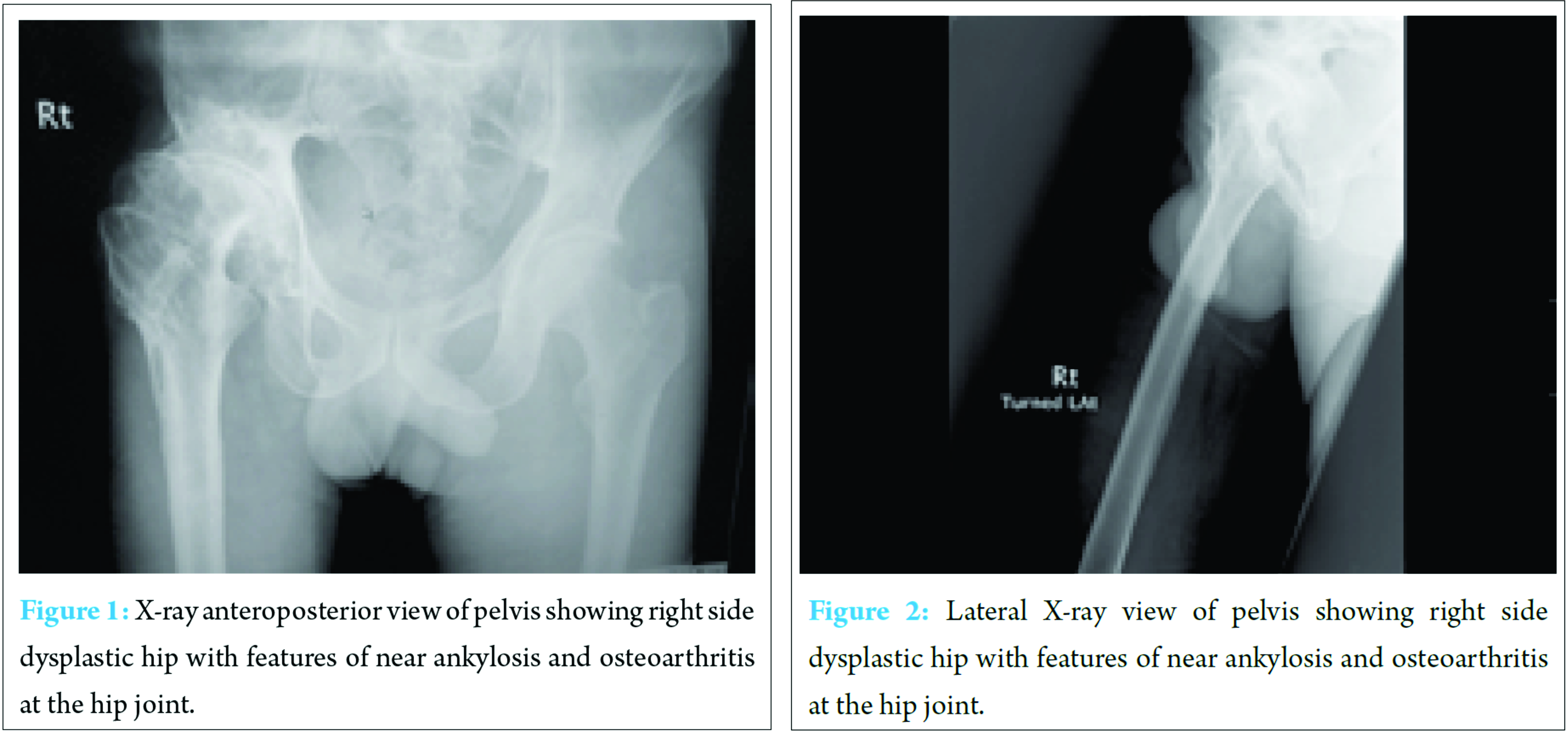
Additional problems include:• Tightness of right leg.• Falls due to adducted right leg catching left leg while walking.• Osteoarthritis of the right hip, knee, and ankle.• Shooting pain from right rib to right ankle, aggravated by stress.• Mechanical back pain which has been present over the past few years.• Spinal stenosis resulting in the loss of muscle control with urinary and fecal incontinence. Mr. J has asthma, psoriasis, agoraphobia, osteoarthritis and depression. Mr. J’s social circumstance is complicated (Table 1): General examination revealed he had antalgic gait, nil right hip movements, right quadriceps and abductor muscle wasting, and right leg on tip toe and