[box type=”bio”] Learning Point for this Article: [/box]
Acute re-implantation of bone is a new frontier in the treatment of bone loss. However, to make it safe, it needs further investigations.
Case Report | Volume 8 | Issue 1 | JOCR Jan – Feb 2018 | Page 3-7| Serafino Carta, Alberto Riva, Mattia Fortina, Giovanni Battista Colasanti, Luigi Meccariello. DOI: 10.13107/jocr.2250-0685.972
Authors: Serafino Carta[1], Alberto Riva[2], Mattia Fortina[1], Giovanni Battista Colasanti[1], Luigi Meccariello[3]
[1]Department of Orthopedics and Traumatology, University of Siena, University Hospital “Santa Maria Alle Scotte,” Siena, Italy.
[2]Department of Orthopaedics and Traumatology, Ente Ospedaliero Ospedali Galliera, Genova, Italy.
[3]Department of Orthopedics and Traumatology, Vito Fazzi Hospital, Lecce, Italy.
Address of Correspondence:
Dr. Luigi Meccariello,
Department of orthopedics and Traumatology, Vito Fazzi Hospital, Via Ada Cudazzo, Block: A-Floor: V, Lecce, Italy.
E-mail: drlordmec@gmail.com
Abstract
Introduction: This case report describes the management and the possible therapeutic solutions for the treatment of femoral bone loss associated with an open fracture IIIB Gustilo Andersonin a polytrauma that includes floating knee (GF) Fraser IIB from damage control orthopedics to final treatment.
Case Report: The patient was treated with an external fixator femorotibial bridge after extensive cleaning and debridement of open fractures. After 17-day post-trauma, we substitute the fixator with a less invasive stabilization system plate and screws with contralateral allograft bone strut.3months after the first surgery, the patient underwent surgery for the intramedullary nailing of the tibia. The follow-up was clinical using the knee injury and osteoarthritis outcome score (KOOS), short form 12 health survey (SF-12) for the quality of life, and radiological at 1–3–6–12–18–24–36 months. The patient walked with partial load up until the 6months after injury and then began a progression to a total load. At 24-months post surgery, the patient had both the KOOS and SF-12 at 100 points.
Conclusion: Not all Fraser IIB are equal, the timing of treatment should be discussed case by case. The surgical sequence should be respected: First, the fixation of the femur, and then, the stabilization of the tibia, taking into account the condition of the skin, eventual exposure or the eventual level of sub-amputation of the limb. The clinical and radiographic results show how efficient damage can lay the foundations for an excellent definitive treatment.
Keywords: Bone loss, floating knee, bone reimplant, external fixation, bone allograft strut, outcomes.
Introduction
With modernization and advances in motorized technology, the pattern and problems associated with trauma are also changing [1]. Road traffic accident accounts for majority of the cases and this was followed by fall from height. The word floating knee was introduced for the first time by McBryde in 1965 as reported by Nouraei et al.[1]. This injury is defined as a flail knee joint resulting from fractures of the shafts or adjacent metaphyses of the femur and ipsilateral tibia (see image below). Floating knee injuries may include a combination of diaphyseal shaft, metaphyseal, and intra-articular fractures [2].Besides, being caused by high-energy trauma with extensive skeletal and soft tissue damage, they are also associated with potentially life-threatening injuries of the head, chest, and abdomen [3]. The floating knee is a complex injury with more than just ipsilateral fractures of the femur and tibia. The prognostic indicators of the initial and final outcome in patients include injuries and the type of fracture (open, intra-articular, and comminution)[4]. Some other complications attributable to floating knee injuries include infection, excessive blood loss, fat embolism, malunion, delayed or nonunion, knee stiffness, prolonged hospitalization, and inability to bear weight[3]. Fractures of the distal part of the femur account for 7% of all femoral fractures [5]. Supracondylar fractures of the femur with bone defect/loss are a challenge for orthopedic surgeons to treat. Bone loss and open fracture are complex injuries that are difficult to manage; despite advances in technique and improved implants, treatment remains a challenge in many situations [5]. The autologous bone reimplant properly treated and the use of bone sticks, derivation of stem cells from the bone marrow and platelet-rich plasma (PRP) is a practice in traumatology used for some years opposed to the metal for the synthesis treats serious bone loss. The purpose of this case report is to report on the proper damage control definitive treatment of bone loss in the treatment of femoral bone loss of a polytrauma affection even knee floating Fraser IIB with double exposure Grade III B of the femoral and tibial shaft.
