[box type=”bio”] What to Learn from this Article?[/box]
It is rare but possible that a suture granuloma can arise even years after surgery.
Case Report | Volume 7 | Issue 3 | JOCR May – June 2017 | Page 50-53| Ömer Naci Ergin, Mehmet Demirel, Emre Özmen. DOI: 10.13107/jocr.2250-0685.802
Authors:
Ömer Naci Ergin[1], Mehmet Demirel[1], Emre Özmen[1]
[1]Department of Orthopedics and Traumatology, Istanbul Faculty of Medicine, Istanbul University Çapa Fatih, Istanbul 34050, Turkey.
Address of Correspondence:
Dr. Mehmet Demirel,
Department of Orthopedics and Traumatology, Istanbul Faculty of Medicine,
Istanbul University, Çapa Fatih, Istanbul 34050, Turkey.
E-mail: dr88.mehmet.demirel@gmail.com
Abstract
Introduction: Rupture of the Achilles’ tendon is a common injury occurring particularly in middle-aged men due to sports trauma. Operative treatment is preferred generally due to lower risk of re-rupture. Possible complications of the operation include suture granulomas. Suture granulomas might represent a foreign body reaction, which itself is the end-stage response of the inflammatory wound-healing process to biomaterials. It may occur with both absorbable and non-absorbable suture materials such as silk in our case. The aim of this study is to present a case of a delayed foreign body reaction 30 years after open repair of the Achilles tendon with silk sutures.
Case Report: Our case is a 38-year-old male who presented to our outpatient clinic with complaints of swelling and pain around the posterior region of the ankle for the past 3 months. He had a history of open Achilles tendon repair at the age of 3 at the site of complaints. Physical examination was positive for a mass under the incision scar. Magnetic resonance imaging report was positive for a granulomatosis formation. The patient was booked for an operation to remove the mass.
Conclusion: Suture granuloma represents a tissue reaction against the suture material. Orthopedic literature is sparse for such cases and case reports. Both because of its rarity in orthopedic literature and the amount of time between the surgery and reaction, our report is a valuable addition to the literature.
Keywords: Orthopedic, case report, Achilles repair, suture granuloma.
Introduction
After an open repair of the Achilles tendon, miscellaneous complications, for example, infection, wound problems, and re-rupture may be encountered, by virtue of poor vascular supply and the superficial nature of the distal portion of the Achilles tendon. Therefore, surgery of the Achilles tendon requires finesse to prevent the occurrence of complications [1]. The foreign body reaction is the end-stage response of the inflammatory and wound-healing process to biomaterials, occurring from macrophages and foreign body giant cells [2]. Whether the suture material is absorbable or non-absorbable, either may cause the foreign body reaction [3, 4, 5]. However, suture granulomas are more common among non-absorbable sutures [6]. There are numerous case reports and clinical studies as regards to suture-related foreign body reaction known as suture granuloma in a variety of branches of the medicine [2, 3, 5, 6, 7, 8, 9, 10, 11, 12, 13]. However, only a small number of cases of the delayed foreign body reaction are noticed and address to orthopedic surgery. Likewise, there are a limited number of case reports which have been referred a granulomatosis formation of the Achilles tendon associated with silk [5]. The aim of this study is to present a specific case in terms of a delayed foreign body reaction 30 years after open repair of the Achilles tendon with silk. We think that our case report may contribute to the current literature as regards to management of this rare complication.
