[box type=”bio”] Learning Points for this Article: [/box]
Unilateral pedicle screw fixation for degenerative spondylolisthesis though is an established surgical technique, proper patient selection with an individualized approach towards the surgery and postoperative rehabilitation keeping factors such as obesity and osteoporosis in mind is crucial to avoid early complications such as implant failure.
Case Report | Volume 7 | Issue 4 | JOCR July – August 2017 | Page 6-9| Prasoon Kumar1, Vishal Kumar, Rakesh John, Rajbahadur Sharma. DOI: 10.13107/jocr.2250-0685.824
Authors: Prasoon Kumar[1], Vishal Kumar[1], Rakesh John[1], Rajbahadur Sharma[2]
[1] Department of Orthopaedics, Postgraduate Institute of Medical Education and Research, Chandigarh, India.
[2] Department of Orthopaedics, Regional Spinal Injuries Centre, Mohali, Punjab, India.
Address of Correspondence:
Dr. Prasoon Kumar,
2240, Sector 38c, Chandigarh – 160036, India.
E-mail: drprasoonksingh@gmail.com
Abstract
Introduction: Unilateral pedicle screw fixation and transforaminal cage for interbody fusion are well-established form of treatment for lumbar spondylolisthesis. It is cost effective and has shown to have a comparable outcome to bilateral pedicle screw fixation. We present a case of unilateral pedicle screw fixation and transforaminal cage for interbody fusion in a patient of Grade 1 Degenerative spondylolisthesis who had an early implant failure, and try to assess the possible events leading to it.
Case Report: A 53-year-old female presented to our outpatient department with low back pain that had persisted for a few years. Plain radiographs revealed degenerative Meyerding Grade I spondylolisthesis at L5-S1. The patient underwent posterior decompression through left-sided laminotomy followed by pedicle screw fixation on the right side. Screws were inserted in the pedicle of L5-S1. An optimal hold of the screw in the left pedicle of L5 could not be achieved due to the poor quality of bone; hence, intraoperatively, the plan was revised from bilateral to unilateral pedicle screw fixation. Further, a transforaminal interbody cage was inserted. The patient started complaining of severe pain on the 8th post-operative day. X-ray done on the next day revealed loosening of the rod from the L5 pedicle screw, with back out of the insert screw. The patient was subsequently posted for revision surgery. During the subsequent follow-up at 6 months, the patient has shown significant symptomatic improvement and has resumed her routine daily activities.
Conclusion: Early rod loosening and migration are a rare phenomenon in lumbar pedicle screw fixation. Meticulous and precise pre-operative planning and surgical techniques may avert such complications. This case highlights the fact that though unilateral fixation is a reported treatment for listhesis, the proper case selection is needed. Conditions such as obesity and osteoporosis need to be considered, and preferably bilateral fixation should be done in such cases.
Keywords: Spondylolisthesis, unilateral pedicle screw fixation, implant failure.
Introduction
Unilateral pedicle screw fixation with transforaminal cage for interbody fusion is well established form of treatment for lumbar spondylolisthesis that is cost effective and has shown to have a comparable outcome to bilateral pedicle screw fixation [1]. It has shown to have led to significant hospital cost savings without compromising clinicoradiological outcomes [1, 2]. With strict indication and good surgical skills, transforaminal interbody fusion with single cage, combined with unilateral pedicle screw fixation in treating lumbar instability, has advantages of being relatively non-traumatic, causing less blood loss and providing faster recovery to the patients [3]. Long-term follow-up studies have shown this to have a lower rate of adjacent segment degeneration and better clinical outcome [3, 4]. Here, we present a case of unilateral pedicle screw fixation and transforaminal cage for interbody fusion in a patient of Grade 1 spondylolisthesis, complicated by early implant failure.