Case report
At 4:30 am, a 23-year-old patient arrived at our drug enforcement administration, after a high kinetic energy car accident (car against the wall) in orotracheal intubation with a Glasgow coma scale (GCS) of 11/15, mangled extremity severity score 4 points for the femur, and 3 points for the leg, and an injury severity score of 24 points:oderate concussion, moderate splenic ulcerations, supra-intercondylar fracture of the femur (3.3-C1 according to AO) left exposed Gustilo Anderson (GA) IIIB and bone loss of the metaphyseal area >50% and shaft fracture(Fig.1 and 2) with a third fragment (4.2-B2 according to AO) exposed GA 3B(Fig.1).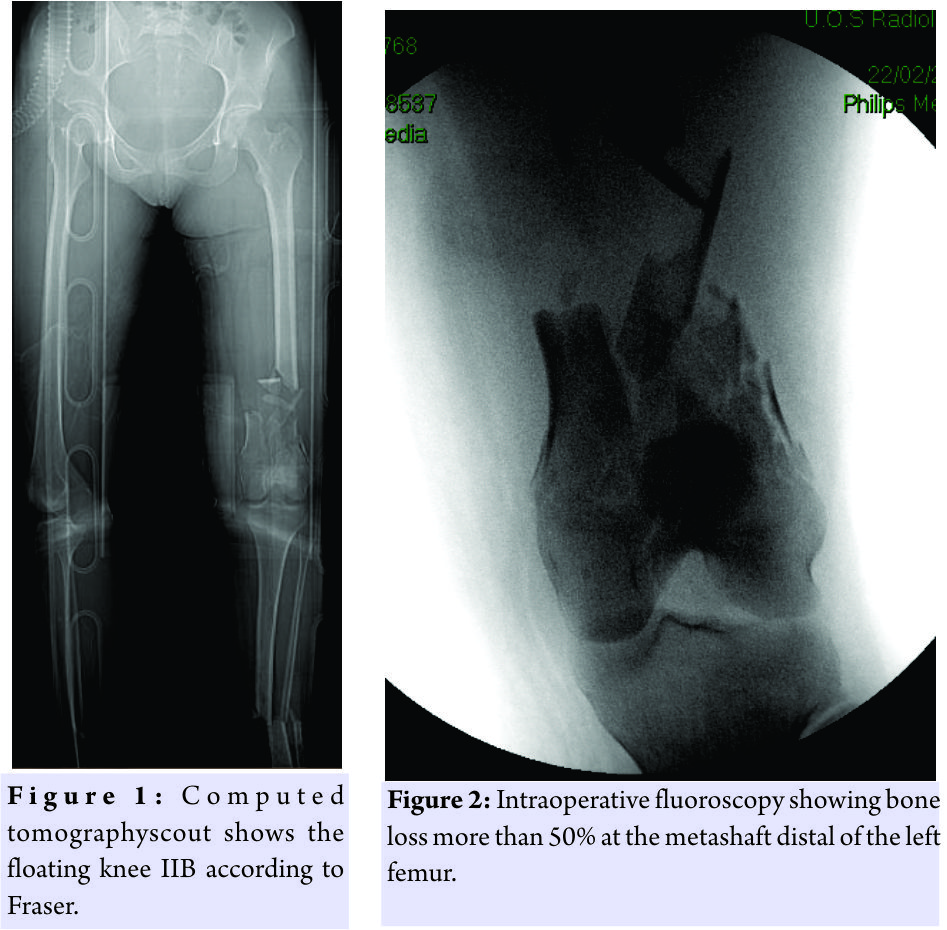 The patient was treated in emergency with a bridge femorotibial external fixator after extensive cleaning and debridement of open fractures(Fig.3a and b). After stabilization, the wounds were covered with iodine-impregnated incision drape (Ioban). During the damage control’s operations, a fragment of 8 cm × 3 cm × 4cm of bone substance corticospongiosa was found in the left sock. The fragment was immersed in a solution of cefuroxime, gentamicin, and metronidazole and maintained at a temperature of −3°C until 2h before the intervention because it was irradiated with a dose of 25kGy. The 4days, we removed the antibiotated chains and the Ioban cover which were replaced with vacuum therapy. The patient never had fever over 38°Cduring his 10 days in intensive care and in the ward. The delayed risk of tibial consolidation was equal to 8 of 10 according to A.R.R.C.O. As regards the femur, the risk of non-union of the fracture of the femur of 51 points according to the non-union scoring system(N.U.S.S).
