[box type=”bio”] Learning Points for this Article: [/box]
To know the 3 aspects of this disease presented together and the minimally invasive treatment.
Case Report | Volume 7 | Issue 6 | JOCR November – December 2017 | Page 68-72| Coulibaly Ndeye Fatou, BA Amadou, Gueye Alioune Badara, Dembele Badara, Daffe Mohamed, Dieme Charles Bertin. DOI: 10.13107/jocr.2250-0685.954
Authors: Coulibaly Ndeye Fatou [1], BA Amadou [1], Gueye Alioune Badara [1], Dembele Badara [1], Daffe Mohamed [1], Dieme Charles Bertin [1]
[1] Department of Orthopedics Traumatology, CHU Aristide le DANTEC, Dakar, Senegal.
Address of Correspondence:
Dr. Coulibaly Ndeye Fatou,
Service d’Orthopédie-Traumatologie C.H.U. Le DANTEC, Dakar,
Sénégal, B.P: 5994 Dakar Fann.
E-mail: nfcoulibaly@yahoo.fr
Abstract
Introduction: Tuberculous tenosynovitis localization is rare. This unusual presentation, often misunderstood, results in frequent misdiagnosis. We report 4 cases of patients which represent the 3 anatomo-clinical forms described by Kanavel. The knowledge of its different manifestations will make it possible to recognize and to suspect the tuberculous origin.
Case Report: This was a retrospective study from January 2006 to May 2017 which involved all patients received and treated with tuberculous tenosynovitis. Of the 4 case studies presented here, there were 3 men and 1 woman, aged, respectively, 23, 30, 40, and 30 years of age. They were all immunocompetent. The onset was, respectively, about 12, 6, 4, and 8 months. The localization was on the wrist for 3 cases (2 on the right and 1 on the left) and one on the palmar face of the second ray on the right hand. Signs of median nerve compression were found in 2 cases. Surgery was extensive, with a complete debridement in 3 patients. For the last one, a simple recess was made associated with a bacteriological sampling. Biopsy was performed for all patients. In the anatomo-clinical study, we observed 1 case of serofibrinous synovitis, 2 cases of rice-like synovitis, and 1 case of caseous synovitis. A rupture of the tendon of the flexor carpi radialis was observed in 1 case. All cases were confirmed histologically with the presence of granuloma gigantocellular with caseous necrosis. We have recorded 1 case of bacteriological positivity in 3 cases requested. Patients had antituberculous chemotherapy after surgery for, respectively, 6, 8, 6, and 8 months. The progression was favorable with a regression of the signs of nerve compression. Revisited at, respectively, 4, 3, 5 years, and 34 months, we did not record any recurrence. The mobility of the wrist was complete and partial for the finger.
Conclusion: Tenosynovitis tuberculous treatment is mostly medical. Early diagnosis enables the treatment to be started as soon as possible to avoid extensive surgery. For this reason, it is currently essential to use high sensitivity diagnostic methods of such as the polymerase chain reaction method and the Genexpert in any suspicion of the disease.
Keywords: Tenosynovitis, tuberculous, caseous, wrist, hand, Genexpert, polymerase chain reaction.
Introduction
Tuberculous tenosynovitis is a rare form of tuberculosis and accounts for 0.7–1% of osteoarticular tuberculosis which involvement accounts for 3–5% of all localized tuberculosis infections [1, 2]. The most common localization is on the wrist [1, 2, 3]. Its chronic and insidious evolution, long supported by patients, is one explanation for delays in consultation [4]. On the other hand, this unusual presentation, often misunderstood, also results in frequent misdiagnosis and is another explanation for therapeutic delay. The incorrect prescription of corticosteroids with deleterious effects aggravates and exacerbates the progression of tuberculosis infection [5]. If tuberculosis is common and remains one of the most feared diseases in developing countries, its spread in developed countries is largely associated with human immunodeficiency virus infection. The diagnosis is based on bacteriology by demonstration of the Koch bacillus and/or histological diagnosis. The treatment is medicosurgical including antituberculous, chemotherapy, and debridement for diagnostic and therapeutic purposes [2, 6, 7, 8]. We report 4 cases of patients which represent the 3 anatomo-clinical forms described by Kanavel [9] in tuberculous tenosynovitis of the wrist and the hand, the different treatments applied to them and their results.