Case Report
A 38-year-old male presented to our outpatient clinic with the complaints of swelling and pain around the posterior of the ankle for the past 3 months. We revealed that he underwent an open repair of the Achilles’ tendon after it was cut by a piece of glass at 3 years of age. The operation report indicated that silk was utilized for the repair of the Achilles’ tendon. On physical examination, a quasi-solid soft tissue mass, almost 3 cm × 3 cm in size, painful with palpation, was noted on the former incision scar of the ankle (Fig. 1). There was neither fistula nor drainage. Muscle power of the plantar flexion was graded as 5/5 in addition to a slightly limited range of motion in the ankle due to pain. The infection parameters, white blood cell count, erythrocyte sedimentation, and C-reactive protein were normal in the laboratory tests (8 × 103/mL and 5 mm/h, 2 mg/L, respectively). Magnetic resonance imaging (MRI) displayed a lesion of 3 cm × 3 cm × 3 cm with low signal on both T1 and T2, and the zone around the lesion demonstrated low signal on T1 and high signal on T2, consistent with granulomatosis formation with reactive tissues around (Fig. 2). Similarly, an ultrasound revealed a heterogeneous cystic mass with echogenic material associated with the Achilles’ tendon. Together all pointed to the possibility of a chronic infection at the ankle. Aspiration of the mass showed a serohemorrhagic fluid which had negative cultures. Due to normal laboratory results and no bacteria in the culture, our initial diagnosis was that the patient had a foreign body reaction. As a result, an operation was undertaken by the senior author based on the preliminary diagnosis, physical, and radiological examination. A prophylactic single dose of cefazolin administered 1 h before spinal anesthesia. The patient was put into sleep in prone position under spinal anesthesia, and a knee above tourniquet was fastened. An incision approximately 8 cm which included the former one was longitudinally made just medially to Achilles’ tendon. There was no sign of infection at the ankle. After the enough exposure, the granulomatosis tissue was excised. Suture materials were detected inside the mass (Fig. 3). After excision of the mass, the defect about 3 cm on the tendon was repaired with polyethylene non-absorbable sutures. At the operation, the mass was dispatched to pathology and culture. After 1-wound drain was put inside the wound, the subcutaneous tissue and skin were primarily closed. Finally, a below knee circular cast was applied with the ankle at 10° of plantar flexion. Histopathological examination indicated classical findings of the foreign body reaction: Hemosiderin-loaded macrophages, giant cells, and eosinophilic infiltration. No microorganism was derived from the wound culture. 3 weeks after the operation, the circular cast was removed and the patient was followed up with an air cast until the 6th week. At the 12th month follow-up, the patient had no complaint and functional evaluation was excellent based on AOFAS (Fig. 4).
Discussion
Rupture of the Achilles’ tendon is a common injury, typically, occurring in men, mostly between the third and fourth decade of life after sports trauma. Open repair of the Achilles’ tendon indicates a low risk of re-rupture as compared to non-operative treatment [14]. Nevertheless, operative treatment has the risk of wound complications [15, 16]. There are a variety of risk factors for wound problems such as the use of tobacco, diabetes mellitus, age, gender, timing of surgery, and body mass index [14]. Moreover, suture materials have the potential to cause wound problems apart from these risk factors [4, 5].
The differential diagnosis of a suture granuloma includes lipoma, ganglion cyst, infection diseases such as abscess, tuberculosis as well as autoimmune diseases [17]. Although computed tomography (CT) and MRI are frequently sensitive at the determination of a suture granuloma, either imaging method is often ineffective at distinguishing between a suture granuloma or an abscess. However, aspiration of the mass and subsequent biopsy may be helpful to distinguish. Debridement of the foreign material is the gold standard treatment for the foreign body reaction [6]. All suture materials may elicit varying degrees of tissue hyperactivities. In the event that a suture material is recognized as a foreign body by the immune system, the tissue hyperactivity progresses to a foreign body reaction and assumes a granuloma formation. The severity and duration