[box type=”bio”] What to Learn from this Article?[/box]
During clinical examination a bilateral shoulder dislocation presents with a fallacious symmetry of the shoulder girdle: sufficient diagnostics are needed to prevent a late-diagnosis and a non-detection of concomitant pathologies.
Case Report | Volume 7 | Issue 5 | JOCR Sep – Oct 2017 | Page 42-49| Kristian Nikolaus Schneider, Benedikt Schliemann, Salomon M Manz, Pranai K Buddhdev, Georg Ahlbäumer. DOI: 10.13107/jocr.2250-0685.890
Authors: Kristian Nikolaus Schneider [1], Benedikt Schliemann [2], Salomon M Manz [1], Pranai K Buddhdev [3], Georg Ahlbäumer [1]
[1] Department of Orthopaedics and Trauma Surgery, Klinik Gut, St. Moritz, Switzerland,
[2] Department of Trauma, Hand- and Reconstructive Surgery, University Hospital Münster, Münster, Germany,
[3] Department of Orthopaedics and Trauma Surgery, King’s College Hospital London, London, United Kingdom.
Address of Correspondence
Dr. Kristian Schneider, Hammerstraße 8, 48153 Münster, Germany.
E-mail: kristian.schneider.mh@gmail.com
Abstract
Introduction: Bilateral shoulder dislocations are rare and a diagnostic as well as a therapeutic challenge.
Case Report: We report the case of a 67-year-old male who fell while skiing and suffered a bilateral anterior shoulder dislocation associated with a four-part proximal humerus fracture on the left side and an osseous avulsion of the rotator cuff, a Pulley lesion, and a Hill–Sachs lesion on the right side. In addition, we searched the PubMed database using the terms “bilateral shoulder dislocation” and also “bilateral glenohumeral dislocation”. All retrieved matches were browsed for reports of bilateral anterior shoulder dislocations in patients aged 40 years or older. We identified and analyzed 35 case reports, including our own, regarding 20 male and 15 female patients with an average age of 58.9 years (female: 59.2 years, male: 58.6 years).
Conclusion: Elderly patients with a bilateral shoulder dislocation are at special risk for late diagnosis (five of 35 cases were not detected on the same day, but up to nine months later), concomitant pathologies (proximal humerus fractures were present in 19 cases; rotator cuff pathologies in seven cases), and insufficient diagnostic soft-tissue imaging (only four cases performed ultrasound/magnetic resonance imaging). Our reported case assembles a variety of possible concomitant pathologies. Through careful and comprehensive diagnostics all accompanying lesions were detected and subsequently addressed. The patient’s outcome shows that even in older patients with a combination of various bony, cartilaginous, muscular and ligamentous pathologies, good-to-excellent post-reductive and post-operative results are possible if diagnostics are comprehensive and treatment is prompt.
Keywords: Shoulder dislocation, Glenohumeral instability, Bilateral anterior shoulder dislocation, Shoulder dislocation in the elderly, Shoulder dislocation concomitant injuries, Shoulder dislocation winter sports.
Introduction
Anterior shoulder dislocation is a common injury with an incidence of 1.7% that frequently happens in contact-, overhead-, or winter sports [1]. Bilateral shoulder dislocations are by contrast rare, as the dislocating forces have to act on both shoulder joints synchronously and simultaneously [2]. We report the first case of a patient with a bilateral anterior shoulder dislocation in winter sports and its subsequent treatment. We also present a complete review of the English literature with 35 cases of bilateral anterior shoulder dislocations in patients aged 40 years and older focusing on the incidence and diagnostics of concomitant pathologies as well as the patient’s outcome. The patient’s age of 40 years and older was arbitrarily chosen by many authors to assess the “elder patient” in shoulder literature [3, 4, 5, 6].