Case Report
This was a retrospective study from January 2006 to May 2017 which involved all patients received and treated with tuberculous tenosynovitis. Of the 4 case studies presented here, there were 3 men and 1 woman. They were all immunocompetent and reported a history of BSG vaccination was performed in childhood.
Patient 1
Mr HF, 23-year-old, consulted for a painful swelling of the left wrist. The onset was about 1 year after the progressive installation of a painless swelling of the left wrist. The clinical findings included swollen wrist in the dorsolateral side, with a pre-fistulized lesion and scarification zones made by bonesetters. Palpation was not painful and the mobilization of the fingers was normal. There were no radiological bone lesions. Surgical exploration showed hypertrophy of the synovial sheath of the extensors of the fingers with the presence of caseous lumps (Fig. 1). Debridement with synovial resection was performed. The outcome was favorable. The anatomopathological examination revealed an epithelial-gigantocellular granuloma with caseous necrosis or tubercular granuloma. An antibacillary quadritherapy based on rifampicin (R), isoniazid (H), ethambutol (E), and pyrazinamide (Z) for 2 months and an HR-based combination for 4 months was administered. The progression was favorable and after a 4-year follow-up, no recurrence was observed.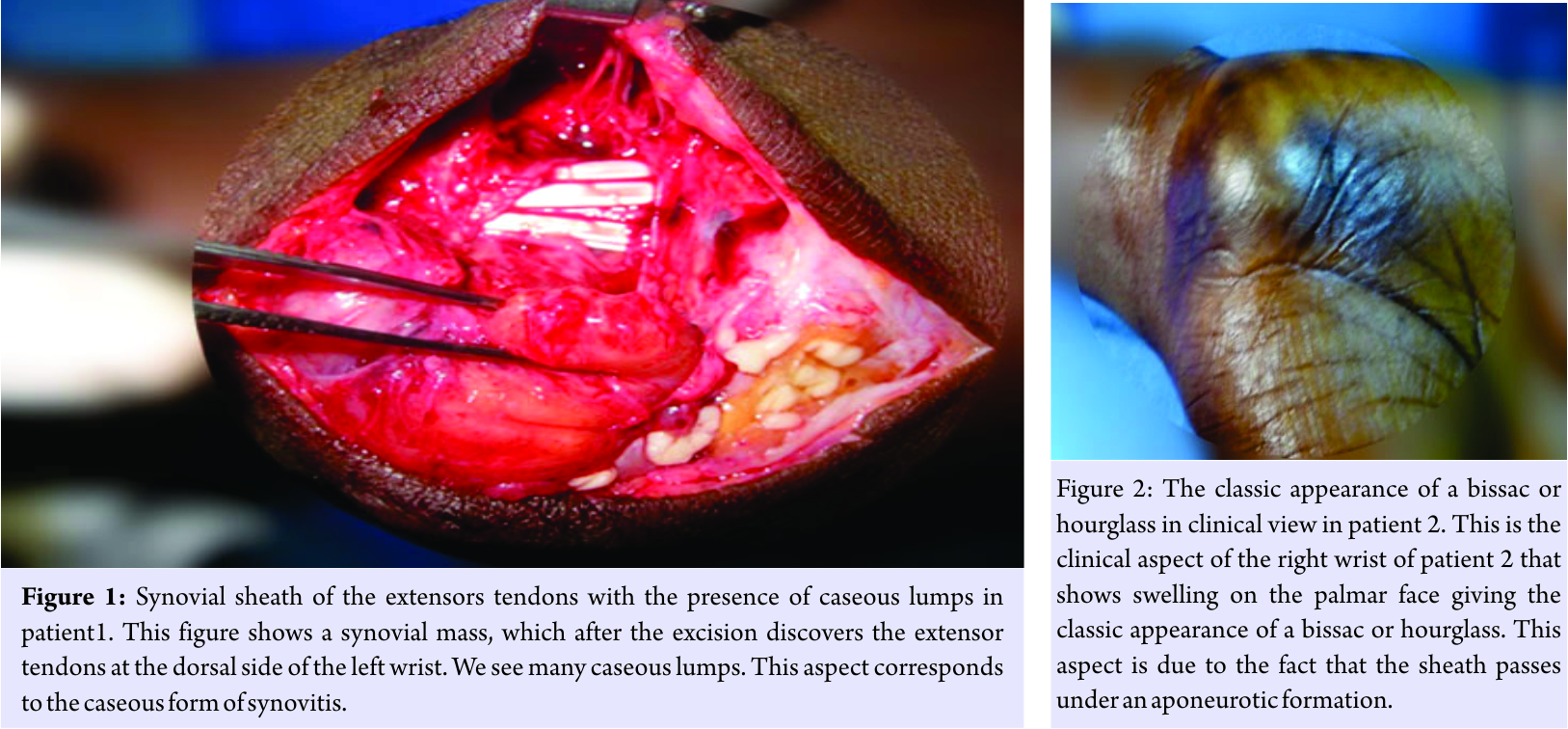
Patient 2
Ms DN, 30-year-old, consulted for a tumefaction of the palmar face of the right wrist progressing progressively for 6 months. The patient presented paresthesias at the level of the first three fingers and reported treatment by injection with corticosteroids 3 months before the date of consultation. The clinical examination revealed swelling on