The patient was treated in emergency with a bridge femorotibial external fixator after extensive cleaning and debridement of open fractures(Fig.3a and b). After stabilization, the wounds were covered with iodine-impregnated incision drape (Ioban). During the damage control’s operations, a fragment of 8 cm × 3 cm × 4cm of bone substance corticospongiosa was found in the left sock. The fragment was immersed in a solution of cefuroxime, gentamicin, and metronidazole and maintained at a temperature of −3°C until 2h before the intervention because it was irradiated with a dose of 25kGy. The 4days, we removed the antibiotated chains and the Ioban cover which were replaced with vacuum therapy. The patient never had fever over 38°Cduring his 10 days in intensive care and in the ward. The delayed risk of tibial consolidation was equal to 8 of 10 according to A.R.R.C.O. As regards the femur, the risk of non-union of the fracture of the femur of 51 points according to the non-union scoring system(N.U.S.S).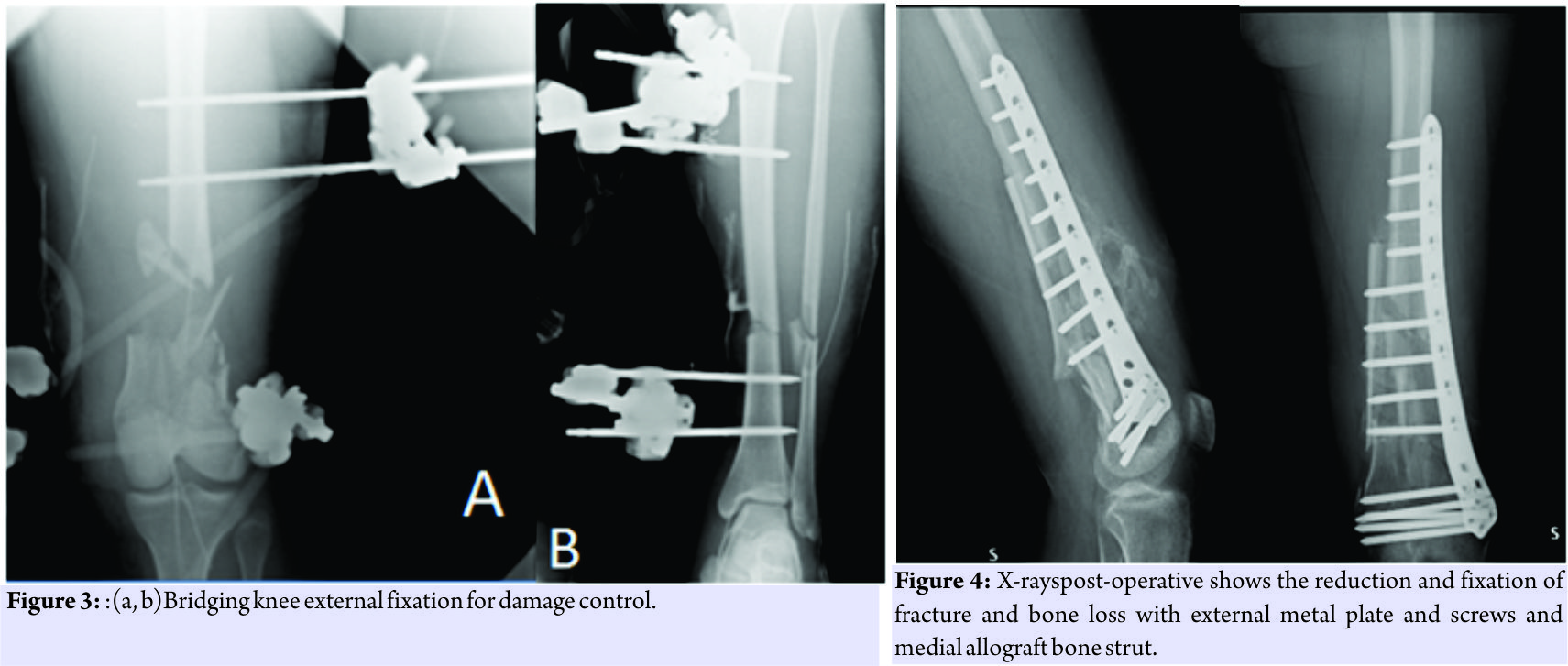 The patient was not treated surgically for the fissure of the spleen, and the resolution of the neurological picture took place after 6 days. The patient was submitted to a specific antibiotic therapy according to the protocol for the open fractures and was monitored with clinical and laboratory examinations. The 21stday post-trauma, without any clinical or laboratory signs, the patient was operated on with a less invasive stabilization system plate and screws, cortical and cancellous bone grafting allogeneic bank, and autologous stem cells taken from the iliac crest, PRP rich in leukocytes and replanting of native bone. The surgical access chosen was the lateral subvastus to preserve the perforating arteries(Fig.4). The patient was monitored with 15 days clinical follow-up, laboratory, and radiological at 1 month, 2 months, 3 months, 6 months, 12 months, 18 months, 24 months, 36 months, and 48 months. The indices used to evaluate the outcomes of this intervention were the knee injury and osteoarthritis outcome score (KOOS), the related union scorefemur (R.U.S.F.) for the femoral bone healing, and the score radiographic union score for tibial fractures (R.U.S.T.). For bone consolidation of shank, the short form 12 health survey (SF-12) for the quality of life, and the number of complications and re-operations. The patient in the immediate post-operative made active and passive mobilization of the knee until the 3rdmonth, reaching a flexion of 90°. The patient was subjected to the intervention of removal of the external fixator and intramedullary nailing of the tibia 3 months after the first surgery(Fig. 5).
