[box type=”bio”] Learning Point for this Article: [/box]
The use of surgical navigation during revision THA can improve the accuracy with which components are placed and has the potential to limit both surgical costs and patient morbidity.
Case Report | Volume 8 | Issue 1 | JOCR Jan – Feb 2018 | Page 53-56 | John Vincent, Ibrahim Alshaygy, Jeffrey M Muir, Paul Kuzyk. DOI: 10.13107/jocr.2250-0685.996
Authors: John Vincent[1], Ibrahim Alshaygy[2], Jeffrey M Muir[3], Paul Kuzyk[2]
[1]Faculty of Applied Health Sciences, School of Public Health and Health Systems, University of Waterloo, Waterloo, Ontario, Canada,
[2]Department of Orthopaedic, Mount Sinai Hospital, Division of Orthopaedic Surgery, Toronto, Ontario, Canada,
[3]Department of Clinical Research, Intellijoint Surgical, Inc., Waterloo, Ontario, Canada.
Address of Correspondence:
Dr. Paul Kuzyk,
Mount Sinai Hospital, 600 University Ave., Room 476A, Toronto, Ontario, Canada.
E-mail: pkuzyk@mtsinai.on.ca
Abstract
Introduction: While intraoperative navigation systems have been shown to improve outcomes in primary total hip arthroplasty (THA), their use in the context of revision has been largely overlooked. This case report presents the first documented use of an imageless navigation tool in the context of revision THA, and an unexpected benefit to the surgical procedure as a result.
Case Report: An 84-year-old female patient presented following five episodes of dislocation of the left hip and with pain in the left buttock, groin, and posterior aspect of her hip. Relevant surgical history included primary hip arthroplasty in 1999 and the first revision in 2014. Pre-operative analysis revealed a constrained liner that had become disengaged and migrated inferiorly, lodging at the distal aspect of the femoral neck. Acetabular protrusion was also noted. The pre-operative plan included the replacement of the fragmented liner and likely of the acetabular cup due to hardware failure. Intraoperative assessment, however, revealed that the cup was in good condition and would be difficult to remove due to substantial bony ingrowth. With the assistance of imageless navigation, the orientation of the acetabular cup was determined and a new constrained liner was cemented into the preexisting acetabular component at an altered orientation, correcting anteversion by 7°.
Conclusions: In revision hip arthroplasty cases, image-based navigation is limited by the presence of existing implants and corresponding metal artefact. This case demonstrates the successful use of an imageless navigation tool for revision surgery. Use of navigation led to the unexpected intraoperative discovery that the acetabular cup was in an acceptable state, and allowed the surgical team to correct the position of the cup using a constrained liner, thus preserving the cup. This significantly benefitted patient outcome, due to the risks associated with the removal of a firmly fixated acetabular cup. While more extensive research is required, this case demonstrates that imageless navigation may be an indispensable tool for revision surgery.
Keywords: Imageless navigation, revision, total hip arthroplasty, elderly, intraoperative navigation.
Introduction
Total hip arthroplasty (THA) is a common surgery for the treatment of end-stage osteoarthritis and other degenerative hip diseases and has been shown to greatly improve patient quality of life [1]. Relative to primary THA, revision cases present greater difficulty and higher associated costs [2]. Removal of existing hip implants introduces substantial risk of both medical and surgical complications, leading to higher in-hospital mortality rates and greater length of stay relative to primary surgeries [1]. These complications contribute to elevated costs of revision arthroplasty. In Canada, while the cost of a primary THA procedure averages $8656, revision THA costs average $12,949, an increase of 50% [3]. Subsequent complications such as infection can raise costs to over $20,000 per case, substantially impacting an already overburdened healthcare system [3]. To reduce the costs associated with revision, as well as the risk of re-revision, optimal positioning of the new implant components is a necessity. Computer-assisted navigation systems have been developed to intraoperatively assist component placement, sizing, and orientation [4]. Unfortunately, their use in revision surgery has been largely overlooked in the literature [5, 6]. The presence of the existing implant components and added surgical steps may alter how navigation can be used, suggesting that a versatile navigation device is needed to accommodate the wide array of scenarios encountered in revision THA. Overall, more information on the use of navigation in revision THA is needed. Here, we report the results of a revision THA procedure performed with the assistance of a new mini-navigation device. The device provides the surgeon with real-time information on cup position and leg length changes and influenced intraoperative decision-making, in this case, allowing for retention of the existing acetabular cup and resulting in reduced procedural costs, blood loss, and potential for iatrogenic injury.