inverted.Examination of the lower limb revealed hip flexion of up to 10°, nil hip extension, internal and external rotation and severely restricted hip abduction, and adduction movements. Spine examination showed reduced lumbar curvature. Investigations X-ray and magnetic resonance imaging findings are shown in (Fig. 1, 2, 3, 4, 5).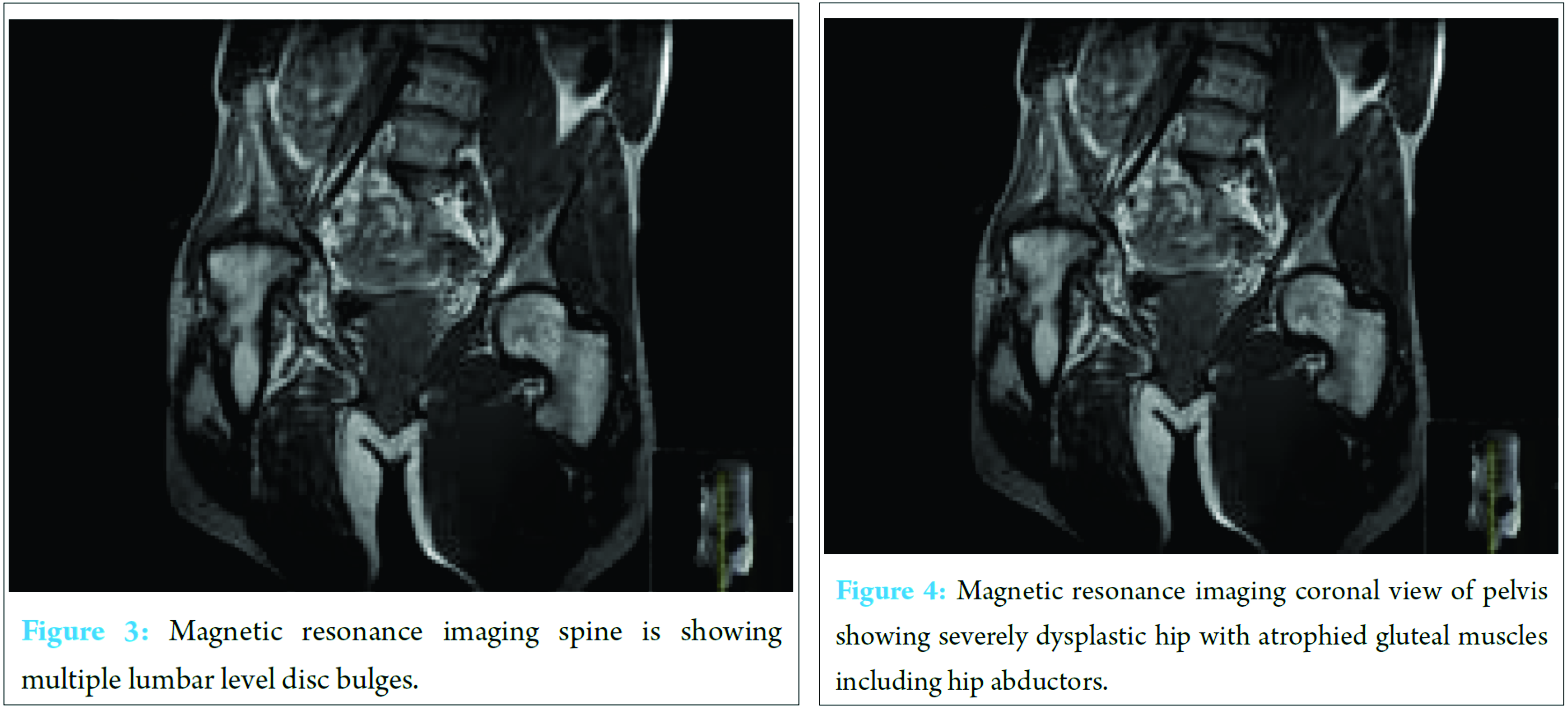 TreatmentAfter full discussion with the orthopedic team, he has decided against surgery on the grounds of surgical and social issues that may arise. This is discussed further below.
TreatmentAfter full discussion with the orthopedic team, he has decided against surgery on the grounds of surgical and social issues that may arise. This is discussed further below.