Case Report
A 53-year-old female presented to our outpatient department with low back pain that had persisted for few years. The patient experienced severe left lower extremity pain for several weeks with no history of trauma. The pain limited her walk to <10 m in a stretch. She had no history of previous spinal surgery. The patient was treated at a local hospital with oral analgesics. However, intermittent claudication and pain persisted. The motor examination did not reveal any weakness; however, there was hypoesthesia in the S1 dermatome. Plain radiographs revealed degenerative Meyerding Grade I spondylolisthesis at L5-S1 (Fig. 1) [5]. Subsequent magnetic resonance imaging done revealed an associated prolapsed intervertebral disc and lumbar canal stenosis (Fig. 2 and 3).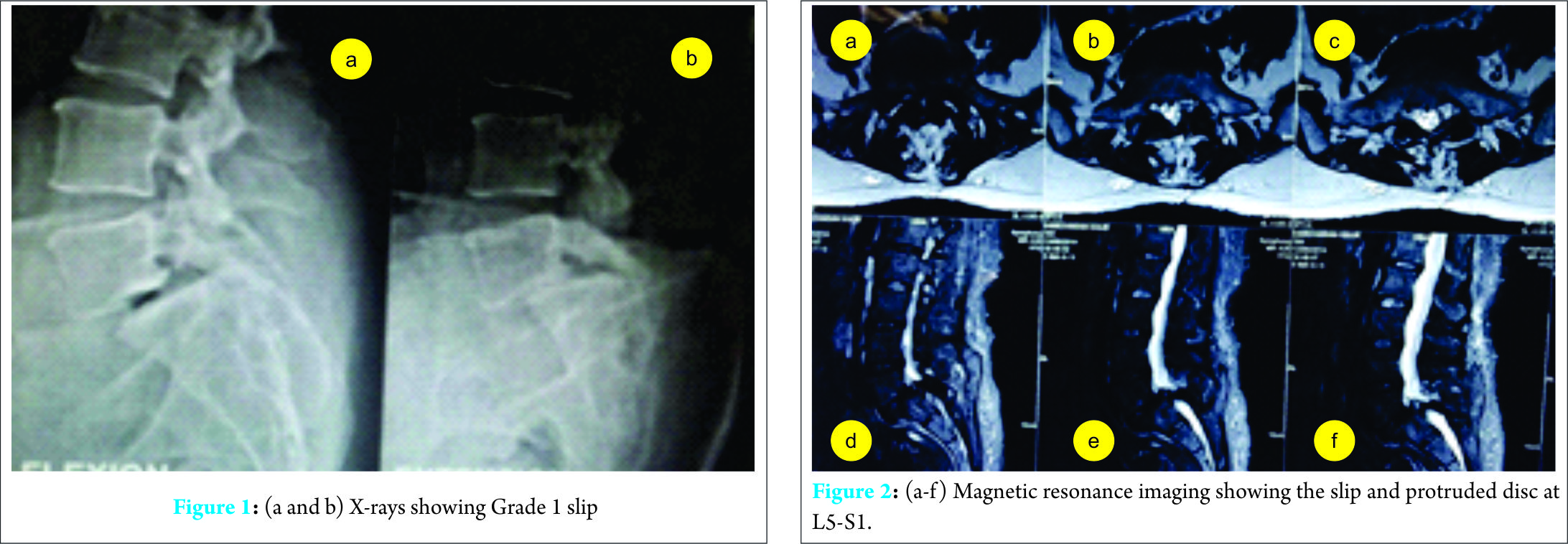 She was given a trial of caudal epidural steroid injections for symptomatic relief. The patient did not improve, and hence, surgical intervention in the form of bilateral pedicle screw fixation with interbody cage was planned. The patient underwent posterior decompression through left-sided laminotomy followed by pedicle screw fixation on the right side. Screws were inserted in the pedicle of L5-S1. An optimal hold of the screw in the left pedicle of L5 could not be achieved due to the poor quality of bone; hence, intraoperatively, the plan was revised from bilateral to unilateral pedicle screw fixation. Further, a transforaminal interbody cage was inserted. Optimal placement of the implant and the reduction was confirmed intraoperatively under C-arm (Fig. 4).