Case report
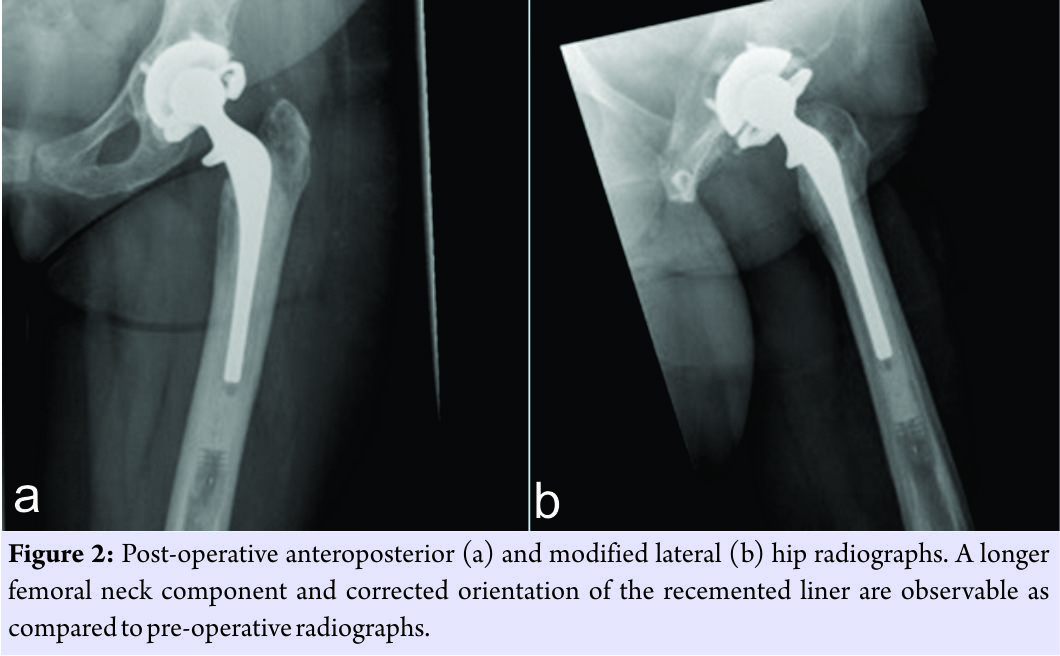
An 84-year-old female patient was seen in the emergency department following a revision total hip dislocation. She had undergone a primary THA in 1999 for avascular necrosis of the femoral head. The primary procedure utilized a hybrid prosthesis, with a cemented femoral stem and uncemented acetabular cup. Her THA functioned well for approximately 15 years until a first revision was required in 2014 for polyethylene wear resulting in hip dislocation. Both stem and cup were left intact during the first revision, with a constrained liner and new femoral head inserted to prevent further dislocation. However, recurrent dislocations were experienced shortly after the first revision surgery. Despite management through closed reduction, pain medication and rehabilitation, the patient was seen in the ED following her fifth dislocation in late 2016. The patient presented with a complex medical history, including sickle cell disease, hypothyroidism, and gastroesophageal reflux disease. Before ED admittance, the patient was mobile with the use of a Rollator walker but experienced an antalgic gait and increased walking difficulties. Despite regular Percocet use to control sickle cell crisis symptoms, the patient presented with pain in the left buttock, groin, and posterior aspect of her hip. Following examination in the ED, a second revision surgery was deemed necessary. Here, we report the findings of this second revision procedure. Pre-operative radiographic analysis revealed disengagement and inferior migration of the constrained liner, with suspicion of a fragmented polyethylene liner superolaterally (Fig. 1).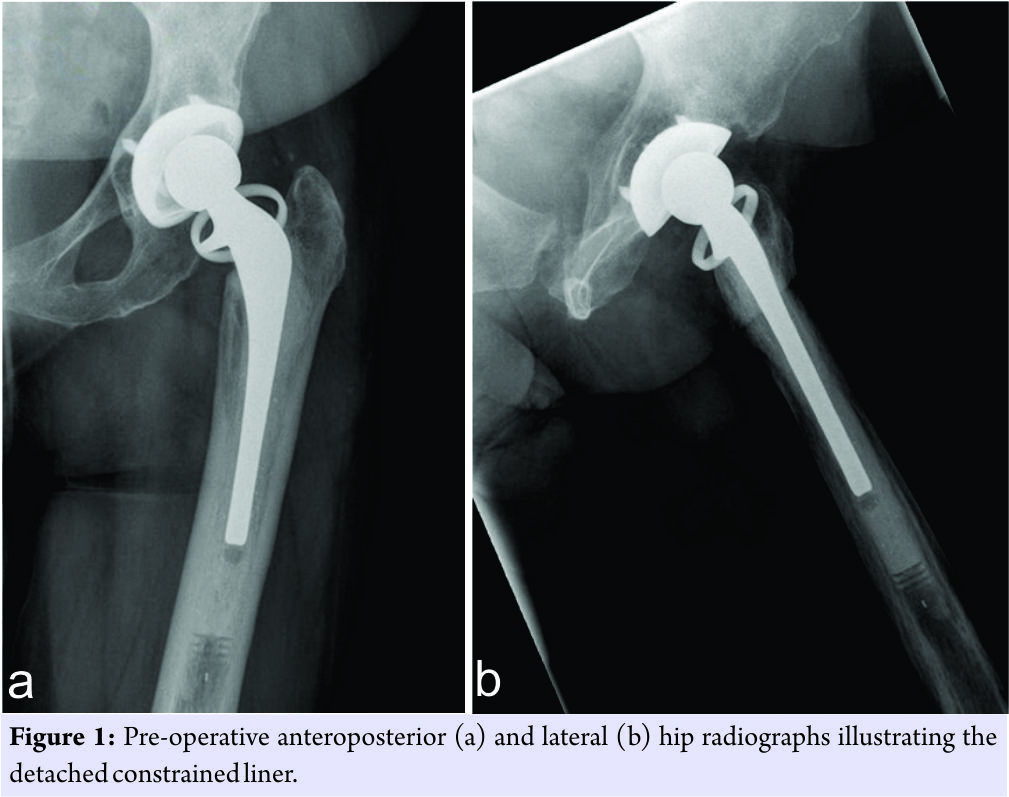 The acetabular cup was noted to be quite vertical but with no evidence of periprosthetic fracture. It was expected that complete removal and replacement of the acetabular cup component would be required, and a surgical plan for the cup revision was prepared. Revision THA was performed through the posterior approach, with the assistance of the Intellijoint