Case Report
A 67-year-old sportive male (1.89 m; 95 kg) was referred to our trauma department by air ambulance after he fell while skiing crossover at a reasonable speed from deep snow back to the prepared slope – overseeing a significant step down of approximately 1 m. The patient unsuccessfully tried to break his fall but hit the snow with both extended arms straight over his head upfront. The patient’s past medical history excluded epilepsy, hypoglycemia, or any other possible seizure trigger.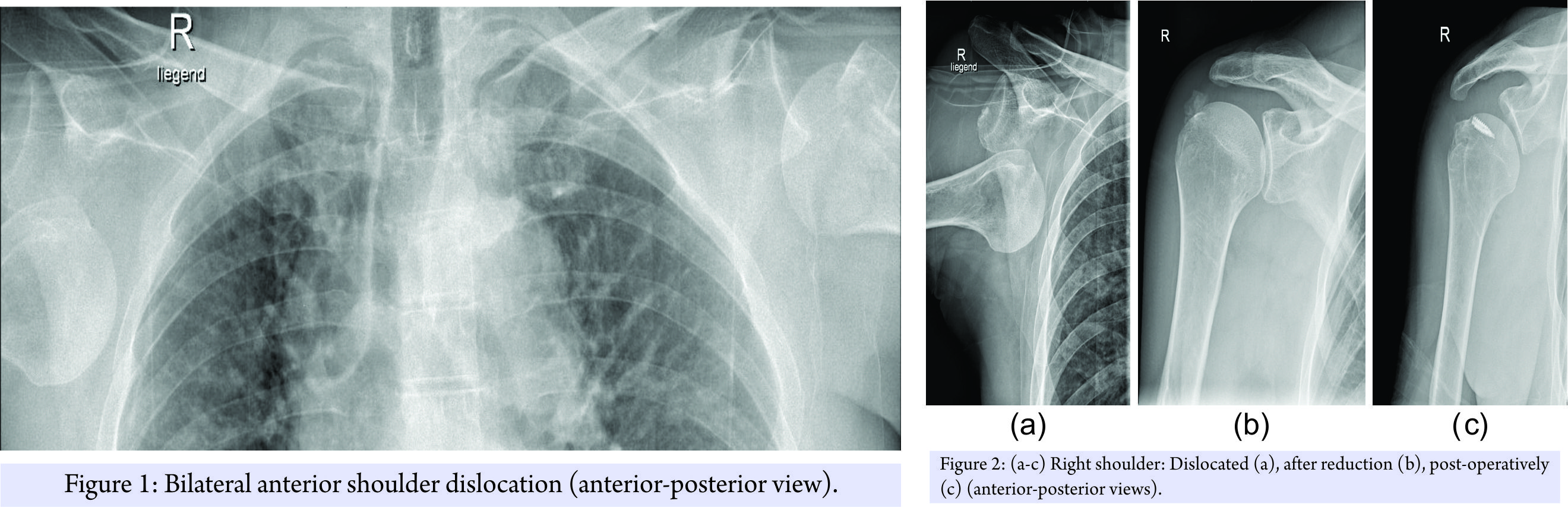
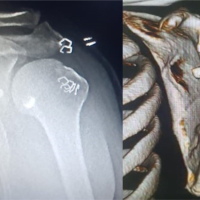
The patient was managed acutely on the slope and in our emergency room, according to ATLS principles, with a presenting GCS of 10 – E3V3M4. Full clinical examination was supplemented with imaging including a FAST scan and radiographs of shoulder joints, thorax, and pelvis. These confirmed the clinically suspected bilateral anterior shoulder dislocation combined with a four-part proximal humerus fracture on the left side and an osseous rotator cuff avulsion on the right side. The patient was neurovascular intact (Fig. 1, 2a and 3a).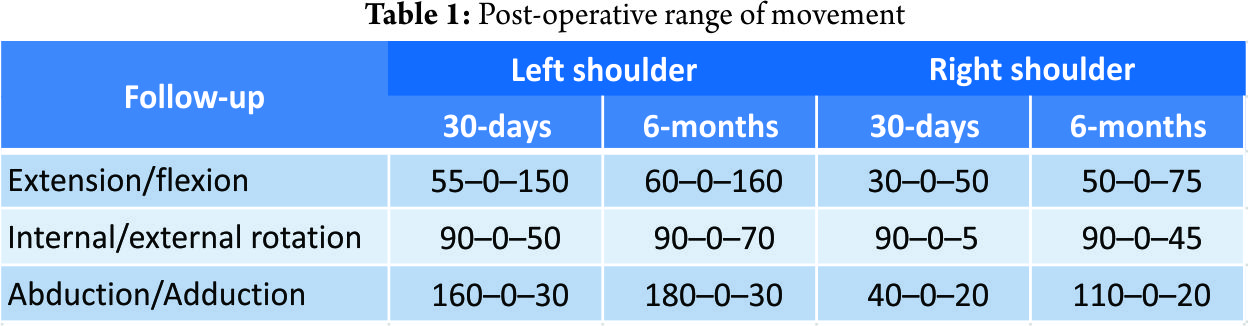
In the emergency room, both dislocations were consecutively reduced under sedation using the traction-counteraction-technique (Fig. 2b and 3b). No neurovascular deficit was detected post reduction. The right shoulder was immobilized in a Gilchrist bandage and the left shoulder in a Desault’s bandage before performing a computed tomography (CT)-scan of the head to successfully eliminate possible cerebral hemorrhage or skull vault injuries.
