[box type=”bio”] Learning Point for this Article: [/box]
The untrained eye can easily miss pediatric medial condyle fractures, open reduction and internal fixation of even neglected cases gives good clinical outcome.
Case Report | Volume 8 | Issue 2 | JOCR Mar – Apr 2018 | Page 65-68| Nishit Bhatnagar, Sneha Sharma, Purushotham Lingaiah, Kameshwaran Jaikumar, Anurag Tiwari. DOI: 10.13107/jocr.2250-0685.1054
Authors: Nishit Bhatnagar[1], Sneha Sharma[2], Purushotham Lingaiah[1], Kameshwaran Jaikumar[1], Anurag Tiwari[3]
[1]Department of Orthopaedics, Maulana Azad Medical College and Lok Nayak Hospital, New Delhi, India.
[2]Department of Orthopaedics, Maulana Azad Medical College and Lok Nayak Hospital, New Delhi, India.
[3]Department of Orthopaedics, All India Institute of Medical Sciences, Bhopal, Madhya Pradesh, India.
Address of Correspondence:
Dr. Nishit Bhatnagar,
7 Godavari Apartments, Alaknanda, New Delhi, India.
E-mail: nishitbhatnagar@yahoo.co.in
Abstract
Introduction: Fractures of the medial condyle of elbow in children are rare. Diagnosis is frequently missed and many authors reported poor outcome for these fractures when treatment was delayed.
Case Report: Here, we present a case of 3-month-old ununited fracture of the medial condyle in an 8-year-old child, treated by osteosynthesis that produced good result. The patient presented to us with valgus instability of elbow and restricted range of motion. Open reduction, freshening of margins, and fixation of the ununited fragment with K-wires were done. Postoperatively, the patient regained functional range of motion and had a stable elbow.
Conclusion: Open reduction and pinning of ununited fracture medial condyle can restore good range of motion and restore elbow stability.
Keywords: Medial condyle humerus, osteosynthesis, child.
Introduction
Fractures of the medial condyle of elbow in children account for <1% of all elbow fractures [1, 2, 3]. These injuries are prone to non-union because they are intra-articular Salter-Harris Type IV injuries [4, 5]. Trochlear ossification occurs later than capitellar ossification, leading to such injuries being frequently missed [6]. Missing such fractures can lead to elbow instability, growth disturbance, and articular incongruity [7]. Many authors reported poor outcome for these fractures when treatment was delayed [6, 7, 8]. Here, we present a case of ununited fracture of the medial condyle in a child, treated by osteosynthesis that produced good result.
Case Report