The patient was not treated surgically for the fissure of the spleen, and the resolution of the neurological picture took place after 6 days. The patient was submitted to a specific antibiotic therapy according to the protocol for the open fractures and was monitored with clinical and laboratory examinations. The 21stday post-trauma, without any clinical or laboratory signs, the patient was operated on with a less invasive stabilization system plate and screws, cortical and cancellous bone grafting allogeneic bank, and autologous stem cells taken from the iliac crest, PRP rich in leukocytes and replanting of native bone. The surgical access chosen was the lateral subvastus to preserve the perforating arteries(Fig.4). The patient was monitored with 15 days clinical follow-up, laboratory, and radiological at 1 month, 2 months, 3 months, 6 months, 12 months, 18 months, 24 months, 36 months, and 48 months. The indices used to evaluate the outcomes of this intervention were the knee injury and osteoarthritis outcome score (KOOS), the related union scorefemur (R.U.S.F.) for the femoral bone healing, and the score radiographic union score for tibial fractures (R.U.S.T.). For bone consolidation of shank, the short form 12 health survey (SF-12) for the quality of life, and the number of complications and re-operations. The patient in the immediate post-operative made active and passive mobilization of the knee until the 3rdmonth, reaching a flexion of 90°. The patient was subjected to the intervention of removal of the external fixator and intramedullary nailing of the tibia 3 months after the first surgery(Fig. 5).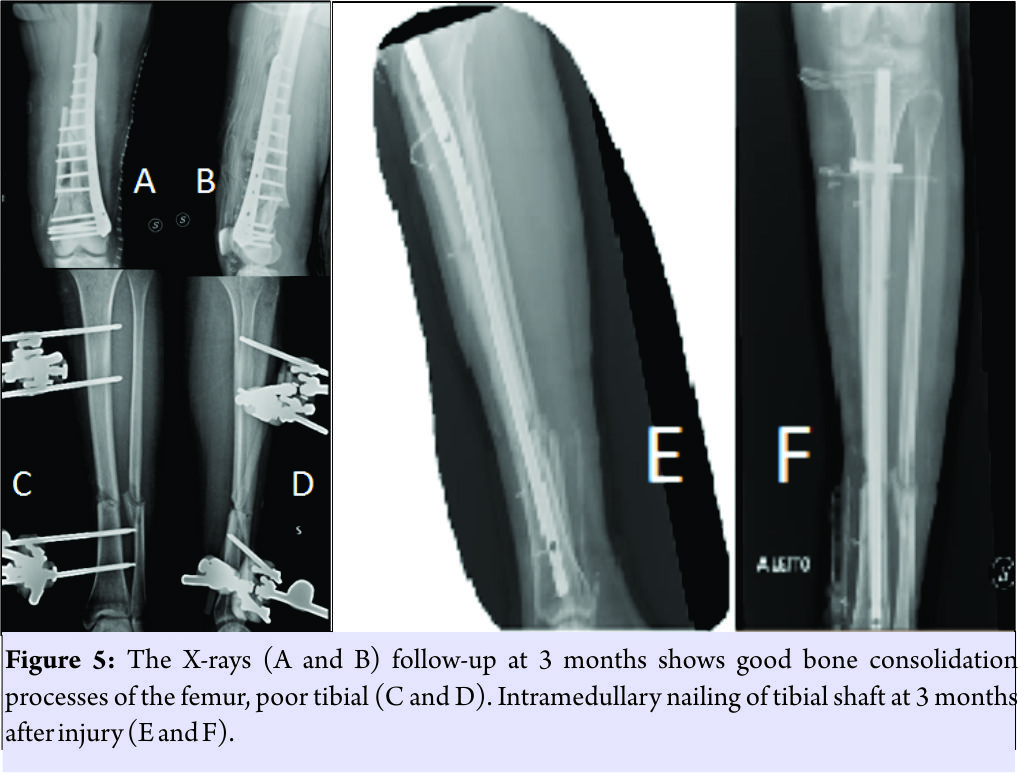 The patient has walked with a partial load up to 6 months after the injury and then began to progress to a total load. At 12 months, the patient had a KOOS of 89.3 points, a SF-36 of 89.3 points, the R.U.S.T. 3 out of 3 points, and R.U.S.F. 3 out of 4 points. At 24months, the patient had an intramedullary nail removal of 100 points KOOS, 100 points SF-36, the R.U.S.T. 3 out of 4 points, and R.U.S.F. 4 out of 4 points. At follow-up at the past 36 months, a year after the removal of plaque and nail, the patient showed KOOS 100 points, a SF-36 out of 100 points(Fig. 6), and R.U.S.T and R.U.S.T 4 out of 4 points(Fig. 7). After 2 years, the patient had the tibia nail removed. The patient did not present any complications throughout the post-operative and follow-up.
The patient has walked with a partial load up to 6 months after the injury and then began to progress to a total load. At 12 months, the patient had a KOOS of 89.3 points, a SF-36 of 89.3 points, the R.U.S.T. 3 out of 3 points, and R.U.S.F. 3 out of 4 points. At 24months, the patient had an intramedullary nail removal of 100 points KOOS, 100 points SF-36, the R.U.S.T. 3 out of 4 points, and R.U.S.F. 4 out of 4 points. At follow-up at the past 36 months, a year after the removal of plaque and nail, the patient showed KOOS 100 points, a SF-36 out of 100 points(Fig. 6), and R.U.S.T and R.U.S.T 4 out of 4 points(Fig. 7). After 2 years, the patient had the tibia nail removed. The patient did not present any complications throughout the post-operative and follow-up.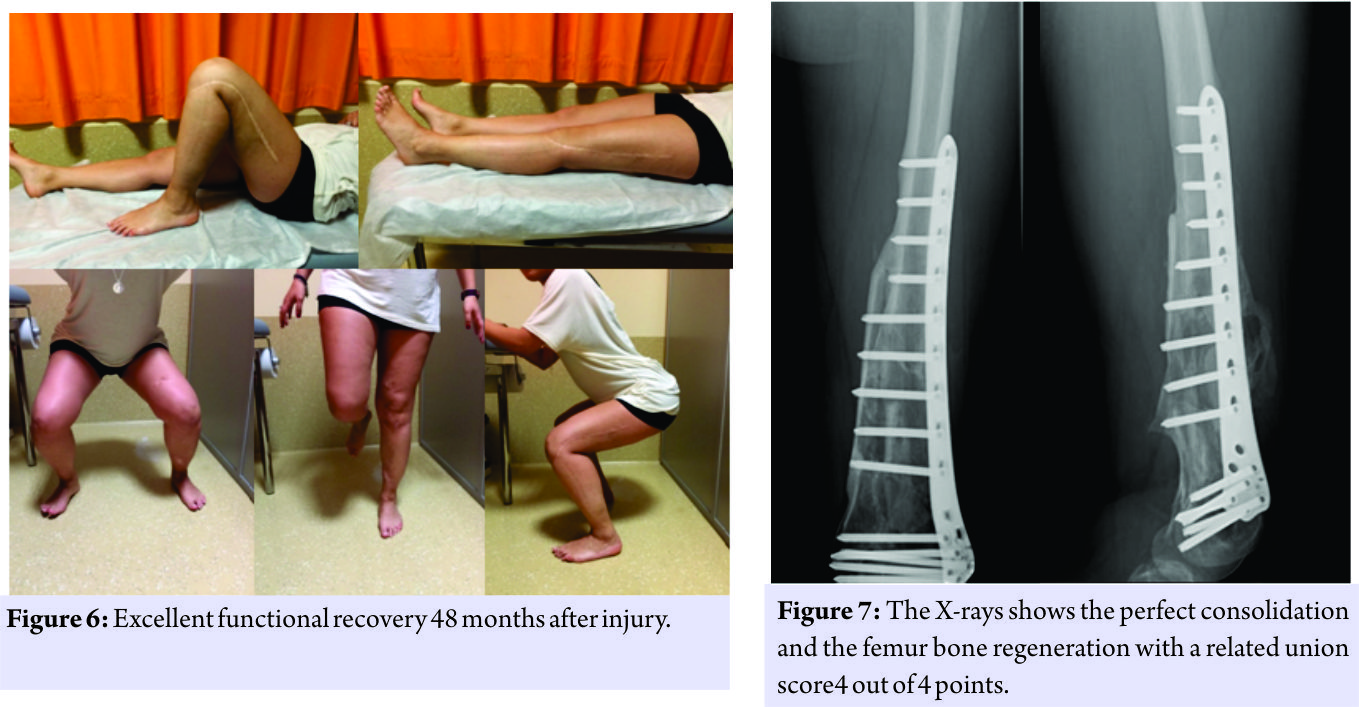