2 h after the accident, surgical treatment of the left four-part proximal humerus fracture was performed by minimally invasive plate osteosynthesis with a PHILOS® plate (Synthes; West Chester, USA). A central bone void was filled with an Allobone® allograft (Neutromedics AG; Charm, Switzerland) (Fig. 3c). An intra-operative diagnostic shoulder arthroscopy revealed no concomitant pathologies to the left shoulder joint, excluding any significant rotator-cuff injury, labral lesion, or chondral articular damage.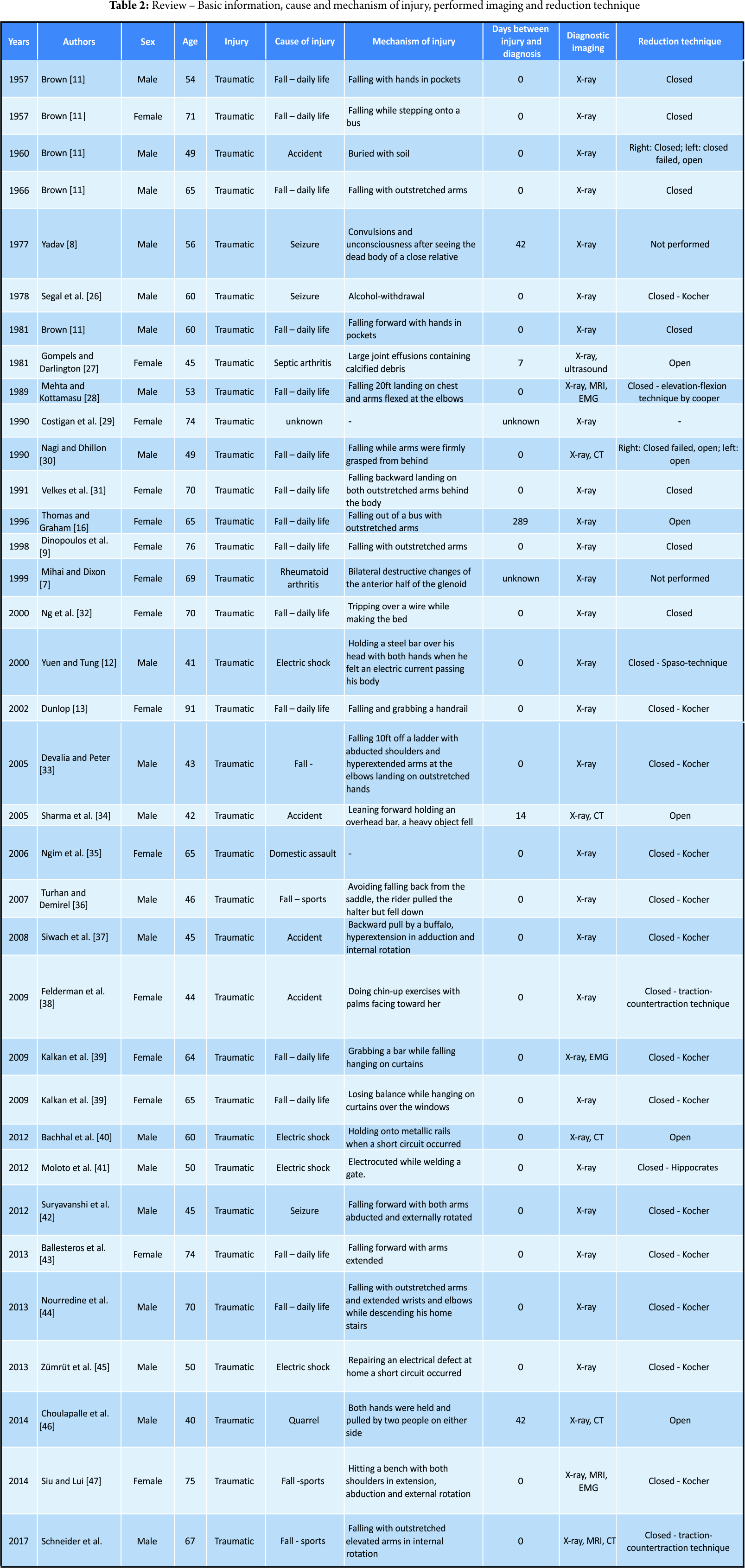
As the patients recovering progressed, a magnetic resonance imaging (MRI) scan of the right shoulder was performed 3-day post-injury to clarify the soft-tissue damage and subsequently a single-row rotator cuff repair using two 5.5 mm TwinFix® anchors (Smith & Nephew; London, United Kingdom) was performed. An additional Pulley-lesion was treated with a biceps tenodesis with fixation of the tendon to the intertubercular sulcus using a 5.5 mm Footprint® anchor (Smith & Nephew; London, United Kingdom). The Hill–Sachs lesion was insignificant and did not require any further treatment (Fig. 2c). Post-operatively, the left shoulder was immobilized in a Velpeau-sling for 4 weeks and the right shoulder in an abduction splint for 6 weeks. Passive mobilization of both shoulders was started immediately on the first post-operative day, followed by increasing active and assistive mobilization. On the right shoulder, progressive adduction and a steady build-up of strength were initiated after 6 weeks. On the left shoulder, full mobilization was allowed following clinical and radiological confirmation of fracture consolidation. Physiotherapy (3 times a week), aquatic therapy (2 times a week), and a 3-week stay in a rehabilitation facility 2-month post-injury completed the post-operative care. The patient was discharged in good general condition with a total inpatient stay of 11 days. The 30-day follow-up assessment showed a still restricted range of movement while the 6-month follow-up assessment demonstrated bilateral considerably improved range of movement (Table 1). At the 2-year follow-up assessment still no evidence of implant failure, recurrence of dislocation or instability was observed.
Materials and Methods
A comprehensive review of the English literature on bilateral anterior shoulder dislocations in patients aged 40 years or older was conducted. The PubMed database was searched using the terms “bilateral shoulder dislocation” and “bilateral glenohumeral dislocation.” All retrieved matches were browsed for reports of bilateral anterior shoulder dislocations in patients aged 40 years or older.