Discussion
Due to the complexity of the case, it provides a valuable opportunity to addresses a number of key issues.When the patient finally presented, AVN of the femoral head had developed from chronic infection and subsequent ankylosis. The capital femoral epiphysis is vulnerable to AVN in two ways:• Ascending branches of circumflex arteries lie around the distal capsular attachment (close to the infected area) and are at risk of compression or septic thrombosis.• Cervical branches arise from the circumflex arteries which travel to the capital femoral epiphysis. A sterile effusion in the region can cause an increase in the intra-articular pressure and therefore occlusion of these vessels by compression.After a couple of months, the epiphysis may show an increased density, and subsequent fragmentation of the area leads to collapse. In this patient’s case, it is most probable that the uncontrolled infection spread to and involved the joint. This results in the inflammatory process spreading rapidly in the avascular epiphysis and resulting in ankylosis and deformity [1]. Fusion of the hip joint due to AVN led to a loss of mobility and subsequent change in gait and muscle atrophy. At the time, the doctors refrained from performing a total hip replacement (THR) as he was just 8 years old and poliomyelitis effects. In general, there is concern about the fate of prosthetic implants in children due to wear, aseptic loosening, implant rejection, long term effects of metal/cement on surrounding tissue, and the effect of growth on the implants [2].Poliomyelitis complicated issues further as polio patients were typically not treated with THR (evidence for THR use in these instances were restricted to case reports in adults with long term effects rather than children) [3]. In these patients, surgical arthrodesis was in fact done typically to prevent future subluxations [4]. As AVN had resulted in natural fusion, he was told to wait until his forties before trying again.In the intervening years before he presented back to an orthopedic team, the muscles around his hip had atrophied due to disuse. The altered gait caused arthritic changes to numerous joints including the right hip, knee, and ankle. His lumbar spine had taken up a lot of strain due to the altered gait and therefore resulted in multiple level disc bulges indicating herniation.At a surgical standpoint, the main reason for performing hip replacement is to relieve pain and improve function. This patient has functional limitations due to capsular contractions and joint deformities resulting in a decreased range of motion of his right hip joint. This again would be improved by a THR [5]. However, this patient’s case is not straight forward as there are other factors that need to be considered which sway the case away from surgery. Bad prognostic indicators (local rather than systemic) include poor vascular supply, poor soft tissue cover, and neuropathic disease; all of which are present in Mr. J. In addition, poor muscular tone is associated with an increased dislocation rate [5]. The alteration in the dynamic hip stabilizers results in abnormal vectors around the hip, therefore, subluxation, leg length discrepancies (LLD), and osteoarthritis developing [3, 4].Surgery may, in fact, result in greater pain for the patient due to recurrent dislocations. In hip replacements, intact hip abductors are needed to protect the implant. He has lost his right femoral head, and the subsequent hip fusion has led to disuse atrophy of the muscles involved in hip movements. The musculature remaining around his hip joint especially the adductors has gone into contractures to stabilize the joint. This leads to increased stiffness, therefore, adductors needs to be released during surgery to regain mobility. In addition, abductor and tensor fascia lata muscle contractures occasionally occur after THR [6]. These muscles may need to be cut through to reduce the hip stiffness post-operative therefore lessens protection given to the new implant. The choice has to be made between reduced mobility and greater protection for the implant or; increased dislocations and pain but an increased range of motion. Finally, a normal neck cut for right hip replacement would lead to a possible right LLD. All these factors may lead to weakness of the right leg.The question is, how successful would a THR be at this stage for our patient.THR as an adultMr. J suffered from natural arthrodesis of his hip joint which resulted in painful secondary degenerative changes to the lumbar spine. Poliomyelitis patients occasionally had surgical arthrodesis of the hip due to painful subluxations which ultimately caused similar spinal problems to our patient which needed reversal with THR. It was noted that reversal of the fusion with THR, while challenging, would minimize mechanical stress on the spine. In Lau et al. paper, it is mentioned that poliomyelitis patients deformities should be addressed surgically, i.e., acetabular deformity and muscle imbalance (forming satisfactory femoral neck shaft angle) [7] (Table 2). This demonstrates that albeit our patient’s case is complex, it can be overcome with the right planning. This patient would require extensive soft tissue releases due to contractures and the importance of hip abductor braces for 6/8 weeks was stressed to prevent dislocations, minimize contractures reoccurrences and correct LLD, therefore, enable soft tissue healing. Kraay and Bigach remarked that overall, despite risk of dislocation being increased; implant durability appears reasonable and using the aforementioned techniques, dislocations can be minimized [4]. Pediatric hip replacementsStudies on pediatric THR demonstrated beneficial effects with reduced dependence on external paraphernalia, pain alleviation, and continued child growth (proximal femoral height only accounts for 0.8% of total height), with the previous reservations for THR surgery being unfounded [6]. However, post-operative instability is the main complication that arises.Raphael et al. discussed the longevity of a THR in children/young adults. They looked at a number of markers in THR in patients with cerebral palsy (another neurological condition that can affect the hip), one of which was durability of the new joint. They concluded that THR can provide durable relief from symptoms that were brought about by disease to the hip in these patients [8]. Another study by Imam et al. discussed developmental dysplasia of the hip whereby the use of uncemented THR in severe cases was recorded over 2-10 years with 100% survival of joints. They reiterated the importance of pre-operative assessment to the success of the procedures [9]. Social issues affecting orthopedic diseasesSocial implications on orthopedic diseases can be profound. Financial, cultural barriers [10], ignorance [11] and even misunderstanding of the problem [12] can all result in delayed presentation.However, one of the toughest to tackle is neglect toward children. The patient had no control of his social circumstance and knowledge of how that would affect his prognosis. A wait of 5 years before the surgical review was enough to cause serious sequela and the subsequent sporadic follow-ups worsened the situation. Questions must be raised on safeguarding that led to this patient slipping through the net.