HIP® mini-navigation tool (Intellijoint Surgical Inc., Waterloo, ON). The use of the mini-navigation system has been described elsewhere [7]. In brief, the system utilizes a camera, which sits atop a pelvic platform fixed to the ipsilateral iliac crest through two surgical screws. The camera captures the position and movement of a tracker that can be magnetically attached to a small platform fixed to the greater trochanter or to surgical tools (e.g., impactor and surgical probe). The camera relays data regarding the position and movement of the tracker to a workstation, located outside of the surgical field but within view of the surgeon. Installation of the navigation system was completed before dislocation and used to determine the initial leg length and offset. On initial surgical examination, damage to the posterior aspect of the liner due to impingement was noted and substantial bony ingrowth around the acetabular cup component had occurred. After posterior dislocation and removal of the polyethylene liner, the navigation probe and tracker were used to verify a cup position of 45° inclination and 27° anteversion. While more anteverted than desired, the cup was stable and in good condition. The decision was made to preserve the cup component and correct the excessive anteversion using a new cemented constrained liner. After thorough irrigation and roughening of the cup interior, the new liner was cemented in place with slight retroversion relative to the cup. The navigation tool was successfully used to guide liner placement, providing updated measurements on position until a final liner orientation of 45° inclination and 19° anteversion was achieved. The femoral stem was found to be stable, and a femoral head with a longer neck length (+7 mm) was inserted to reduce the chances of levering. No signs of impingement were noted, and navigation confirmed that leg length and offset remained stable. Navigation enabled modification of the initial surgical plan, resulting in successful preservation of the primary acetabular cup and stem (Fig. 2).