Results
Including this case (see “case report” above), we identified and analyzed 35 case reports regarding 20 male and 15 female patients with an average age of 58.9 years (female: 59.2 years, male: 58.6 years) (Tables 2 and 3).
Diagnostics
Thirty reported cases were traumatic, four cases atraumatic, and the reason for injury in one case remains unclear. Out of the 30 traumatic cases, 19 were due to a fall in everyday life, four cases due to an accident, four cases involved electric shocks and two patients due to assault. The four reported atraumatic cases were in two cases due to chronic arthritis (×1 septic arthritis, ×1 rheumatoid arthritis) and in addition two cases due to a seizure without any related fall or brunt.
Imaging
In all 35 cases, an X-ray examination was used to assess the shoulder joint pre- and post-reduction. A CT-scan for further fracture evaluation was performed in three cases. An MRI scan was performed in three and ultrasound imaging in one case. An EMG was also conducted in three reported cases.
Concomitant injuries
A total of 19 patients suffered a concomitant fracture of the proximal humerus (×8 bilateral, ×11 unilateral) ranging from a simple fracture of the greater tuberosity to a four-part humeral head fracture. Concomitant soft-tissue damage was discovered in nine patients with seven reported cases of rotator cuff tears (×2 bilateral, ×5 unilateral), two Hill–Sachs lesions, two Pulley-lesions, and six reported cases of injured nerves.
Reduction-technique
In 26 cases a closed reduction was performed (×13 Kocher technique, ×2 traction-counteraction technique, ×1 Hippocrates technique, ×1 Cooper technique, ×1 Spaso technique, and ×8 not specified), in four cases open reduction was performed, in two cases a bilateral closed reduction failed unilaterally and was subsequently performed in an open approach. In another two cases, no reduction was performed as the situations were chronic and an initial reduction unpromising [7, 8].
Post-reductive immobilization
In total, 24 of 35 reports (69%) documented the post-reductive immobilization instructions of both upper extremities. The different immobilization schemes varied greatly in type and duration: 22 cases (92%) report a type of sling immobilization – ranging from a Velpeau – sling and the similar “broad arm sling” to an abduction sling. In two cases (8%), body strapping was used to immobilize both shoulder joints. The duration of immobilization ranged from as short as 2 days to 6 weeks.