An 8-year-old girl fell from a height of around 1.5 m and injured her left elbow. She was examined by a physician in her village and diagnosed as having an elbow sprain for which limb was immobilized in a plaster cast for 3 weeks. The child sustained another injury to the same elbow following fall on her outstretched hand 4 weeks after removal of the cast. Again the elbow was immobilized in a long arm cast for 3 weeks. After removal of the cast, the child complained of persistent pain and discomfort in the elbow. She was then referred to our hospital 3 months after the initial injury. Examination revealed a stiff elbow with a painless range of motion from 45° to 90°, with only terminal limitation of pronation and supination. The ununited fragment was palpable separately from the rest of the distal humerus and freely mobile. Valgus instability was also noted. There were no signs of ulnar nerve irritability or deficit. An anteroposterior and lateral radiographs revealed a displaced fragment of the medial condyle involving the trochlea (Fig. 1).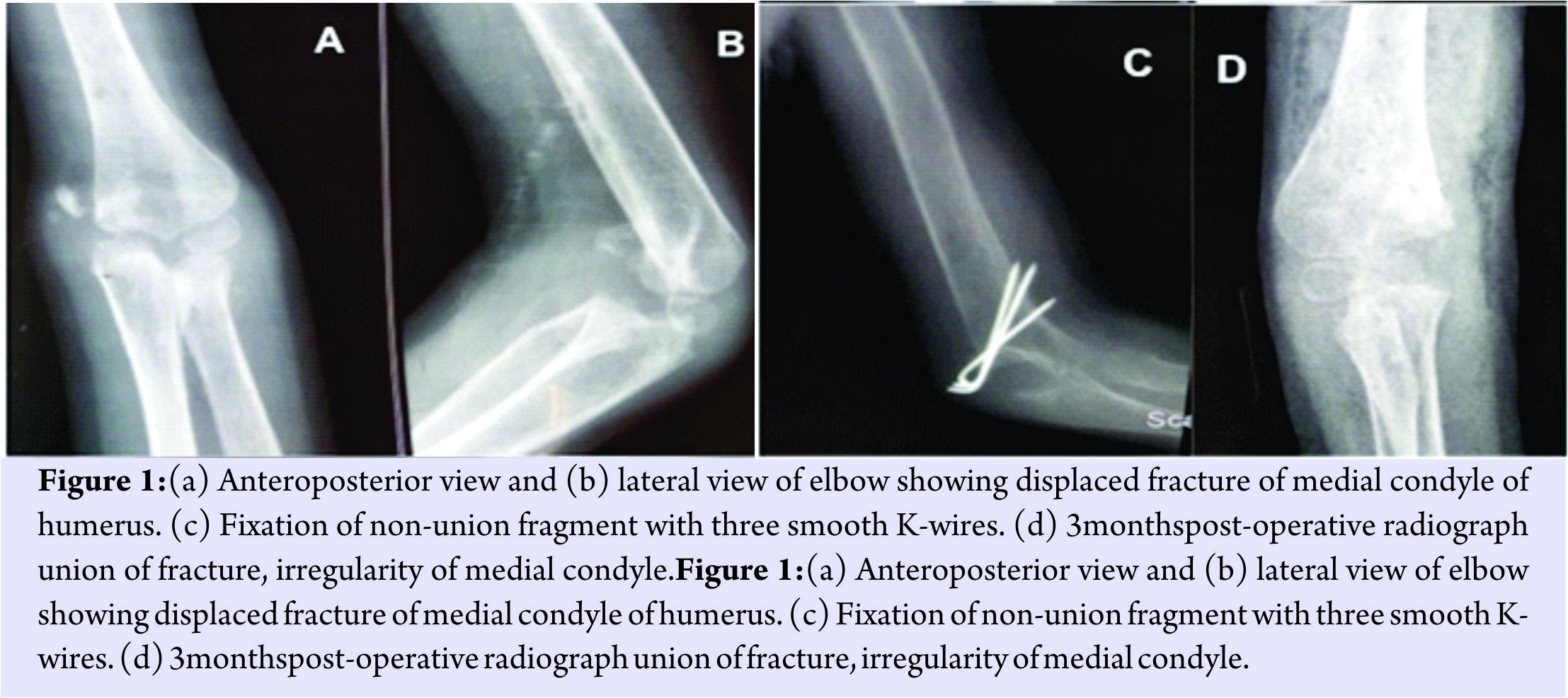
To address the limitation of movement, articular incongruity and elbow instability, open reduction, and fixation of the fracture was planned. After obtaining consent from the parents, the patient was administered general anesthesia and positioned supine on the operating table with arm abducted on arm board. Limb was exsanguinated and surgery was commenced under tourniquet. Incision was made directly over the medial condyle fragment. The ulnar nerve was identified and protected with plastic tube. The medial condyle fragment was found displaced proximally and anteriorly. The fragment was rotated with its cancellous surface lying anteriorly. This surface was freshened with a curette. Fracture surface on the humeral side was identified and freshened. Medial articular edge of distal humerus was identified for accurate reduction. Without any undue soft tissue stripping, the fractured fragment was reduced to the best possible position with approximation of articular surfaces. Fixation with three smooth Kirschner (K) wires was done followed by suturing of surgical wound. Long arm cast was applied with elbow at 90° and forearm in mid-prone position. There were no post-operative complications.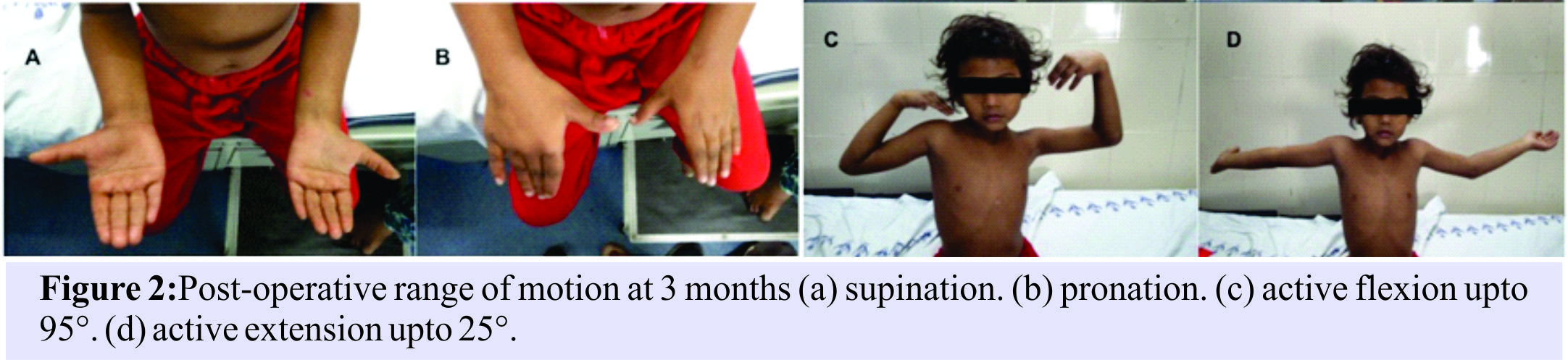
Considering that the fracture was already 3 months old at the time of surgery, we anticipated that a longer duration of immobilization would be required; hence, the cast and K-wires were removed at 6 weeks under local anesthesia. Active and active-assisted elbow range of motion exercises were started after K-wire removal. Radiographs taken at 3-month follow-up show union of the fracture, with an irregular medial condyle. The patient regained an active flexion arc of 25° to 95°, with complete pronation and supination (Fig. 2). Passively 20° to 100° arc of motion had been restored. At 6-month follow-up range from 10° to 120° had been restored and there was no coronal plane deformity.
Discussion