She was given a trial of caudal epidural steroid injections for symptomatic relief. The patient did not improve, and hence, surgical intervention in the form of bilateral pedicle screw fixation with interbody cage was planned. The patient underwent posterior decompression through left-sided laminotomy followed by pedicle screw fixation on the right side. Screws were inserted in the pedicle of L5-S1. An optimal hold of the screw in the left pedicle of L5 could not be achieved due to the poor quality of bone; hence, intraoperatively, the plan was revised from bilateral to unilateral pedicle screw fixation. Further, a transforaminal interbody cage was inserted. Optimal placement of the implant and the reduction was confirmed intraoperatively under C-arm (Fig. 4). 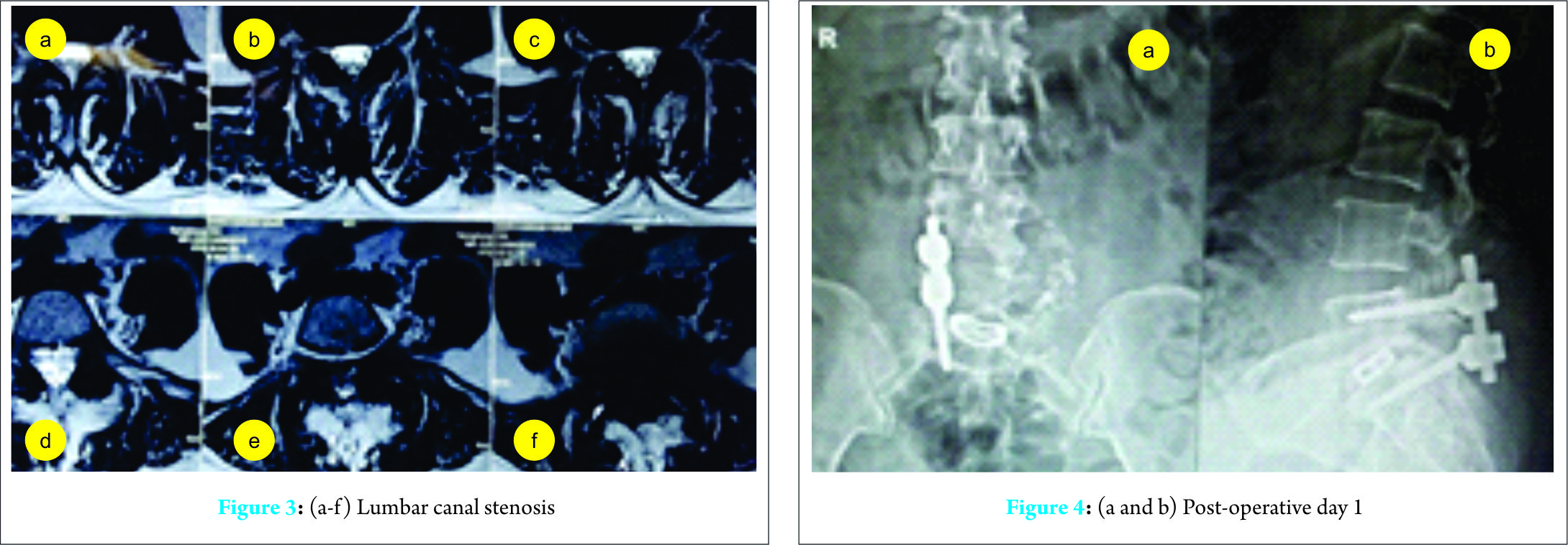 The patient was given a lumbosacral corset, and physiotherapy was initiated from the 2nd post-operative day. The patient’s leg pain decreased immediately after surgery, and ambulation was started 3 days later (Fig. 5a and b). The patient started complaining of severe pain on the 8th post-operative day, for which she was treated with oral analgesics. X-ray done on the next day revealed loosening of the rod from the L5 pedicle screw, with back out of the insert screw (Fig. 6). The patient was subsequently posted for revision surgery, where the insert screw was found to be loose and out (Fig. 7).