Discussion
Unilateral anterior shoulder dislocation is the most frequent joint dislocation in the human body [9]. The dislocation requires a set mechanism of injury: Forced extension, abduction, and external rotation leading the humeral head to dislocate into anterior direction [9, 10]. The dislocation is common in contact-, overhand-, and winter sports when a skier or snowboarder tries to prevent a fall. Bilateral shoulder dislocations are by contrast rare and – in sharp contrast to unilateral shoulder dislocations – not mainly due to a sports trauma but often described as the result of a seizure or electric shock, when the stronger internal rotator muscles outmatch the weaker external rotators in contraction resulting in a strong adduction and internal rotation forcing the humeral head to dislocate posteriorly [11, 12, 13, 14]. Even less frequent than bilateral posterior shoulder dislocations are bilateral anterior shoulder dislocations – <80 cases of this lesion have been reported in English literature. Although winter sports account for a majority of unilateral shoulder dislocations, there has been no case in the literature reporting on a bilateral anterior shoulder dislocation [15].
Diagnostics
The rarity of this lesion and the fallacious symmetry of the shoulder girdle during the clinical examination – as opposed to the typical asymmetry in the frequent unilateral dislocation – exacerbate the diagnosis of a bilateral shoulder dislocation. Dunlop reported that more than 10% of all bilateral shoulder dislocations are not diagnosed immediately. In our review, the patient did not always remember the date of injury, so that only in 33 of 35 reports the interval between injury and diagnosis could be defined. Although in 28 of these 33 cases (85%) the diagnosis was made on the same day, four cases (12%) remained undetected for up to 6 weeks. One case was not diagnosed for over 9 months [13, 16]. Due to the frequent cause of seizure as a trigger of bilateral shoulder dislocations, a careful anamnesis for any history of epilepsy or hypoglycemia should always be conducted and was performed in 17 of 35 cases (49%) [11, 17].
Concomitant Injuries
Patients with a shoulder dislocation are at special risk for concomitant pathologies. While damage to the labrum is more prominent in younger patients, fractures, and especially rotator cuff tears become more frequent in elder patients [18, 19, 20]. Nineteen of our 35 reviewed bilateral shoulder dislocations (54%) were accompanied by a unilateral (×11) or bilateral (×8) proximal humerus fracture – ranging from a simple fracture of the greater tuberosity to a four-part humeral head fracture. Simank et al. have shown that with increasing patient’s age, the incidence of concomitant rotator cuff tears increases, too and is omnipresent in patients aged 70 years or older. In addition, Pevny et al. report the significant negative impact of concomitant rotator cuff tears – present in 35% of their patients – on the outcome of their reviewed patients aged 40 years or older [4]. In our review, rotator cuff pathologies were only detected in seven cases (20%) – five unilaterally and two bilaterally. Taking into account that one case of bilateral shoulder dislocation consists of two affected shoulders, there are only nine diagnosed rotator cuff tears (13%) in a total of 70 individual dislocated shoulder joints. Despite this high risk, the relevant diagnostic imaging such as ultrasound or MRI was only performed in four cases (11%) – including our own case. Therefore, a high number of undetected rotator cuff lesions must be assumed due to insufficient diagnostic measures. To detect concomitant injuries, we suggest performing an ultrasound or MRI scan in all elderly patients presenting with an anterior shoulder dislocation.
Treatment
The pre-reduction radiograph is necessary to assess the humeral head and to detect possible fractures that could be worsened through an impetuous try of reduction while the post-reductive X-ray confirms a successful reposition and allows the second elimination of possible fractures. Furthermore, Kahn and Mehta and Kottamasu have shown that 37.5% of all concomitant fractures in shoulder dislocations were only seen on a post-reductive X-ray [20, 21]. Numerous techniques of closed reduction have been described in the literature, but no universal approach has been found yet. The Kocher technique and variations of the traction-counteraction technique of Hippocrates remain the most popular performed with the Kocher technique being applied in every second case (×13) of initial closed reductions (×26) in our review. However, Dala-Ali et al. highlighted the various complications of the traditional reduction techniques and recommend modern alternatives such as the FARES technique [5, 22]. In two reported cases, the initial closed reduction failed and was subsequently performed open, and in another two cases, an initial and successful open reduction was performed. An immediate but careful reduction is vital to prevent damage to the brachial plexus and rotator cuff muscles as delayed repositions are associated with permanent nerve damage, reduced mobility, and a higher risk for re-dislocation [16].