Fractures of the medial condyle of humerus usually occur between the ages of 8 and 12 years [1, 4]. The diagnosis is frequently missed in young children since the trochlear ossification center appears from the age of 7 to 13 years [9]. Two mechanisms of injury are described for medial condyle fractures in children. One is a direct blow to the posterior proximal ulna while the elbow is flexed, splitting off the medial condyle. The second mechanism is a fall on outstretched hand with elbow extended, forearm supinated, and wrist dorsiflexed, leading to avulsion of the medial condyle [10]. These fractures are produced by trauma of significant force and hence can be associated with other injuries around the elbow as well like elbow dislocation and radial head dislocation [2, 4]. Medial condyle fractures were classified by Kilfoyle into three types based on the degree of displacement [10]. He reported favorable results even in completely displaced fractures when diagnosed and treated early. Papavasiliou reported excellent outcomes of conservative treatment for non-displaced fractures (Type I and II Kilfoyle) [1]. Since these fractures are frequently missed, they have high chances of complications such as limitation of movements, physeal arrest, and delayed ulnar nerve palsy [1, 3, 4, 11]. Non-union has been reported in 7.4–33.3% of patients by different authors when left untreated [5, 6, 12]. Trochlea has a tenuous blood supply provided by terminal branches with no collateral circulation. Open reduction carries the risk of avascular necrosis of trochlea and non-union if the posterior condyle is stripped off during surgery [7]. However, the ulnar nerve is at risk in closed percutaneous pinning [13]. Demiroglu published one of the largest series on medial condyle fractures in children and recommended early open reduction and percutaneous pinning for rotated and/or displaced fractures [14]. Mitsunaga and Helfet separately described osteosynthesis for medial condylar non-union in adults [15, 16]. However, there are very few reports of ununited or non-union medial condyle in children (Table 1). Papavasiliou et al. and Varma in their separate reports described the success of supracondylar osteotomy for correcting cubitus varus associated with non-union medial condyle [1, 5]. Song et al. reported a case of rotated fracture of medial condyle managed conservatively, with the ultimate outcome of non-union at the fracture site [17]. However, the good clinical outcome was obtained following open reduction, freshening of fracture site, and K-wire pinning. They also advocated maintaining K-wires and cast for 6 weeks duration. Ryu et al. reported an adolescent with non-union medial condyle managed by osteosynthesis with good long-term clinical outcome [11].