Discussion
The floating knee is unfortunately always associated with more internal injuries that make it difficult to provide a total care early on [6]. Furthermore, in our case, we had a double IIIB exposure which is very rare in floating knee IIB according to Fraser. Looking at the ISS score and the GCS, we must put a damage control in place [7], before the stabilization of both bone fragments, it is essential to carry out a careful debridement and thorough washing with a physical examination of the exposition. As reported by Veith, to have a chance of a good outcome, and also to save the patient’s life and reduce perioperative complications, it is necessary to optimally stabilize both segments. In fact, our choice fell on the external fixation, putting the knee bridge in bending at 20°. To maintain the highest possible sterility and preserve the sites of exposure by superinfection of resistant super bacteria residing in TI, we have isolated the bone exposure with a steri-strip with betadine [8] waiting to activate the vacuum-assisted closure (VAC) therapy at the moment not yet available at our structure. As shown by Grubor et al. [9], the use of VAC therapy in open fracture IIIB Cierny and Mader IIIB osteomyelitis drastically reduces the risk of septic shock and limb amputation. In the literature, there are not many studies, but a few case reports show the opportunity to replant large fragments of bone devascularized, however, to make this replanting on final osteosynthesis you need to make careful cleaning and debridement. The bone fragment was sent to the bone bank for a proper preservation and thawed 2 days before, to be subjected to a treatment for decantation in antibiotics and irradiation with ionizing rays to avoid the formation of bacterial biofilms on the surface of the implant. The treatment by decantation in the three antibiotics was fundamental: Gentamicin for the broad spectrum against g + and g − bacteria, in particular against Escherichiacoli, coliforms, Pseudomonas aeruginosa, and Proteus [10] and for the ability to perform a surfactant function that covers the bone surface and prevents the adhesion of bacterial colonies [11]; cefuroxime, also for the broad spectrum of action and in particular the activities toward all Staphylococci and Streptococci and metronidazole for the activity to all anaerobes as Freeman et al. [12].In the literature, there is no consensus on how to permanently sterilize bone segment to