The acetabular cup was noted to be quite vertical but with no evidence of periprosthetic fracture. It was expected that complete removal and replacement of the acetabular cup component would be required, and a surgical plan for the cup revision was prepared. Revision THA was performed through the posterior approach, with the assistance of the Intellijoint HIP® mini-navigation tool (Intellijoint Surgical Inc., Waterloo, ON). The use of the mini-navigation system has been described elsewhere [7]. In brief, the system utilizes a camera, which sits atop a pelvic platform fixed to the ipsilateral iliac crest through two surgical screws. The camera captures the position and movement of a tracker that can be magnetically attached to a small platform fixed to the greater trochanter or to surgical tools (e.g., impactor and surgical probe). The camera relays data regarding the position and movement of the tracker to a workstation, located outside of the surgical field but within view of the surgeon. Installation of the navigation system was completed before dislocation and used to determine the initial leg length and offset. On initial surgical examination, damage to the posterior aspect of the liner due to impingement was noted and substantial bony ingrowth around the acetabular cup component had occurred. After posterior dislocation and removal of the polyethylene liner, the navigation probe and tracker were used to verify a cup position of 45° inclination and 27° anteversion. While more anteverted than desired, the cup was stable and in good condition. The decision was made to preserve the cup component and correct the excessive anteversion using a new cemented constrained liner. After thorough irrigation and roughening of the cup interior, the new liner was cemented in place with slight retroversion relative to the cup. The navigation tool was successfully used to guide liner placement, providing updated measurements on position until a final liner orientation of 45° inclination and 19° anteversion was achieved. The femoral stem was found to be stable, and a femoral head with a longer neck length (+7 mm) was inserted to reduce the chances of levering. No signs of impingement were noted, and navigation confirmed that leg length and offset remained stable. Navigation enabled modification of the initial surgical plan, resulting in successful preservation of the primary acetabular cup and stem (Fig. 2).
At 6-week follow-up, the patient was mobilizing with a cane, undergoing physical therapy, and progressing as planned.
Discussion
Cases of revision hip arthroplasty often present with high clinical complexity and associated risks due to the nature of the surgery and the patient cohort in which they are performed. In the presented case, the patient’s advanced age (84), medical comorbidities, and history of primary THA 18 years before the revision procedure were risk factors for potential complication. Based on pre-operative analysis, the surgical plan indicated complete removal and replacement of the acetabular cup. Intraoperatively, the cup was found to be in good condition but excessively anteverted. With the assistance of the surgical navigation tool, the existing cup was preserved and a new constrained liner was placed in the appropriate position. Liner anteversion was corrected by 7° achieving the goals of revision surgery without disruption of the acetabular cup. Preservation of the existing acetabular cup provided numerous clinical benefits in this case. For the presented patient, the acetabular component had been in situ for 18 years, providing ample time for the formation of bony in-growth and firm fixation of the cup within the pelvis. In such cases, removal of components can be extremely demanding and time-consuming, resulting in excessive blood loss and damage to the remaining host bone [8]. Poor bone quality and bone loss, as expected in an elderly female patient with sickle cell disease, can necessitate the use of bone grafts or specialized acetabular components to ensure stable fixation [9]. Bone disruption in revision THA is also a significant risk factor for heterotopic ossification, resulting in severe post-operative hip pain and reduced range of motion [10]. Finally, replacing the acetabular cup increases wound exposure, leading to greater risk of wound disruption, surgical site infection, and systemic sepsis [1, 8]. Thus, while removal of the acetabular cup is sometimes necessary, surgeons must weigh the risks and benefits to best suit the patient. In the presented case, removal of the cup was averted with the assistance of imageless navigation. Regarding the femoral components, in this case, the use of a longer neck reduced future risk of levering and helped establish an equalized leg length and slight increase to offset. Results were confirmed by the navigation device, an important consideration for challenging cases such as this due to the current lack of reliable methods for measuring changes in leg length and offset intraoperatively [11]. The economic implications of the presented case are noteworthy due to reductions in direct expense, re-revision risk, and surgical time. Preservation of the acetabular cup not only reduced the risk of associated complications and for costly surgical techniques, such as bone grafting, but also removed the direct expense of a new acetabular component. With THA implant accounting for up to 50% of overall surgical costs, the potential cost savings are significant [12]. Furthermore, navigation use has been shown to reduce the risk of re-revision compared to unnavigated cases, thus liberating more resources for primary surgeries and reducing the overall case burden [13]. Finally, preservation of the acetabular cup reduced the length of surgery. Reductions in surgical time minimize procedural costs, as operating room time is valued at the equivalent of $30–108 Canadian dollar per minute [14]. Reduced surgical times also enhance efficiency, an important consideration since efficiency permits higher treatment volumes, and thus reduced waiting periods for patients. While Canada’s current benchmark for acceptable wait times in THA is 6 months (182 days), one in five patients do not receive treatment within this time frame [15]. Roughly 10% of Canadian patients wait more than 1 year for THA surgery, a concerning statistic considering the functional decline and pain that patient may experience during this time [15]. In primary cases, intraoperative navigation has been shown to improve outcomes following THA [4]. However, considerations unique to revision surgery may change or limit how existing navigation systems can be used, and studies investigating this topic are rare [5, 6]. Image-based navigation systems, such as computed tomography (CT) or fluoroscopy, have been shown to improve revision outcomes, but exhibit reduced accuracy due to image distortion from metal artefact introduced by the implants [5, 6]. In addition, image-based navigation systems are limited by concerns regarding radiation exposure, additions to surgical time, and high capital costs that reduce accessibility [5]. Imageless navigation presents a promising alternative, as it shown similar accuracy to CT-navigation in primary THA, and may be viable in revision THA since it does not rely on radiation [5]. Conversely, imageless systems that require fixation around the acetabulum or femoral head may not be viable in revision cases where native bone is limited [6].