the palmar face giving the classic appearance of a bissac or hourglass. Palpation was not painful. The Tinel’s sign and the sign of Phalen’s sign were positive. The radiograph of the wrist showed a densification of the soft parts. In perioperative operation, there was a large synovial mass passing through the carpal tunnel (Fig. 2). It contained at the opening some firm riziform grains. A release of the median nerve was achieved. At the exploration, a rupture of the tendon of the flexor carpi radialis was observed (Fig. 3). Synovial resection was performed. Only the pathological examination was requested and showed a tubercular granuloma. Medical treatment based on four molecules (ERHZ) was administered for 2 months for the initial phase followed by a bitherapy based on RH for 6 months. The evolution was favorable with a complete recovery of wrist mobility. After 3 years, the patient was lost to follow-up.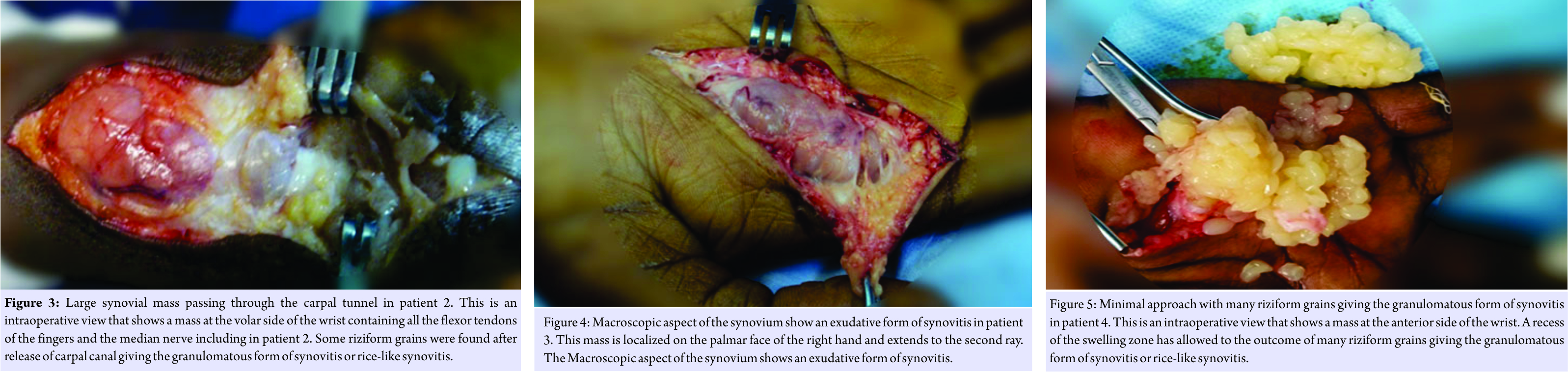
Patient 3
Mr. MD aged 40 years is an accounting officer with no reported tuberculosis history. He had consulted for a tumefaction on the palmar face of the second ray on the right hand. The active and passive mobility of the 2nd ray was limited with a distance palm to 5 cm. He had no axillary adenopathies. The radiograph (X-ray) of the hand and wrist showed no bone damage, and the radiograph (X-ray) lungs were normal. Ultrasound suggested a diagnosis of tenosynovitis. The intradermal reaction to tuberculin was positive at 18 mm. Macroscopic aspect of the synovium was an exudative form of Kanavel [9] (Fig. 4). A synovectomy with synovial biopsy was performed. Anatomopathological examination revealed a tubercular granuloma. An antituberculosis therapy was performed on the basis of RHE for 2 months followed by a maintenance treatment made of RH for 4 months. Functional rehabilitation had enabled a complete passive mobility. As for the active one, it persisted a palm pulp distance of 2 cm after 5-year follow-up.