replant, however, Singh et al. [13] showed the high rate of sterilization of tumor cells from soft tissue using the autoclave. However, the use of the autoclave to the high temperatures destroys the osteoinductive capacity and mechanical bone to replant [13]. According to ISO 11137, 2002 to sterilize the bone serve a 25 kGy of ionizing rays, in fact, Aizah et al. [14] showed a success in the replanting of a distal femoral metaphysis (open fracture IIIA GA) in a young man of 14 years after sterilization by gamma irradiation of the entire fragment. Finding ourselves in front of a massive bone loss >50% of the distal metaphysis of the femur and a N.U.S.S score of 51, we had to resort to diamond concept, being comparable to a Grade 3 N.U.S.S, or rather compromission of both biological and mechanical segments. We decided, even in the absence of inflammatory or septic manifestations, to wait 21 days for the final intervention, as a soft callus was formed which is comparable to a primordial biological room. At the same time, the necessary time for the formation of our biological room with respect to the distal femur had relapsed; we had to choose among three possible treatments: The method of pseudomembrane of massequet, the double opposed plate of metal according Ruedi, and the organic metal solution according to the Bologna’s school. The choice of the method was carried out in the surgery room, after the subvastus lateral access for the preservation of the perforating [15], and therefore, the respect of the biology of the lateral compartment. It was decided to opt for the organic metal solution, as from the experience of periprosthetic femoral fractures, the contrast between a splint bone and a metal plate increases the mechanical strength of the femur 2250 N and is the best biological solution, considering that the splint has a mechanical filler as well as a stimulus for the bone’s growing [16]. Our technique has been put in place respecting the algorithm devised by Calori et al. [17], with the only change the PRP and mesenchymal cells instead of Bone morphogenetic protein-7, for exploiting the totipotent capacity of leukocytes to turn into osteoblasts [17]. Having a ligament stability from both the collaterals and cruciates, and because we did not have a fibrous retraction, nor a knee pseudoankylosis since the early moments of the intervention, we made a cautious passive knee kinesis with a progressive increase of joint range of motion during the post-operative days. The external fixator leg during surgery had been overhauled by placing compression fragments to heal the fracture of tibia with that kind of synthesis. We scored ARCO and could see both direct and indirect radiological signs of modest bone callus, 3 months after, the tibia had been repaired with plate