The patient was given a lumbosacral corset, and physiotherapy was initiated from the 2nd post-operative day. The patient’s leg pain decreased immediately after surgery, and ambulation was started 3 days later (Fig. 5a and b). The patient started complaining of severe pain on the 8th post-operative day, for which she was treated with oral analgesics. X-ray done on the next day revealed loosening of the rod from the L5 pedicle screw, with back out of the insert screw (Fig. 6). The patient was subsequently posted for revision surgery, where the insert screw was found to be loose and out (Fig. 7).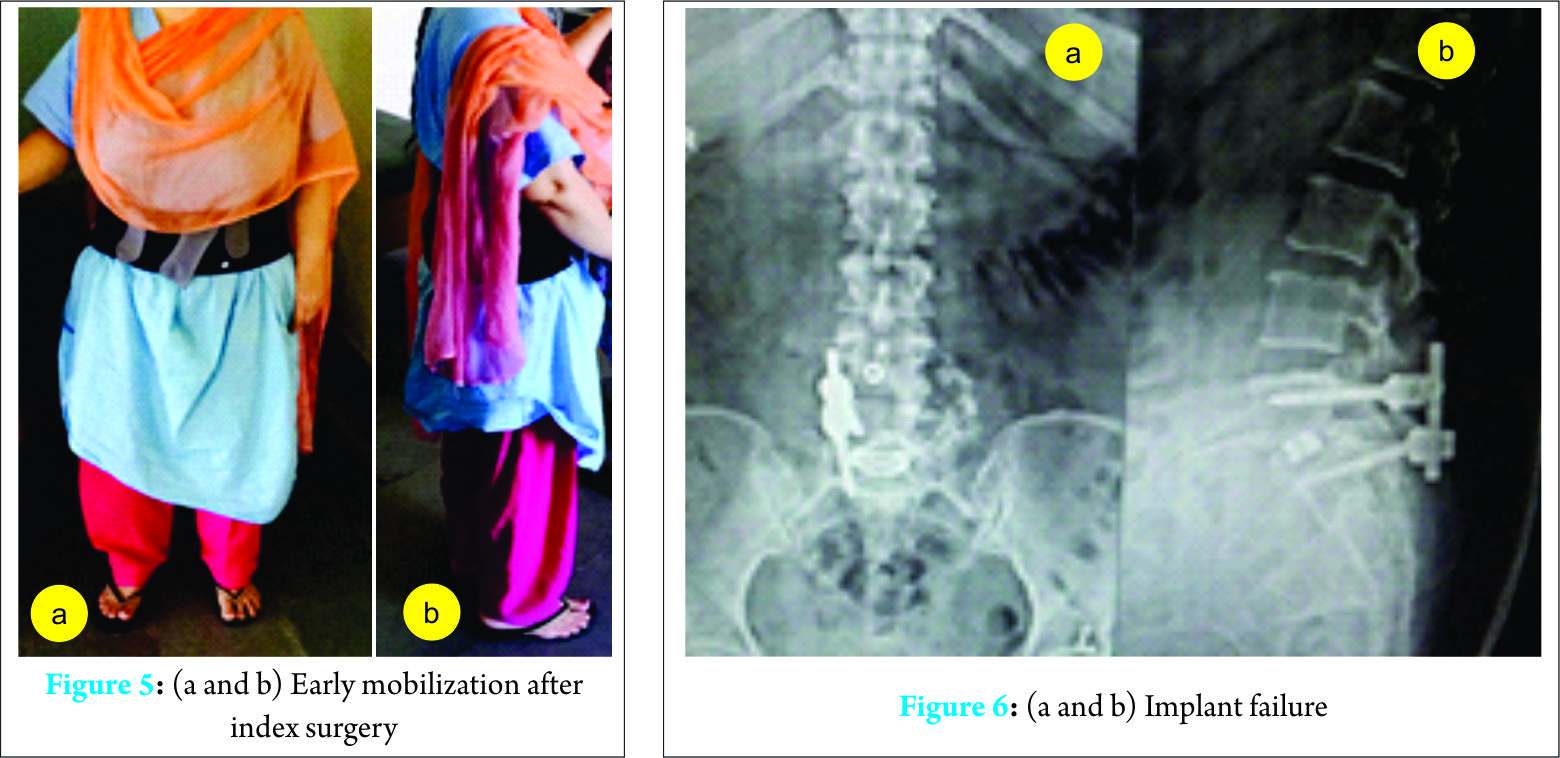 The screws were inserted now on the left pedicle of L4 and S1. Another screw was placed in the right pedicle of L4, and a longer rod was placed (Fig. 8). The patient was discharged after suture removal on the 14th post-operative day. The patient was relatively pain-free and ambulating at the time of discharge. During the subsequent follow-up at 6 months, the patient has shown significant symptomatic improvement and has resumed her routine daily activities.
