[box type=”bio”] Learning Point for the Article: [/box]
Retroperitoneal hemorrhage causing neurological compression is an unusual suspect in patients receiving thrombolytic therapy that requires sharp-eyed heedfulness.
Case Report | Volume 8 | Issue 3 | JOCR May – June 2018 | Page 55-57| Vishesh Khanna, Munis Ashraf, Senthil Nathan Sambandam. DOI: 10.13107/jocr.2250-0685.1106
Authors: Vishesh Khanna[1], Munis Ashraf[2], Senthil Nathan Sambandam[3]
[1]Department of Orthopaedics, Arthroplasty Fellow, Sunshine Hospital, Secunderabad, Telangana, India.
[2]Department of Orthopaedics, K.G Hospital and Postgraduate Medical Institute, Coimbatore, Tamil Nadu, India.
[3]Department of Orthopaedics, Louis A Johnson VA Medical Center, Clarksburg, West Virginia, USA.
Address of Correspondence:
Dr. Vishesh Khanna,
Arthroplasty Fellow, Sunshine Hospital. Secunderabad – 500 003, Telangana, India.
E-mail: visheshkhanna85@gmail.com
Abstract
Introduction: Retroperitoneal hemorrhage has been sparsely reported with warfarin therapy. In this paper, we describe a case of spontaneous retroperitoneal hematoma causing femoral neuropathy following treatment with low molecular weight heparin.
Case Report: A 65-year-old gentleman had presented with acute onset left-sided thigh pain, paraesthesia, and weakness along with lower backache. On deeper introspection, our patient had, in the recent past, been thrombolyzed for pulmonary embolism. The clinical examination led us to suspect an acute lumbar pathology, and he was investigated on those lines. Imaging studies, however, revealed a massive retroperitoneal hemorrhage which was the cause of femoral neuropathy. In this case report, the presentation of this rare association has been discussed with special emphasis on clinical premonition in the background of anticoagulant therapy. Watchful and medical treatment yielded successful recovery at follow-up.
Conclusion: Cautious clinical assessment is needed in patients taking anticoagulant therapy. The presentation of a femoral neuropathy is often intriguing. Management options include careful observation and emergency decompression in cases of worsening neurological status.
Keywords: Femoral neuropathy, low molecular weight heparin, spontaneous retroperitoneal hematoma.
Introduction
Retroperitoneal hemorrhage is seen most frequently following femoral artery catheterization and trauma. Hemorrhage can also result from aneurysms, renal or suprarenal pathologies. Occasionally, a spontaneous atraumatic variant of retroperitoneal hematoma can occur. This potentially life-threatening lesion can be observed in recipients of anticoagulant therapy or patients with clotting disorders. The reported incidence of such hemorrhage following anticoagulant therapy is 1.3% and 6.6% [1]. An uncommon presentation of femoral neuropathy with an underlying retroperitoneal hematoma is illustrated here.