Patient 4
Mr. IS is, 20-year-old, a driver, presented a swelling of spontaneous and progressive installation of the palmar face of the right hand evolving for 8 months. Clinical examination found a palpate swelling in bissac on the palmar side of 6 cm by 3, painful, elastic, and renitent with crepitus feeling at the alternating pressure of the two zones of swelling. He had paresthesia on the 3rd finger. No pathological ganglionic areas were found. Sedimentation rate and blood count were normal. The intradermal reaction to tuberculin was positive at 20 mm. The radiograph (X-ray) of the hand showed no bone damage and the lungs were normal. Ultrasound revealed tenosynovitis with the presence of grains. A synovial biopsy per 2 cm palmar approach to the distal part of the mass was performed. The tendon sheaths had a hypertrophied appearance. After an incision of the sheath, we noted an outcome of many riziform grains giving the granulomatous form of synovitis (Fig. 5). A recess of the swelling zone was made associated with a synovial biopsy and a bacteriological sampling. The anatomopathological examination had found a tubercular granuloma. Bacteriological examination of the sampling fluid was negative on direct examination and culture. Triple antituberculosis antibiotics combining RHE were prescribed during 2 months followed by HR-based combination therapy for 6 months. The progression was favorable with a regression of the signs of nerve compression. Revisited at 34 months, we did not record any recurrence. The mobility of the fingers and the wrist is complete.