The screws were inserted now on the left pedicle of L4 and S1. Another screw was placed in the right pedicle of L4, and a longer rod was placed (Fig. 8). The patient was discharged after suture removal on the 14th post-operative day. The patient was relatively pain-free and ambulating at the time of discharge. During the subsequent follow-up at 6 months, the patient has shown significant symptomatic improvement and has resumed her routine daily activities.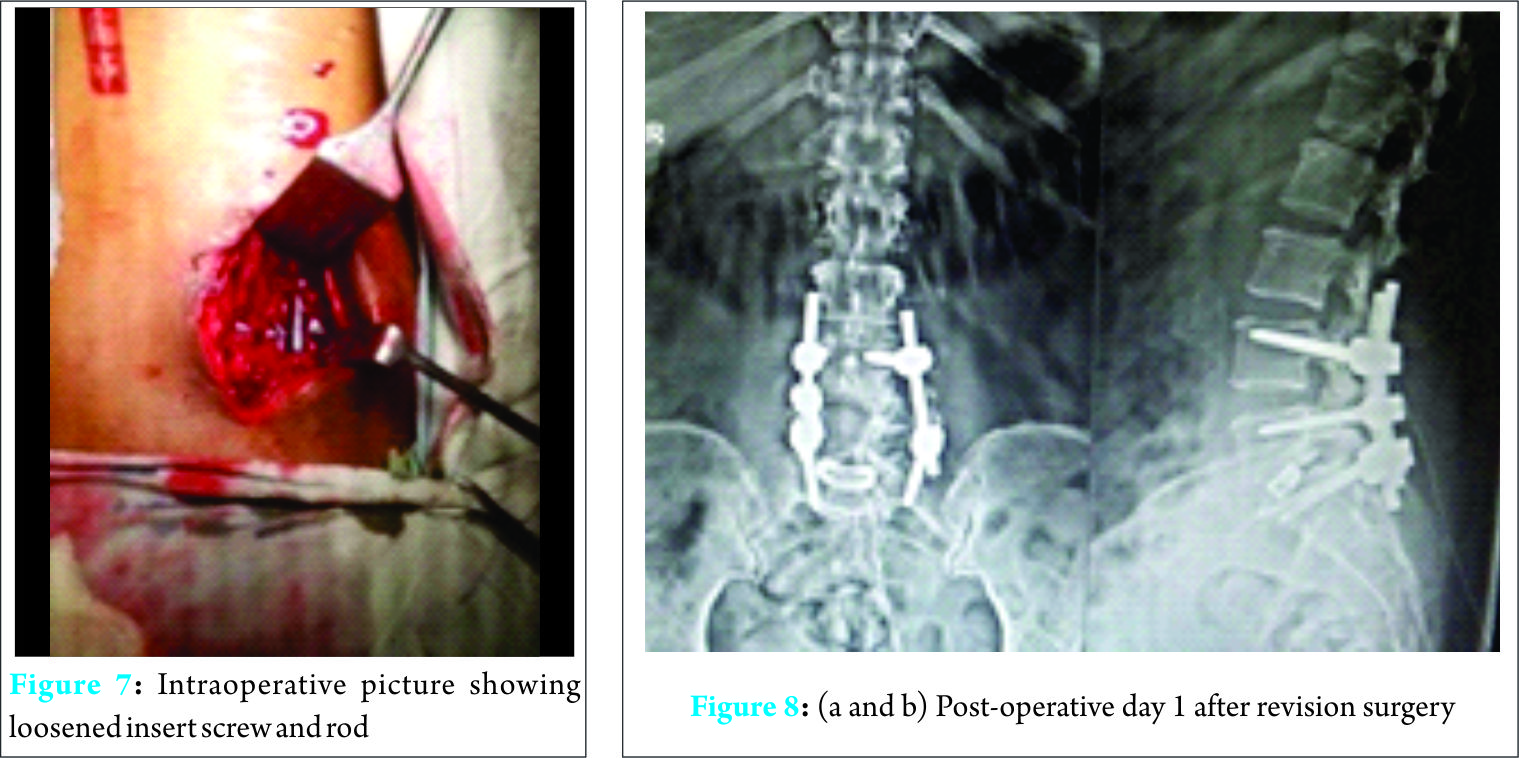
Discussion
Degenerative lumbar spondylolisthesis (DS) is a disorder that causes the slip of one vertebral body over the one below due to degenerative changes in the spine. It is a major cause of spinal canal stenosis and is often related to low back and leg pain. The degree of spondylolisthesis is based on the widely recognized method proposed by Meyerding who defined the slip on plain radiology in accordance to the vertebra below [5]. The lower vertebra is divided into four parts. Grade I means a translation of the upper vertebra of up to 25%, Grade II of up to 50%, Grade III of up to 75%, and Grade IV up to 100%. Flexion extension views aid in identifying even obscure instability. Decompression and internal fixation improve the symptoms of patients with lumbar spinal stenosis associated with spondylolisthesis. Transpedicle instrumentation can reduce spondylolisthesis and maintain the physical curve of the lumbar spine [6]. The pedicle is the strongest part of a vertebra. They are used to create strong construct in spinal stabilization surgeries [7]. The use of unilateral and bilateral pedicle screw fixation has been described. Hua et al., in their study, have termed unilateral fixation in treating lumbar instability advantageous in terms of lesser complications and cost [2]. According to Eliades et al., the results of both unilateral and bilateral fixation are similar [1]. Similar results were given by Kim et al., after 10 years of follow-up of 147 Grade 1 spondylolisthesis patients, treated with either unilateral or bilateral pedicle screw fixation for posterolateral fusion [3]. Transforaminal lumbar interbody fusion, with the aid of interbody cage and unilateral pedicle screw fixation, is less invasive and improves symptoms. In the present case, the initial plan to do bilateral fixation was changed intraoperatively, in view of poor bone quality of pedicle and