of the reaction depend on the type, amount, and in situ longevity of the suture material [9]. Above all, the triggering cause of suture granulomas is unclear, and it is estimated that antigens of the suture or changes related to damaged adjacent tissue may cause a suture granuloma [18]. In a review of the literature, there are a good number of clinical studies regarding delayed foreign body reactions associated with suture in other surgeries except for orthopedic surgery. For instance, foreign body reactions with Dacron have been reported in the abdominal surgery [11, 13]. Tsujita et al. presented a case report concerning the suture granuloma a short period following a gastrectomy and lymphadenectomy operation most recently [13]. Furthermore, Rossitch et al. reported a delayed foreign body reaction to silk suture in the neurosurgery [3]. In their studies, two pediatric patients suffered from late inflammatory reaction due to suture granulomas 7 years following the first neurosurgical operation. In a related way, Secil et al. reported a suture granuloma 8 months after orchiectomy [12]. In a paper by Tubbs et al., similar cases in children who underwent neurosurgery were discussed. The reactions in these cases, however, occurred in <5 years [19].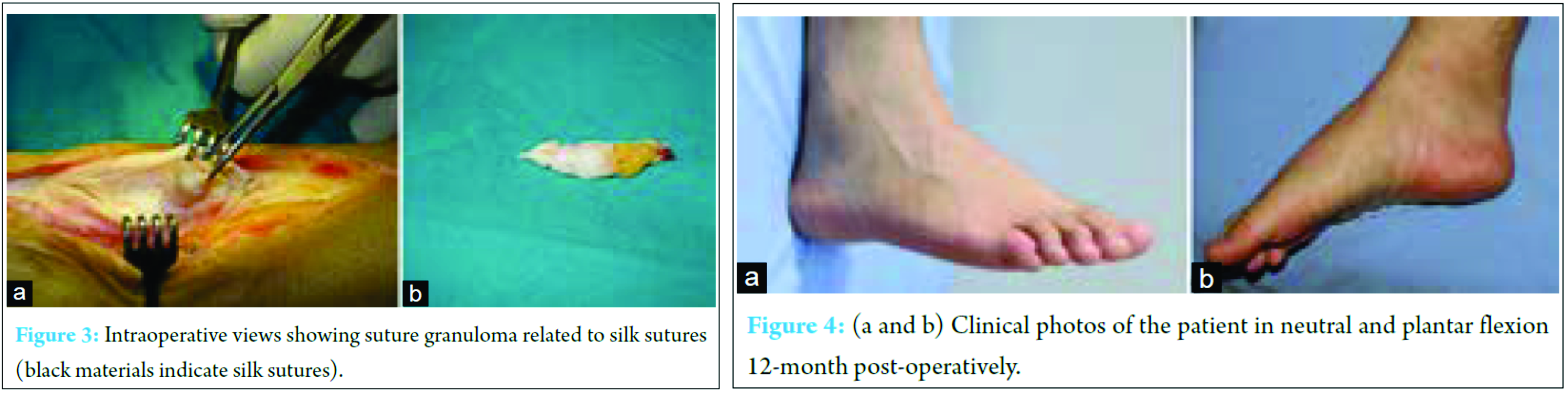
As was pointed out above, there are studies in terms of suture granulomas in the field of the general surgery, urology, ophthalmic surgery, and neurosurgery. However, suture granulomas reported in the orthopedic literature are very rare. For example, in a study by Bekler et al. [5], 4 patients who had chronic discharges associated with silk sutures utilized for open repair of Achilles’ tendon ruptures were reported. All discharges emerged 10 days to 6 months after the operation and were successfully managed by removing the sutures. In an another study by Ollivere et al. [4], a foreign body reaction associated with polyethylene “Fiberwire®” used in Achilles’ tendon repair was reported. This reaction was observed 8 months following open repair of the Achilles’ tendon. They managed by debridement and reconstruction of the Achilles’ tendon with the transfer of the flexor hallucis longus tendon. Histology enlightened a granulomatosis reaction occurring from giant cell response surrounding sections of the suture. In addition, Kara et al. [10] reported an another granuloma formation secondary to Achilles’ tendon repair with Ethibond 4 months following the first operation. Another granuloma formation due to non-absorbable suture was published by Warme et al. In this case report, a late foreign body reaction associated with TICRON (Tyco, Waltham, Massachusetts) 4 years after a shoulder inferior capsular shift operation was noticed [6]. It is rare but possible that a suture granuloma may occur several years following a surgery. The occurrence of delayed suture granulomas has varied about from 4 months to 7 years in the literature [3, 7, 8]. Here, we present a 30-year suture granuloma. To the best of our knowledge, this is the first case report which has the longest latent period among delayed foreign body reactions associated with sutures reported in the literature. Silk-related suture granuloma is very rare in the orthopedic literature. To the best of our knowledge, there is only one case series [5]. Our case is the second one which has been published to date in the literature.
Conclusion
Orthopedic surgeons may confront different complications, after an open repair of the Achilles tendon. One of these complications is the foreign body reaction to suture materials. Non-absorbable sutures have a bigger potential; nevertheless, absorbable sutures, such as silk, may cause suture granulomas as well. When a suture granuloma is encountered, infections, neoplasms, tuberculosis, and autoimmune diseases should be considered in the differential diagnosis. CT and MRI have a higher sensitivity; however, either shows a lower specificity for the recognition of the suture granuloma. Therefore, aspiration of the mass and subsequent biopsy may be efficient in the differential diagnosis. The gold standard treatment is the debridement of the foreign material. Suture granulomas commonly emerge a short period after an operation; however, surgeons should be aware of the suture granuloma having a long latent period even 30 years.
Clinical Message
Suture granuloma is usually seen in early post-operative period; however, it should be kept in mind when evaluating a patient with relative surgical history even years later.