Conclusion
Conclusions cannot be drawn from a single case, however, we believe that early diagnosis and management is of utmost importance for good outcome. Review of literature suggests that non-displaced fractures of medial condyle should be managed conservatively with cast immobilization for 4 weeks. Displaced or rotated fractures are best managed by open reduction and K-wire fixation. For delayed presentation or established non-union medial condyle, we prefer open reduction and percutaneous pinning, with emphasis on minimal soft tissue stripping of the fragment to prevent trochlear avascular necrosis.
Clinical Message
Medial condyle fractures can be easily missed in the pediatric age group by the untrained eye. Keeping a high index of suspicion is of utmost importance. In ununited fractures or established non-union, open reduction and pinning can give satisfactory results.
References
1. Papavasiliou V, Nenopoulos S, Venturis T. Fractures of the medial condyle of the humerus in childhood. J Pediatr Orthop 1987;7:421-3.
2. Bensahel H, Csukonyi Z, Badelon O, Badaoui S. Fractures of the medial condyle of the humerus in children. J Pediatr Orthop 1986;6:430-3.
3. Chacha PB. Fracture of the medical condyle of the humerus with rotational displacement. Report of two cases. J Bone Joint Surg Am 1970;52:1453-8.
4. Leet AI, Young C, Hoffer MM. Medial condyle fractures of the humerus in children. J Pediatr Orthop 2002;22:2-7.
5. Varma BP, Srivastava TP. Fracture of the medial condyle of the humerus in children: A report of 4 cases including the late sequelae. Injury 1972;4:171-4.
6. Fowles JV, Kassab MT. Displaced fractures of the medial humeral condyle in children. J Bone Joint Surg Am 1980;62:1159-63.
7. Hanspal RS. Injury to the medial humeral condyle in a child reviewed after 18 years. Report of a case. J Bone Joint Surg Br 1985;67:638-9.
8. Cothay DM. Injury to the lower medial epiphysis of the humerus before development of the ossific centre. Report of a case. J Bone Joint Surg Br 1967;49:766-7.
9. Harrison RB, Keats TE, Frankel CJ, Anderson RL, Youngblood P. Radiographic clues to fractures of the unossified medial humeral condyle in young children. Skeletal Radiol 1984;11:209-12.
10. Kilfoyle RM. Fractures of the medial condyle and epicondyle of the elbow in children. Clin Orthop Relat Res 1965;41:43-50.
11. Ryu K, Nagaoka M, Ryu J. Osteosynthesis for nonunion of the medial humeral condyle in an adolescent: A case report. J Shoulder Elbow Surg 2007;16:e8-12.
12. Ghawabi MH. Fracture of the medial condyle of the humerus. J Bone Joint Surg Am 1975;57:677-80.
13. Gosens T, Bongers KJ. Neurovascular complications and functional outcome in displaced supracondylar fractures of the humerus in children. Injury 2003;34:267-73.
14. Demiroglu M, Kilic B, Unay K, Ozkan K, Aydın D. Open reduction and percutaneous pinning for medial condyle fractures of elbow in children: Is it a risk for complications? Int J Res Orthop 2016;2:36-39.
15. Mitsunaga MM, Bryan RS, Linscheid RL. Condylar nonunions of the elbow. J Trauma 1982;22:787-91.
16. Helfet DL, Kloen P, Anand N, Rosen HS. Open reduction and internal fixation of delayed unions and nonunions of fractures of the distal part of the humerus. J Bone Joint Surg Am 2003;85-A:33-40.
17. Song KS, Ramnani K, Cho CH, Son ES. Late diagnosis of medial condyle fracture of the humerus with rotational displacement in a child. J Orthop Traumatol 2011;12:219-22.
 |
 |
 |
 |
 |
| Dr. Nishit Bhatnagar | Dr. Sneha Sharma | Dr. Purushotham Lingaiah |
Dr. Kameshwaran Jaikumar |
Dr. Anurag Tiwari |
| How to Cite This Article: Bhatnagar N, Sharma S, Lingaiah P, Jaishankar K, Tiwari A. Ununited Fracture Medial Condyle in a Child: A Case Report and Review of Literature. Journal of Orthopaedic Case Reports 2018 Mar-Apr;8(2):65-68. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com