strong literature evidence of unilateral fixation having comparable outcomes [1, 2, 3]. Complications described for such a fixation are hardware failure, infection, and neural damage. In the study by Faraj and Webb, screw-rod disconnection due to a technical error occurred in one case which was subsequently replaced [7]. According to Ohlin et al., transpedicular fixation is a safe procedure with a low incidence of serious early post-operative complications [8]. Early loosening of the rod and migration are very rare and reported infrequently [9, 10]. Failure within first 10 days is an even rarer subset. In the present case, the patient was pain-free and mobile, doing active physiotherapy during the 1st week post-operatively. The immediate post-operative X-ray did not show any hardware problem. Hence, the failure could have been due to improper coupling of the inner nut and the pedicle screw similar to the reported case by Aggarwal where the failure occurred after 1 year of surgery [11]. In the present case, the laminotomy on one side with a fixation on the contralateral side could have made the fixation unstable and may have been the plausible cause of such an early failure. The obesity of the patient and early mobilization could have contributed to the early failure of the fixation. In hindsight, we believe quantification of quality of patient’s bone could have been done pre-operatively. The patient was subsequently reoperated with three level vertebral fixations as it is reported to give additional stability, particularly in case of a compromised bone architecture and quality [12].
Conclusion
Early rod loosening and migration are a rare phenomenon in lumbar pedicle screw fixation. Meticulous and precise pre-operative planning and surgical techniques may avert such complications. Fixation in the present case should have been planned as bilateral transpedicular fixation of L4-L5-S1 vertebral bodies. The omission of insertion of the L5 pedicular screw during the planned bilateral transpedicular fixation had necessitated the screws in L4-L5-S1 for appropriate fixation in index surgery. This case highlights the fact that though unilateral fixation is a reported treatment for spondylolisthesis, proper case selection is crucial. Conditions such as obesity and osteoporosis need to be considered, and preferably, bilateral fixation should be done for such cases.