and screws, to increase the partial load bearing ability, the patient had been able to progress to total load bearing; there were also direct and indirect bone regeneration and strengthening of the femur that allowed the patient to walk with aids. Although trivial, we were able to ascertain that the mood of the patient was directly related to the ability to walk that was gradually acquired [18]. The clinical and radiographic results in the case reported are certainly encouraging, demonstrating that at least part of the “biological push” provided by the use of stem cells is capable of increasing the potential of synthesis techniques, however, we should not underestimate the opportunity to attack the biological chamber through the soft tissue and the possible role of the post head trauma somatostatin secretion that may assist the regenerative potential of stem cells. Furthermore, the placement of a splint to the medial cortical bone level opposite to the plaque leads to an increase of the resistance of the femoral medial wall to almost 2250 Newton giving the femoral shaft undisputed biomechanical advantages. These results encourage a continuation of the experience and a comparison with the literature for results that are uniform for each one.
Conclusion
Clinical and radiographic results in the case are certainly encouraging, demonstrating at least in part that the “biological thrust” provided by the use of stem cells is capable of increasing the potential of synthesis techniques, but should not be underestimated, the opportunity not to attack the biological chamber by observing the soft tissue and the possible role of the secretion of somatostatin post-traumatic trauma that can support the regenerative potential of stem cells. In addition, the placement of a medial cortical bone cage opposite to the plaque leads to an increase in the femoral medial wall resistance to nearly 2250 Newton giving the biomechanical advantages of undifferentiated femoral shaft[16]. Such results stimulate a continuation of experience and a comparison with literature to achieve results that are homogeneous for each segment.
Clinical Message
Traumatic extrusion of bone is a rare complication of high-energy open fractures, and there are only few studies published in literature on reimplantation of the extruded bone segment. Studies with clear guidelines regarding timing of reimplantation, stabilization of extruded bone segments, and bone disinfection, and disinfection techniques are very few. Reimplantation of extruded bone is a risky procedure due to high chances of infection which determines the final outcome and can result in secondary amputations. Our technique described may be one of the possible alternatives for bone reimplantation and regeneration of bone defects in long bones.