Discussion
Tuberculous tenosynovitis is a rare form of tuberculosis. In 10 years, only 4 cases located at the level of the hand and the wrist were diagnosed in the department of orthopedic surgery. This rarity is mirrored in all published case studies with a number rarely exceeding 2 cases per study [3, 7, 8, 10, 11]. Our patients consulted late, at 5 months or even more than a year after the onset of the disease. Tuberculous tenosynovitis is marked by an insidious and progressive onset and the swelling becomes evident after several months. This makes a high tolerance of the disease. The clinician, on the other hand, rarely, considers the diagnosis of tuberculosis when faced with a case of tenosynovitis. The diagnosis is most often confused with a rheumatic pathology for which corticotherapy is often prescribed [5], as was the case of patient 2. These practices accelerate the progression of complications. In this patient, we observed a rupture of the flexor carpi radialis tendon after 6 months of evolution. Clinically, local inflammatory signs were discrete. Given the long course of the disease, swelling can evolve toward fistulization [9]. One of our patients showed a pre-fistulizating lesion. Carpal tunnel syndrome observed in 2 of our patients is often seen in palmar localization at the wrist [12]. In fact, hyperplasia of the synovial sheaths naturally leads to compression of the median nerve in the carpal tunnel, which they traverse with the tendon structures and the nerve. In both cases of palmar localization in the wrist, we found riziform grains inside the sheath. Biologically, the blood count is usually normal, but may sometimes show leukocytosis, as in the JARAA series [3]. The ultrasound was only requested in 2 patients and it was contributory. The latter should also be useful for performing an echo-guided puncture for bacteriological examination [10] and/or a polymerase chain reaction (PCR) study of the liquid removed from the lesion, as it may prevent the use of diagnostic surgery [12]. MRI is a highly useful and sensitive examination [12]. This examination did not exist in the country at the beginning of our study and for socioeconomic reasons; the last 2 patients could not afford to perform it. In our societies, most of the patients have no medical coverage, and then, they assume all costs of the treatment. All these diagnostics support a potential diagnosis of tuberculosis. However, the definitive diagnosis of certainty requires the detection of BK in the sampling fluid and/or histological evidence. We have recorded 1 case of bacteriological positivity in 3 cases requested. According to Kanavel [9], bacteriological evidence is present in direct examination only in 20% of cases and cultures are negative in 35–45% of cases. Indeed, the bacterial density is low in the synovial fluid and in the tendinous or synovial tissues [7]. This paucibacillary nature of the infection explains a large number of false negatives and the absence of BK in the cultures cannot and should not in any way invalidate the diagnosis. Molecular techniques, such as gene amplification methods (PCR), which was not available in our regions at the moment of our study, are more sensitive and allow rapid and specific detection of BK [1]. We have very recently the contribution of Genexpert which also, due to its very high specificity (97–100%), contributes highly to the diagnosis of tuberculosis. Hence, for us, these 2 examinations will be asked systematically in case of suspicion of this disease. In the anatomo-clinical aspect, we observed all the stages of the Kanavel classification [9]. We had 1 case of serofibrinous synovitis (patient 3), 2 cases of rice-like synovitis (patients 2 and 4), and 1 case of caseous synovitis (patient 1). All were confirmed histologically with the presence of granuloma gigantocellular with caseous necrosis. This histological evidence is found in the majority of studies [1, 3, 7, 8, 9, 10, 11]. All our patients had antituberculous chemotherapy self-reported after surgery. This surgery is most often extensive, with the goal of making a complete debridement [7]. In one patient, a simple recess was made associated with a bacteriological sampling and a biopsy. We describe this process as minimally invasive or conservative given its minimal approach. At the end of 34 months, no recurrence was noted. We believe that in the absence of signs of rupture of the tendinous or of confirmed compression syndrome, this treatment may be considered. It reduces the esthetic and especially functional sequelae due to the extent of the incision and the risks of tendon adhesion (patient 3). We recorded 1 case of tendon rupture (patient 2) which is frequent [9, 13]. This lesion occurs earlier in the case of corticosteroid treatment in our study. In our patients, the duration of medical treatment varied between 6 and 8 months. The progression was favorable with a minimum follow-up of 32 months for the last patient. The function of the wrist and the hand was excellent in all with a slight defect of winding of the index in patient 3. However, there is a significant risk of recurrence of osteoarticular tuberculosis and requires long-term monitoring [7, 14]. There are limitations to our study. First, its sample size was relatively small due to disease rarity. In the second part, this retrospective study represents patients for which the care was not standardized due to, for the two fist patients, tuberculous etiological disease was not suspected.