Immobilization
Following a successful reduction, immobilization with regard to concomitant injuries and the patient’s compliance is necessary. About 92% of all reviewed cases use a form of sling immobilization that is especially challenging when done bilaterally in internal rotation. A seldom but possible danger of a sling immobilization in the elder population are skin pressure ulcer in the head and neck area. A careful physical examination during follow-up visits is vital to prevent this deuteropathy [23].
Outcome
Eleven reviewed cases (31%) report a full recovery bilaterally, whereas twelve cases (34%) report a restricted range of movement bilaterally. Three cases (9%) report both: A restriction in one shoulder and a full recovery in the other. Five reports (14%) remain vague on the patient’s outcome as statements like “reasonable resumption of painless arm movement” or “adequate recovery” let suspect a neither quantified nor published restricted range of movement. No follow-up results were published in four case reports (11%). Out of the fifteen cases with post-reductive restricted range of movement only two cases (13%) have used ultrasound or an MRI scan to assess the rotator cuff. In the remaining 13 reports (87%), the further diagnostic was not considered necessary. Hawkins et al. strengthen the influence of previously undetected rotator cuff tears in patients with an unsatisfying outcome. They have re-evaluated 14 patients with persistent “pain, weakness and functional problems despite an aggressive physiotherapy program” following a shoulder dislocation and discovered in all cases a previously unknown rotator cuff tear [5]. Sonnabend et al. further support this finding in a re-assessment of 13 patients aged 40 years or older who “continued to experience pain and varying degrees of associated weakness” after a primary anterior shoulder dislocation. The authors found “evidence of full-thickness cuff disruption” in all 13 patients – surgical repair was performed in five patients who became subsequently “virtually pain-free” [6]. This emphasizes the need for additional diagnostic imaging such as ultrasound or MRI scans.
Conclusion
Bilateral anterior shoulder dislocations in patients aged 40 years or older are frequently accompanied by proximal humeral head fractures or soft-tissue injuries, especially rotator cuff tears. While the first-mentioned fractures are detectable on the pre- or post-reductive X-ray, the latter-mentioned soft-tissue pathologies are often overseen as required clinical test and imaging are not performed. However, these concomitant injuries – especially the rotator cuff tears – have a significant influence on the outcome [5, 6, 18, 19, 24, 25]. We have shown that soft-tissue imaging was only performed in a total of five of all 35 reviewed cases (14%) and only in two of 15 (13%) cases where a bilateral or unilateral restricted range of movement was present. Even in cases with a significant post-reductive restricted range of movement in rotation and abduction was present, no further diagnostics were conducted and the patient’s poor outcome accepted. Furthermore, we have shown that the previously reported high rate of late diagnosis in bilateral shoulder dislocations is even higher in elder patients suffering from this lesion (15%). Our reported case of bilateral anterior shoulder dislocation assembles a variety of possible concomitant pathologies. Through careful and comprehensive diagnostics all accompanying lesions were detected and subsequently addressed within 5-day post-injury. The patient’s outcome shows that even in older patients with a combination of various bony, cartilaginous, muscular and ligamentous pathologies, good-to-excellent post-reductive and post-operative results are possible if diagnostics are comprehensive and treatment is prompt. In addition, we report the first bilateral shoulder dislocation in winter sports, despite winter sports accounting for a majority of unilateral shoulder dislocations.
Clinincal Message
Comprehensive anamnesis – excluding seizure as a possible trigger – and diagnostics – including soft tissue imaging – are necessary in patients with bilateral anterior shoulder dislocation aged 40 years or older not only to prevent a late diagnosis but also a non-detection of concomitant pathologies that can negatively affect the patient’s outcome. Particularly in cases with post-reductive restricted range of movement, the rotator cuff integrity has to be evaluated.
References
1. Hovelius L. Incidence of shoulder dislocation in Sweden. Clin Orthop Relat Res 1982;166:127-31.
2. Tripathy SK, Sen RK, Aggarwal S, Dhatt SS, Tahasildar N. Simultaneous bilateral anterior shoulder dislocation: Report of two cases and review of the literature. Chin J Traumatol 2011;14:312-5.