Conclusion
In the presented case study, an imageless mini-navigation system was successfully implemented without obstructing the surgical workflow, demonstrating its potential role in this context. Further research is required to verify the findings of this case study and to determine which navigation systems are best suited to revision THA given the surgical variance from case to case.
Clinical Message
Preservation or removal of existing hardware in revision THA can significantly impact surgical costs, time and the potential for iatrogenic injury. The use of computer navigation in such cases can assist with intraoperative decision-making leading to improved patient outcomes.
References
1. Schwartz BE, Piponov HI, Helder CW, Mayers WF, Gonzalez MH. Revision total hip arthroplasty in the United States: National trends and in-hospital outcomes. Int Orthop 2016;40:1793-802.
2. Nichols CI, Vose JG. Clinical outcomes and costs within 90 days of primary or revision total joint arthroplasty. J Arthroplasty 2016;31:1400-6, e3.
3. CIHI. Patient Cost Estimator: Canadian Instituties of Health Information; 2017. Available from: https://www.cihi.ca/en/spending-and-health-workforce/spending/patient-cost-estimator. [Last cited on 2017 Mar 03].
4. Xu K, Li YM, Zhang HF, Wang CG, Xu YQ, Li ZJ, et al. Computer navigation in total hip arthroplasty: A meta-analysis of randomized controlled trials. Int J Surg 2014;12:528-33.
5. Chang JD, Kim IS, Prabhakar S, Mansukhani SA, Lee SS, Yoo JH, et al. Revision total hip arthroplasty using imageless navigation with the concept of combined anteversion. J Arthroplasty 2017;32:1576-80.
6. Franke J, Zheng G, Wendl K, Grützner PA, von Recum J. Clinical experience with computer navigation in revision total hip arthroplasty. Proc Inst Mech Eng H 2012;226:919-26.
7. Grosso P, Snider M, Muir JM. A smart tool for intraoperative leg length targeting in total hip arthroplasty: A Retrospective cohort study. Open Orthop J 2016;10:490-9.
8. Paprosky WG, Weeden SH, Bowling JW Jr. Component removal in revision total hip arthroplasty. Clin Orthop Relat Res 2001;393:181-93.
9. Sheth NP, Nelson CL, Springer BD, Fehring TK, Paprosky WG. Acetabular bone loss in revision total hip arthroplasty: Evaluation and management. J Am Acad Orthop Surg 2013;21:128-39.
10. Aljurayyan A, Tanzer D, Tanzer M. Acute revision hip arthroplasty: A previously unrecognized risk factor for heterotopic ossification. Eur J Orthop Surg Traumatol 2016;26:183-8.
11. Manzotti A, Cerveri P, De Momi E, Pullen C, Confalonieri N. Does computer-assisted surgery benefit leg length restoration in total hip replacement? Navigation versus conventional freehand. Int Orthop 2011;35:19-24.
12. Healy W. The economics of total hip arthroplasty. In: Callaghan J, Rosenberg A, Rubash H, eds. The Adult Hip. Vol 2. Philadelphia: Lippincott-Raven Publishers; 1998:845-852.
13. Sugano N, Takao M, Sakai T, Nishii T, Miki H. Does CT-based navigation improve the long-term survival in ceramic-on-ceramic THA? Clin Orthop Relat Res 2012;470:3054-9.
14. Volpin A, Khan O, Haddad FS. Theater cost is £16/Minute so what are you doing just standing there? J Arthroplasty 2016;31:22-6.
15. CIHI. Wait Times for Priority Procedures in Canada, 2017. Ottawa, ON: Canadian Institutes for Health Information; 2017.
 |
 |
 |
 |
| Mr. John Vincent | Dr. Ibrahim Alshaygy | Dr. Jeffrey M Muir | Dr. Paul Kuzyk |
| How to Cite This Article: Vincent J, Alshaygy I, Muir J. M, Kuzyk P. Preservation of the Acetabular Cup During Revision Total Hip Arthroplasty Using a Novel Mini-navigation Tool: A Case Report. Journal of Orthopaedic Case Reports 2018 Jan-Feb; 8(1): 53-56 |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com