Case Report
A 65-year-old gentleman presented to our hospital with sudden onset of pain, swelling, weakness and paresthesia over the front of his left thigh and lower back. His symptoms had progressed and worsened over a week and had restricted him to the bed. There was no history of recent trauma. The patient was a smoker, and previous medical history included treatment for pulmonary embolism with anticoagulants [low molecular weight heparin] about a month ago. There was no history of any drug allergy.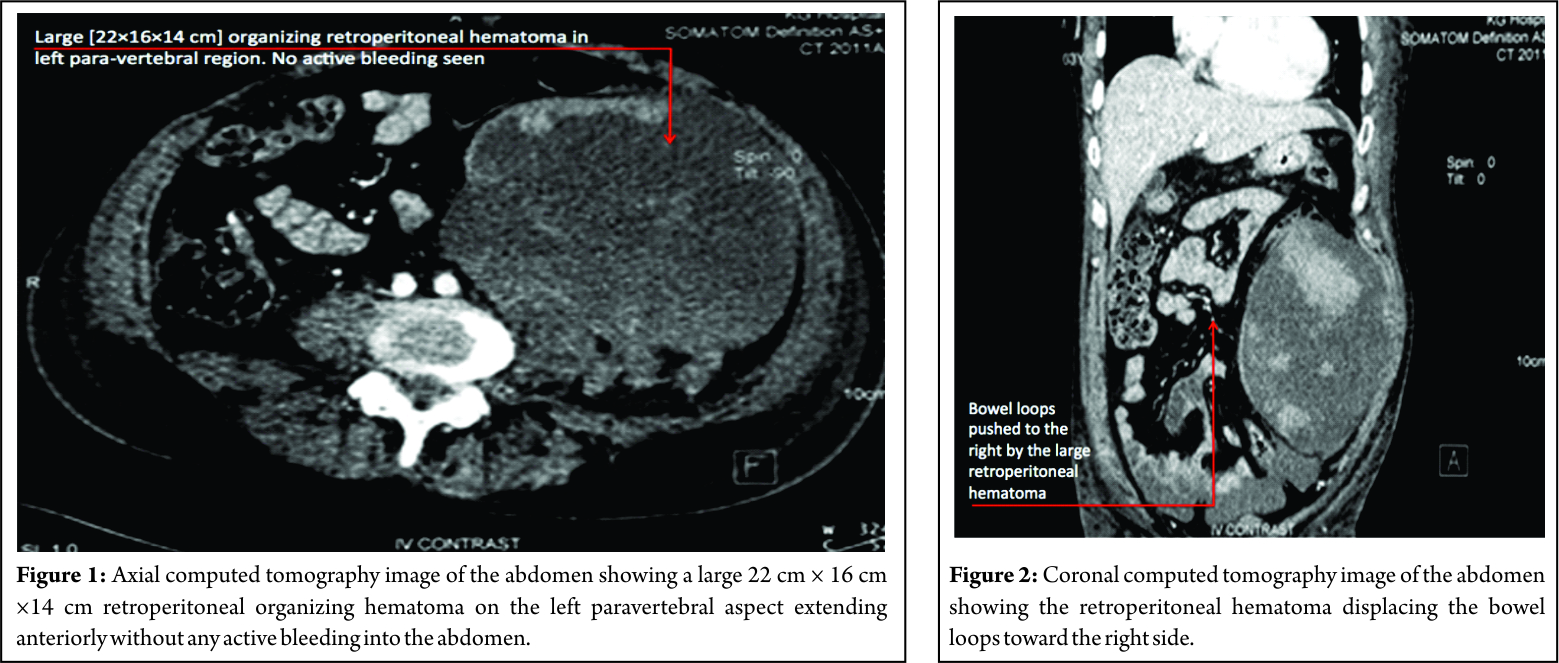
On clinical examination, he had a distended abdomen, pitting edema over the left lumbar region and left thigh, with weak (Grade 2) quadriceps along with reduced sensations over the anterior thigh. His knee reflex was absent on the left side, and hip and knee movements were painful. Left femoral pulse was feeble, and the patient was unable to perform a straight leg raise. Movements of opposite hip and knee were full and pain-free with an intact neurovascular status. Investigations had revealed that the total counts, renal parameters, and liver enzymes were elevated with a hemoglobin of 8 g/dl. Ultrasound abdomen revealed a large mass in the left hypochondrium and iliac region which was confirmed as a retroperitoneal organizing hematoma contiguous with the left psoas and iliacus without any active bleeding in the abdomen. The massive dimensions of the lesion were 22 cm × 16 cm × 14 cm (Fig. 1 and 2). The case was managed conservatively with cessation of anticoagulants, limb elevation and bed rest and had made complete neurological recovery at subsequent follow-up at 1 month.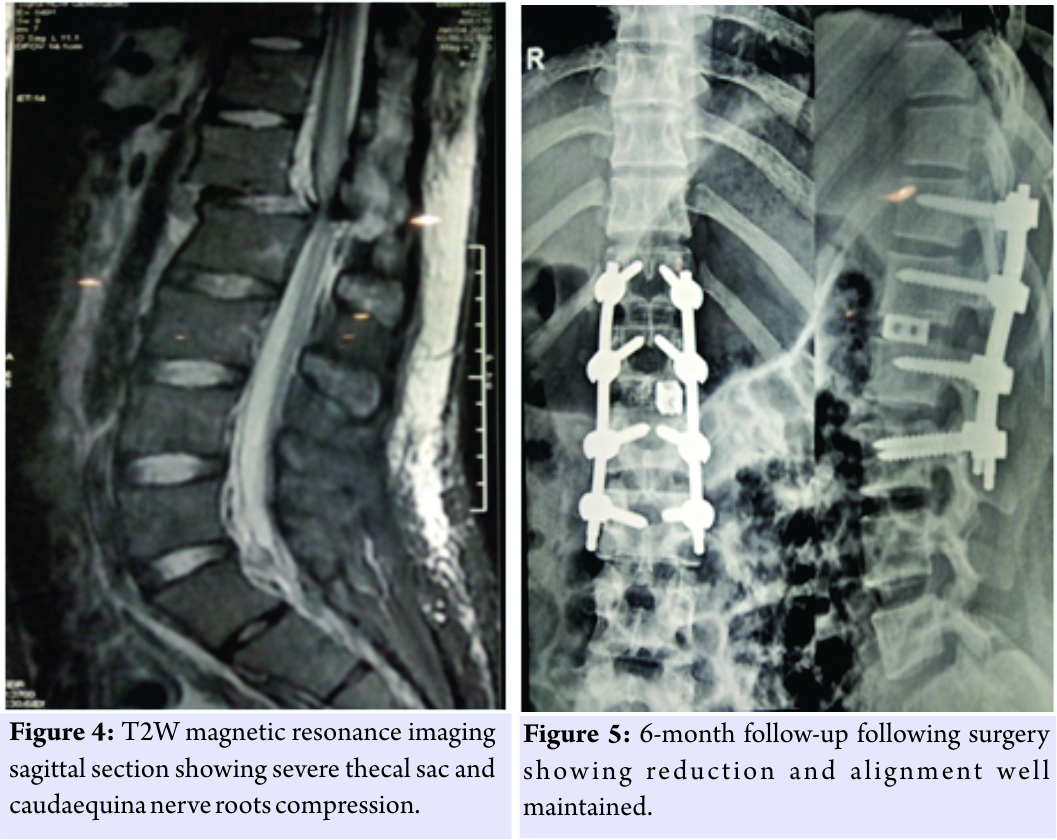
Discussion
In current practice, the indications for anticoagulant use are expanding as a result, of which complications arising from therapy are undeniably bound to increase [2]. Over the years, there has been a drift toward the use of low molecular heparin from warfarin and its derivatives for treating venous thromboembolism among physicians. While reports suggestive of neuropathy attributable to warfarin have surfaced in the past, only a few have ascribed this complication to heparin therapy [3, 4]. Isolated cases of bilateral femoral neuropathy [5] and meralgia paresthetica [6] due to iliopsoas hematoma with anticoagulant therapy have made an intuitive and conjectural diagnosis of this entity, plausible, and foreseeable in these distinct conditions. The typical clinical presentation, often with pain, weakness, and numbness of thigh, mandates ultrasound and tomography to ascertain the extent and magnitude of the lesion.