References
1. Nouraei MH, Hosseini A, Zarezadeh A, Zahiri M. Floating knee injuries: Results of treatment and outcomes. J Res Med Sci 2013;18:1087-91.
2. Rethnam U, Yesupalan RS, Nair R. Impact of associated injuries in the floating knee: A retrospective study. BMC Musculoskelet Disord 2009;10:7.
3. Elmrini A, Elibrahimi A, Agoumi O, Boutayeb F, Mahfoud M, Elbardouni A. Ipsilateral fractures of tibia and femur or floating knee. Int Orthop 2006;30:325-8.
4. Hegazy AM. Surgical management of ipsilateral fracture of the femur and tibia in adults (the floating knee): Postoperative clinical, radiological, and functional outcomes. Clin Orthop Surg 2011;3:133-9.
5. Gawri V, Garg Y, Singh D, Garg RS, Choudhary N. Complex open distal femur fracture managed by primary autogenous fibular graft in conjunction with DFLP- A case report. J Clin Diagn Res 2015;9:RD01-3.
6. Pfeifer R, Pape HC. Diagnostics and treatment strategies for multiple trauma patients. Chirurg 2016;87:165-73.
7. Easton R, Balogh ZJ. Peri-operative changes in serum immune markers after trauma: A systematic review. Injury 2014;45:934-41.
8. Cross WW 3rd, Swiontkowski MF. Treatment principles in the management of open fractures. Indian J Orthop 2008;42:377-86.
9. Grubor P, Falzarano G, Grubor M, Piscopo A, Franzese R, Meccariello L. Treatment of the chronic war tibial osteomyelitis, Gustilo Type IIIB and Cierny-Mader IIIB, using various methods. A Retrospective study. Euromediterranean Biomed J 2014;9:7-18.
10. El Zowalatyl ME, Gyetvaii B. Effectiveness of antipseudomonal antibiotics and mechanisms of multidrug resistance in Pseudomonas aeruginosa. Pol J Microbiol 2016;65:23-32.
11. Lucke M, Schmidmaier G, Sadoni S, Wildemann B, Schiller R, Haas NP, et al. Gentamicin coating of metallic implants reduces implant-related osteomyelitis in rats. Bone 2003;32:521-31.
12. Freeman CD, Klutman NE, Lamp KC. Metronidazole. A therapeutic review and update. Drugs 1997;54:679-708.
13. Singh VA, Nagalingam J, Saad M, Pailoor J. Which is the best method of sterilization of tumour bone for reimplantation? A biomechanical and histopathological study. Biomed Eng Online 2010;9:48.
14. Aizah N, Su Y, Shaifulnizam C, MRos M. Reimplantation of an extruded femoral segment after gamma sterilization in A Type IIIA supracondylar femur fracture: A Case report. Malays Orthop J 2014;8:66-8.
15. Bertrand ML, Andrés-Cano P, Pascual-López FJ. Periarticular fractures of the knee in polytrauma patients. Open Orthop J 2015;9:332-46.
16. Peters CL, Bachus KN, Davitt JS. Fixation of periprosthetic femur fractures: A biomechanical analysis comparing cortical strut allograft plates and conventional metal plates. Orthopedics 2003;26:695-9.
17. Calori GM, Giannoudis PV. Enhancement of fracture healing with the diamond concept: the role of the biological chamber. Injury. 2011;42(11):1191-3. doi: 10.1016/j.injury.2011.04.016.
18. Collins NJ, Prinsen CA, Christensen R, Bartels EM, Terwee CB, Roos EM, et al. Knee injury and osteoarthritis outcome score (KOOS): Systematic review and meta-analysis of measurement properties. Osteoarthritis Cartilage 2016;24:1317-29.
 |
 |
 |
 |
 |
| Dr. Serafino Carta | Dr. Alberto Riva | Dr. Mattia Fortina | Dr. Giovanni Battista Colasanti | Dr. Luigi Meccariello |
| How to Cite This Article: Carta S, Riva A, Fortina M, Colasanti G. B, Meccariello L. The Challenges of the Femoral Bone Loss in the Management of the Floating Knee IIB According Fraser: A Case Report. Journal of Orthopaedic Case Reports 2018 Jan-Feb; 8(1): 3-7. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com