Clinical Message
Unilateral pedicle screw fixation for DS is a well-reported and established technique. However, proper patient selection is a necessity to avoid unforeseen early complications such as implant failure. Obesity and osteoporosis must be taken into account before proceeding with such fixations. Even post-operative physiotherapy protocols should be individualized depending on these factors.
References
1. Eliades P, Rahal JP, Herrick DB, Corliss BM, Riesenburger R, Hwang S, et al. Unilateral pedicle screw fixation is associated with reduced cost and similar outcomes in selected patients undergoing minimally invasive transforaminal lumbar interbody fusion for L4-5 degenerative spondylolisthesis. Cureus 2015;7(2):e249.1. Eliades P, Rahal JP, Herrick DB, Corliss BM, Riesenburger R, Hwang S, et al. Unilateral pedicle screw fixation is associated with reduced cost and similar outcomes in selected patients undergoing minimally invasive transforaminal lumbar interbody fusion for L4-5 degenerative spondylolisthesis. Cureus 2015;7(2):e249.
2. Hua YJ, Wang RY, Guo ZH, Zhu LM, Lu JY. Treatment of lumbar instability with transforaminal lumbar interbody fusion (with single cage) combined with unilateral pedicle screw fixation. Zhongguo Gu Shang 2014;27(9):722-725.
3. Kim TH, Lee BH, Moon SH, Lee SH, Lee HM. Comparison of adjacent segment degeneration after successful posterolateral fusion with unilateral or bilateral pedicle screw instrumentation: A minimum 10-year follow-up. Spine J 2013;13(10):1208-1216.
4. Aoki Y, Yamagata M, Ikeda Y, Nakajima F, Ohtori S, Nakagawa K, et al. A prospective randomized controlled study comparing transforaminal lumbar interbody fusion techniques for degenerative spondylolisthesis: Unilateral pedicle screw and 1 cage versus bilateral pedicle screws and 2 cages. J Neurosurg Spine 2012;17(2):153-159.
5. Meyerding HW. Spondylolisthesis. Surg Gynecol Obstet 1932;54:371-377.
6. Vaccaro AR, Garfin SR. Pedicle-screw fixation in the lumbar spine. J Am Acad Orthop Surg 1995;3(5):263-274.
7. Faraj AA, Webb JK. Early complications of spinal pedicle screw. Eur Spine J 1997;6(5):324-326.
8. Ohlin A, Karlsson M, Düppe H, Hasserius R, Redlund-Johnell I. Complications after transpedicular stabilization of the spine. A survivorship analysis of 163 cases. Spine (Phila Pa 1976) 1994;19(24):2774-2779.
9. Bayri Y, Eksi MS, Dogrul R, Koç DY, Konya D. Migration of rod into retroperitoneal region: A case report and review of the literature. Korean J Spine 2014;11(4):241-244.
10. Dhatt S, Kumar S, Arora N, Dhillon M, Tripathy SK. Migration of anterior spinal rod from the dorsolumbar spine to the knee: An unusual complication of spinal instrumentation. Spine (Phila Pa 1976) 2010;35(7):E270-E272.
11. Aggarwal A. Improper coupling between inner nut and screw head leading to rod loosening and dislodgement. Roman Neurosurg 2014;21(2):236-297.
12. Li CS. Three vertebral reduction and fixation for revision of lumbar spondylolisthesis. Zhongguo Gu Shang 2014;27:717-721.
 |
 |
 |
 |
| Dr. Prasoon Kumar | Dr. Vishal Kumar | Dr. Rakesh John | Dr. Rajbahadur Sharma |
| How to Cite This Article: Kumar P, Kumar V, John R, Sharma R. Early Loosening of Spinal Rod in a Case of Degenerative Grade 1 Spondylolisthesis treated with Unilateral Pedicle Screw Fixation and Transforaminal Cage for Interbody Fusion. Journal of Orthopaedic Case Reports 2017 Jul-Aug: 7(4): 6-9 |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com