3. Paxton ES, Dodson CC, Lazarus MD. Shoulder instability in older patients. Orthop Clin North Am 2014;45:377-85.
4. Pevny T, Hunter RE, Freeman JR. Primary traumatic anterior shoulder dislocation in patients 40 years of age and older. Arthroscopy 1998;14:289-94.
5. Hawkins RJ, Bell RH, Hawkins RH, Koppert GJ. Anterior dislocation of the shoulder in the older patient. Clin Orthop Relat Res 1986;206:192-5.
6. Sonnabend DH. Treatment of primary anterior shoulder dislocation in patients older than 40 years of age. Conservative versus operative. Clin Orthop Relat Res 1994;304:74-7.
7. Mihai R, Dixon JH. Bilateral atraumatic dislocation of the shoulder. J Accid Emerg Med 1999;16:460.
8. Yadav SS. Bilateral simultaneous fracture-dislocation of the shoulder due to muscular violence. J Postgrad Med 1977;23:137-9.
9. Dlimi F, Rhanim A, Lahlou A, Kharmaz M, Ouadghiri M, El-Bardouni A, et al. Bilateral anterior dislocation of the shoulders at the start of a backstroke competition. J Orthop Traumatol 2012;13:47-9.
10. Dinopoulos HT, Giannoudis PV, Smith RM, Matthews SJ. Bilateral anterior shoulder fracture-dislocation. A case report and a review of the literature. Int Orthop 1999;23:128-30.
11. Brown RJ. Bilateral dislocation of the shoulders. Injury 1984;15:267-73.
12. Yuen MC, Tung WK. The use of the spaso technique in a patient with bilateral dislocations of shoulder. Am J Emerg Med 2001;19:64-6.
13. Dunlop CC. Bilateral anterior shoulder dislocation–a case report and review of the literature. Acta Orthop Belg 2002;68:168-70.
14. Meena S, Saini P, Singh V, Kumar R, Trikha V. Bilateral anterior shoulder dislocation. J Nat Sci Biol Med 2013;4:499-501.
15. Ogawa H, Sumi H, Sumi Y, Shimizu K. Glenohumeral dislocations in snowboarding and skiing. Injury 2011;42:1241-7.
16. Thomas DP, Graham GP. Missed bilateral anterior fracture dislocations of the shoulder. Injury 1996;27:661-2.
17. Mathis RD. Bilateral shoulder dislocation: An unusual occurrence. J Emerg Med 1990;8:41-3.
18. Simank HG, Dauer G, Schneider S, Loew M. Incidence of rotator cuff tears in shoulder dislocations and results of therapy in older patients. Arch Orthop Trauma Surg 2006;126:235-40.
19. Breitenseher MJ, Pones M, Breitenseher JB. Systematics of injuries of the rotator cuff and biceps tendon. Radiologe 2015;55:221-30.
20. Ferkel RD, Hedley AK, Eckardt JJ. Anterior fracture-dislocations of the shoulder: Pitfalls in treatment. J Trauma 1984;24:363-7.
21. Kahn JH, Mehta SD. The role of post-reduction radiographs after shoulder dislocation. J Emerg Med 2007;33:169-73.
22. Dala-Ali B, Penna M, McConnell J, Vanhegan I, Cobiella C. Management of acute anterior shoulder dislocation. Br J Sports Med 2014;48:1209-15.
23. Radha S, Vaghela KR, Konan S, Radford W. Polysling skin pressure necrosis–a complication of shoulder immobilisation. BMJ Case Rep 2012;2012. pii: bcr2012006671.
24. Teunis T, Lubberts B, Reilly BT, Ring D. A systematic review and pooled analysis of the prevalence of rotator cuff disease with increasing age. J Shoulder Elbow Surg 2014;23:1913-21.
25. Maman E, Dolkart O, Chechik O, Amar E, Rak O, Rath E, et al. Arthroscopic findings of coexisting lesions with greater tuberosity fractures. Orthopedics 2014;37:e272-7.
26. Segal D, Yablon IG, Lynch JJ, Jones RP. Acute bilateral anterior dislocation of the shoulders. Clin Orthop Relat Res 1979;140:21-2.
27. Gompels BM, Darlington LG. Septic arthritis in rheumatoid disease causing bilateral shoulder dislocation: Diagnosis and treatment assisted by grey scale ultrasonography. Ann Rheum Dis 1981;40:609-11.