Conclusion
This is a very complex case that had to be handled sensitively due to the issues surrounding it. The social issues are pivotal in the cause of chronic pathology and the patient’s current motivators for a hip replacement surgery. He believed that with the hip replacement and subsequent ability to move his joint, he would be capable of work without pain and therefore help his family. However, on full discussion with the orthopedic team and realizing the complications that can arise, he chose not to have anything done for the time being. While the decision not to operate in Mr. J’s childhood was made on outdated thinking, the decision for future pediatric patients should not be as limited. The arthrodesis (caused by AVN) of the joint was seen at the time as a fortuitous natural “treatment” of the poliomyelitis which meant surgical intervention was not required. However, the line of thinking surrounding poliomyelitis treatment has changed with arthrodesis now considered as a salvage procedure [8]. As stated by Ruddlesdin et al., “replacement of a joint in a growing child is not an operation to be undertaken lightly” but “earlier reservations regarding total joint replacement for these patients seem to be unfounded” [6]. The importance of planning cannot be stressed in this cohort of patients. The benefits of surgical intervention, if done correctly, can make all the difference in quality of life down the line.
Clinical Message
The human body has a remarkable capacity to adapt and minimize effects of pathological insults. However, these adaptations should be temporary, and our job as clinicians is to intervene preventing chronic changes in the body. This is true of orthopedic pathologies and in a field where there is a great scope to alleviate patients suffering in many cases, it is imperative that social issues are always considered at the start as their impact on outcomes can be devastating if missed/not accounted for.
References
1. British Society for Children’s Orthopaedic Surgery. The Management of Acute Bone and Joint Infection in Childhood a Guide to Good Practice. Available from: http://www.bscos.org.uk/resources/Downloads/Blue-Book-Infection.pdf. [Last accessed on 2014 Dec 21].1. British Society for Children’s Orthopaedic Surgery. The Management of Acute Bone and Joint Infection in Childhood a Guide to Good Practice. Available from: http://www.bscos.org.uk/resources/Downloads/Blue-Book-Infection.pdf. [Last accessed on 2014 Dec 21].
2. Lew DP, Waldvogel FA. Osteomyelitis. Lancet 2004;364(9431):369-379.
3. Queally JM, Abdulkarim A, Mulhall KJ. Total hip replacement in patients with neurological conditions. J Bone Joint Surg Br 2009;91(10):1267-1273.
4. Kraay MJ, Bigach SD. Management factorials in total hip arthroplasty-the neuromuscularly challenged patient. Bone Joint J 2014;96-B(11):27-31.
5. Kemp HB, Lloyd-Roberts GC. Avascular necrosis of the capital epiphysis following osteomyelitis of the proximal femoral metaphysis. J Bone Joint Surg Br 1974;56-B(4):688-697.
6. Ruddlesdin C, Ansell BM, Arden GP, Swann M. Total hip replacement in children with juvenile chronic arthritis. J Bone Joint Surg Br 1986;68(2):218-222.
7. Lau JH, Parker JC, Hsu LC, Leong JC. Paralytic hip instability in poliomyelitis. J Bone Joint Surg Br 1986;68(4):528-533.
8. Raphael BS, Dines JS, Akerman M, Root L. Long-term followup of total hip arthroplasty in patients with cerebral palsy. Clin Orthop Relat Res 2010;468(7):1845-1854.
9. Imam MA, Fathalla I, Holton J, Nabil M, Kashif F. Cementless total hip replacement for the management of severe developmental dysplasia of the hip in the middle eastern population: A prospective analysis. Front Surg 2016;3:31.
10. Sharma R. Flowerpot sequestrum of the Humerus Neglect for 10 years!! J Orthop Case Rep 2012;2(4):32-34.
11. Sharma R, Sohal HS, Malhotra N. Mega Tumour (Chondrosarcoma) of Humerus-an insanely large Tumor and its social implications. J Orthop Case Rep 2017;7(1):102-105.
12. Josm R. Femoral perforation after hemiarthroplasty-life goes on for 7 years! J Orthop Case Rep 2012;2(3):33-34.
 |
 |
| Dr. Ananthakrishnan Raghupathi | Dr. Delran Anandkumar |
| How to Cite This Article: Anandkumar D, Raghupathi A, Gadelra R. The Destructive Power of Circumstance on Concurrent Poliomyelitis and Osteomyelitis. Journal of Orthopaedic Case Reports 2017 May-June;7(3):45-49 |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com