References
1. Dalton GP, Wapner KL, Hecht PJ. Complications of Achilles and posterior tibial tendon surgeries. Clin Orthop Relat Res 2001;391:133-139.1. Dalton GP, Wapner KL, Hecht PJ. Complications of Achilles and posterior tibial tendon surgeries. Clin Orthop Relat Res 2001;391:133-139.
2. Anderson JM, Rodriguez A, Chang DT. Foreign body reaction to biomaterials. Semin Immunol 2008;20(2):86-100.
3. Rossitch E Jr, Bullard DE, Oakes WJ. Delayed foreign-body reaction to silk sutures in pediatric neurosurgical patients. Childs Nerv Syst 1987;3(6):375-378.
4. Ollivere BJ, Bosman HA, Bearcroft PW, Robinson AH. Foreign body granulomatous reaction associated with polyethelene ‘Fiberwire(®)’suture material used in Achilles tendon repair. Foot Ankle Surg 2014;20(2):e27-e29.
5. Bekler HI, Beyzadeoglu T, Gökçe A, Servet E. Aseptic drainage associated with polyglactine sutures used for repair of Achilles tendon ruptures. Acta Orthop Traumatol Turc 2008;42(2):135-138.
6. Warme WJ, Burroughs RF, Ferguson T. Late foreign-body reaction to ticron sutures following inferior capsular shift a case report. Am J Sports Med 2004;32(1):232-236.
7. Biyani CS, Upsdell SM. An unusual foreign body in the bladder 7 years after a Stamey endoscopic bladder neck suspension. Int Urogynecol J Pelvic Floor Dysfunct 1998;9(5):303-304.
8. Foster JA, John KB, Castro E, Meisler DM. Blepharoptosis surgery complicated by late suture migration. Am J Ophthalmol 2000;130(1):116-117.
9. Hochberg J, Meyer KM, Marion MD. Suture choice and other methods of skin closure. Surg Clin North Am 2009;89(3):627-641.
10. Kara A, Celik H, Seker A, Uysal MA, Uzun M, Malkoc M, et al. Granuloma formation secondary to Achilles tendon repair with nonabsorbable suture. Int J Surg Case Rep 2014;5(10):720-722.
11. LoCicero J 3rd, Robbins JA, Webb WR. Complications following abdominal fascial closures using various nonabsorbable sutures. Surg Gynecol Obstet 1983;157(1):25-27.
12. Secil M, Mungan U, Yorukoglu K. Suture granuloma after orchiectomy: Sonography, doppler and elastography features. Int Braz J Urol 2015;41(4):813-816.
13. Tsujita E, Ikeda Y, Kinjo N, Yamashita Y, Kumagai R, Taguchi K, et al. Suture granuloma with false-positive finding on PET/CT after gastrectomy for gastric cancer. Asian J Endosc Surg 2015;8(4):457-460.
14. Bruggeman NB, Turner NS, Dahm DL, Voll AE, Hoskin TL, Jacofsky DJ, et al. Wound complications after open Achilles tendon repair: An analysis of risk factors. Clin Orthop Relat Res 2004;427:63-66.
15. Pajala A, Kangas J, Ohtonen P, Leppilahti J. Rerupture and deep infection following treatment of total Achilles tendon rupture. J Bone Joint Surg Am 2002;84(11):2016-2021.
16. Khan RJ, Fick D, Keogh A, Crawford J, Brammar T, Parker M, et al. Treatment of acute Achilles tendon ruptures. J Bone Joint Surg 2005;87(10):2202-2210.
17. Mozaffar T, Lopate G, Pestronk A. Clinical correlates of granulomas in muscle. J Neurol 1998;245(8):519-524.
18. Marcus VA, Roy I, Sullivan JD, Sutton JR. Necrobiotic palisading suture granulomas involving bone and joint: Report of two cases. Am J Surg Pathol 1997;21(5):563-565.
19. Tubbs RS, Verma K, Riech S, Mortazavi M, Oakes WJ, Cohen-Gadol AA, et al. Reaction to silk suture in children undergoing neurosurgery: Case reports and review of the literature. Childs Nerv Syst 2011;27(3):497-499.
 |
 |
 |
| Dr. Emre Özmen | Dr. Mehmet Demirel | Dr. Ömer Naci Ergin |
| How to Cite This Article: Ergin ÖN, Demirel M, Özmen E. An Exceptional Case of Suture Granuloma 30 Years Following an Open Repair of Achilles Tendon Rupture: A Case Report. Journal of Orthopaedic Case Reports 2017 May-Jun;7(3):50-53. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com