28. Mehta MP, Kottamasu SR. Anterior dislocation of the shoulders with bilateral brachial plexus injury. Ann Emerg Med 1989;18:589-91.
29. Costigan PS, Binns MS, Wallace WA. Undiagnosed bilateral anterior dislocation of the shoulder. Injury 1990;21:409.
30. Nagi ON, Dhillon MS. Bilateral anterior fracture dislocation of the shoulders. J Orthop Trauma 1990;4:93-5.
31. Velkes S, Lokiec F, Ganel A. Traumatic bilateral anterior dislocation of the shoulders. A case report in a geriatric patient. Arch Orthop Trauma Surg 1991;110:210-1.
32. Ng AB, Rix TE, Roy BR. Acute bilateral anterior dislocations of the shoulders. Ulster Med J 2000;69:171-2.
33. Devalia KL, Peter VK. Bilateral post traumatic anterior shoulder dislocation. J Postgrad Med 2005;51:72-3.
34. Sharma L, Pankaj A, Kumar V, Malhotra R, Bhan S. Bilateral anterior dislocation of the shoulders with proximal humeral fractures: A case report. J Orthop Surg (Hong Kong) 2005;13:303-6.
35. Ngim NE, Udorroh EG, Udosen AM. Acute bilateral anterior shoulder dislocation following domestic assault–case report. West Afr J Med 2006;25:256-7.
36. Turhan E, Demirel M. Bilateral anterior glenohumeral dislocation in a horse rider: A case report and a review of the literature. Arch Orthop Trauma Surg 2008;128:79-82.
37. Siwach R, Singh R, Rohilla R, Sangwan SS. Bilateral anterior dislocation of the shoulder. A case report and review of the literature. Injury Extra 2008;39:394-7.
38. Felderman H, Shih R, Maroun V. Chin-up-induced bilateral anterior shoulder dislocation: A case report. J Emerg Med 2009;37:400-2.
39. Kalkan T, Demirkale I, Ocguder A, Unlu S, Bozkurt M. Bilateral anterior shoulder dislocation in two cases due to housework accidents. Acta Orthop Traumatol Turc 2009;43:260-3.
40. Bachhal V, Goni V, Taneja A, Shashidhar BK, Bali K. Bilateral four-part anterior fracture dislocation of the shoulder–a case report and review of literature. Bull NYU Hosp Jt Dis 2012;70:268-72.
41. Moloto M, Mungulu B, Golele S. Bilateral anterior glenohumeral fracture dislocation. SA Orthop J 2012;11:88-92.
42. Suryavanshib A, Mittal A, Dongre S, Kashyap N. Bilateral anterior shoulder dislocation with symmetrical greater tuberosity fracture following seizure. J Orthop Case Rep 2012;2:28-31.
43. Ballesteros R, Benavente P, Bonsfills N, Chacon M, Garcia-Lazaro FJ. Bilateral anterior dislocation of the shoulder: Review of seventy cases and proposal of a new etiological-mechanical classification. J Emerg Med 2013;44:269-79.
44. Nourredine H, El-Sayad M, Gull S, Davies AP. Bilateral anterior shoulder dislocation. BMJ Case Rep 2013;2013. pii: bcr2012008308.
45. Zümrüt M, Marcil E. Bilateral shoulder injury caused by electric shock. JAEMCR 2013; 4:92-4.
46. Choulapalle R, Kolluri RK, Anne SR, Perumal SR, Avadhanam PK, Bheemanathuni R. A case of neglected bilateral anterior shoulder dislocation: A rare entity with unusual mechanism of injury. Case Rep Orthop 2015;2015:461910.
47. Siu YC, Lui TH. Bilateral anterior shoulder dislocation. Arch Trauma Res 2014;3:e18178.
 |
 |
 |
 |
 |
| Dr. Kristian Nikolaus Schneider |
Dr. Benedikt Schliemann |
Dr. Salomon Manz |
Dr. Pranai Buddhdev |
Dr. Georg Ahlbäumer |
| How to Cite This Article: Schneider KN, Schliemann B, Manz SM, Buddhdev PK, Ahlbäumer G. Bilateral Anterior Shoulder Dislocation in the Elderly – A Case Report and Review of the Literature. Journal of Orthopaedic Case Reports 2017 Sep-Oct;7(5):42-49 |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com