Cadaveric studies have demonstrated that while the iliacus muscle can expand to its maximum limit of 150 ml, the psoas has a much higher capacity to tumefy [6]. These findings are only suggestive of the significant amount of blood that these muscles can hold even before the patient is symptomatic. A review of the literature demonstrates that there has been no consensus regarding the treatment of choice. Aggressive decompression has been propounded to forestall impending neurological deficits with inflated intramuscular tension [7, 8]. As with our case, conservative management can be effective provided the patient is hemodynamically stable and is monitored regularly [9]. Modification or cessation of anticoagulant therapy, correction of the hemodynamic state with volume resuscitation stabilization by adequate transfusion and supportive measures form the pillars of medical treatment. It is to be noted that a progressive hematoma with evidence of neurological worsening decrees an urgent decompression and drainage [10].
Conclusions
Vigilance in patients on heparin can help in prompt recognition of neurological complications that may inadvertently stem from this therapy. Typical features of femoral nerve compression are redolent and should be timely heeded to lest permanent neurological impairment may ensue. Management options can range from medical, conservative therapy to emergency decompression in patients with worsening neurological status.
Clinical Message
Retroperitoneal hematoma causing femoral neuropathy can occur in a patient on anticoagulants. A high index of suspicion should help in immediate recognition of neurological signs and swift initiation of therapy. Treatment options of decompression or conservative management can be based on patients’ general condition and the extent of hematoma.
References
1. Tosun A, Inal E, Keles I, Tulmaç M, Tosun Ö, Aydin G, et al. Conservative treatment of femoral neuropathy following retroperitoneal hemorrhage: A case report and review of literature. Blood Coagul Fibrinolysis 2014;25:769-72.
2. Parmer SS, Carpenter JP, Fairman RM, Velazquez OC, Mitchell ME. Femoral neuropathy following retroperitoneal hemorrhage: Case series and review of the literature. Ann Vasc Surg 2006;20:536-40.
3. Brantigan JW, Owens ML, Moody FG. Femoral neuropathy complicating anticoagulant therapy. Am J Surg 1976;132:108-9.
4. Gurbuz O, Ercan A, Kumtepe G, Karal IH, Velioglu Y, Ener S, et al. Femoral nerve palsy due to anticoagulant induced retroperitoneal hematoma. Case Rep Med 2014;2014:450750.
5. Macauley P, Soni P, Akkad I, Demir S, Shankar S, Kakar P, et al. Bilateral femoral neuropathy following psoas muscle hematomas caused by enoxaparin therapy. Am J Case Rep 2017;18:937-40.
6. Satpathy J, Mounasamy V, Golladay G, Reynolds JP. Retroperitoneal hematoma presenting as acute meralgia paresthetica: Case report, review of literature and cadaveric demonstration. J Case Reports Images Orthop Rheumatol 2016;1:6-11.
7. Merrick HW, Zeiss J, Woldenberg LS. Percutaneous decompression for femoral neuropathy secondary to heparin-induced retroperitoneal hematoma: Case report and review of the literature. Am Surg 1991;57:706-11.
8. Chan YC, Morales JP, Reidy JF, Taylor PR. Management of spontaneous and iatrogenic retroperitoneal haemorrhage: Conservative management, endovascular intervention or open surgery? Int J Clin Pract 2008;62:1604-13.
9. Seijo-Martínez M, Castro del Río M, Fontoira E, Fontoira M. Acute femoral neuropathy secondary to an iliacus muscle hematoma. J Neurol Sci 2003;209:119-22.
10. Mastroianni PP, Roberts MP. Femoral neuropathy and retroperitoneal hemorrhage. Neurosurgery 1983;13:44-7.
 |
 |
 |
| Dr. Vishesh Khanna | Dr. Munis Ashraf | Dr. Senthil Nathan Sambandam |
| How to Cite This Article: Khanna V, Ashraf M, Sambandam SN. Spontaneous Retroperitoneal Hematoma Presenting as Femoral Neuropathy in a Patient on Low Molecular Weight Heparin Therapy. Journal of Orthopaedic Case Reports 2018. May- June; 8(3): 55-57 |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com