Conclusion
Tenosynovitis is a rare localization of tuberculosis. The treatment is both surgical and medical. The disease progression under treatment was toward healing in all our patients with a total functional recovery in 3 patients and partial in 1 case. We recommend in suspected cases, an early diagnosis which enables a treatment to be started as soon as possible to avoid complications such as tendon ruptures, joint damage, and extensive surgery. For this reason, it is currently essential to use high sensitivity diagnostic methods of such as the PCR method and the Genexpert in any suspicion of osteoarticular tuberculosis.
Clinical Message
Tuberculous tenosynovitis localization is rare. This unusual presentation, often misunderstood, results in frequent misdiagnosis. We report 4 cases of patients which represent the 3 anatomo-clinical forms described by Kanavel. The knowledge of its different manifestations will make it possible to recognize and to suspect the tuberculous origin.
References
1. Astudillo L, Garrousteb C, Chabrolc A, Saillerd L. Tuberculous tenosynovitis: A currently rare presentation of tuberculosis. Rev Méd Interne 2007;28:160-83.
2. Walker UA, Gutfleisch J, Peter HH. Tuberculous tenosynovitis. Ann Rheum Dis 2002;61:384.
3. Jaraa M, Qacifa H, Sekkacha Y, El Qatnia M, Elouennassb M, Ghafira D. Tuberculous Tenosynovitis: A rare localization. Rev Méd Interne 2007;28:56-8.
4. Kriegs-Au G, Ganger R, Petje G. The sequelae of late diagnosis in tuberculous flexor tenosynovitis of the hand-A report of 2 cases. Acta Orthop Scand 2003;74:221-4.
5. Barnes PF, Bloch AB, Davidson PT, Snider DE Jr. Tuberculosis in patients with human immunodeficiency virus infection. N Engl J Med 1991;324:1644-50.
6. Fellander M. Tuberculous tenosynovitis of the hand treated by combined surgery and chemotherapy. Acta Chir Scand 1956;111:142-50.
7. Aboudola S, Sienko A, Carey RB, Johnson S. Tuberculous tenosynovitis. Hum Pathol 2004;35:1044-6.
8. Sanders CJ, Schucany WG. Tuberculous tenosynovitis. Proc (Bayl Univ Med Cent) 2008;21:71-2.
9. Kanavel AB. Tuberculous tenosynovitis of the hand: A report of 14 cases. Sur Gynecol Obstet 1923;37:635-47.
10. Dhammi IK, Singh S, Jain AK, Kumar S. Isolated tuberculous tenosynovitis of the flexor carpi ulnaris: A case report and review of literature. Acta Orthop Belg 2006;72:779-82.
11. Le Meur A, Arvieux C, Cormier M. Tenosynovitis of the wrist due to resistant mycobacterium tuberculosis in a heart transplant patient. J Clin Microbiol 2005;43:988-90.
12. Miquel A, Frouge C, Adrien C, Hibou I, Bittoun J, Bisson M, et al. Tuberculous tenosynovitis of the wrist: Ultrasonographic diagnosis and contribution of MRI. J Radiol 1995;76:285-8.
13. Sy MH, Diouf S, Dansokho AV, Ndiaye A, Ndiaye PD, Seye SIL. Tuberculous tenosynovitis of the wrist: about 2 cases. Main 1998;3:69-76.
14. Regnard PJ, Barry P, Isselin J. Mycobacterial tenosynovitis of the flexor tendons of the hand. A report of five cases. J Hand Surg Br 1996;21:351-4.
 |
 |
 |
 |
| Dr. Coulibaly Ndeye Fatou | Dr. BA Amadou | Dr. Dembele Badara | Dr. Gueye Alioune Badara |
| How to Cite This Article: Coulibaly Nf, BA A, Gueye AB , Dembele B, Daffe M, Dieme CB. Tuberculous Tenosynovitis of the Wrist and the Hand: The 3 Anatomo-Clinical Forms Described by Kanavel (About 4 Cases). Journal of Orthopaedic Case Reports 2017 Nov-Dec; 7(6): 68-72. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com




