[box type=”bio”] Learning Point of the Article: [/box]
This case report would like to emphasise the importance of keeping in mind a rare diagnosis, essential thrombocytosis, in femoral head transient osteoporosis.
Case Report | Volume 9 | Issue 1 | JOCR January – February 2019 | Page 41-44 | Murat Altan, Serkan Bayram, Ahmet Salduz, Emre Özmen, Mehmet Ekinci. DOI: 10.13107/jocr.2250-0685.1300
Authors: Murat Altan[1], Serkan Bayram[1], Ahmet Salduz[1], Emre Özmen[1], Mehmet Ekinci[1]
[1]Department of Orthopaedics and Traumatology, Istanbul University Istanbul Medical Faculty, Istanbul, Turkey.
Address of Correspondence:
Dr. Murat Altan,
Department of Orthopaedics and Traumatology, Istanbul University Istanbul Medical Faculty, Fatih- ,İstanbul—- 34098–, Turkey.
E-mail: altanmurat88@gmail.com
Abstract
Introduction: Transient osteoporosis(TO), also known as bone marrow edema syndrome, is characterized by marrow edema which causes increasing of intramedullary pressure. Among the other causes, such as third-trimester pregnancy, impaired circulation may also be caused by changes in normal blood counts such as thrombocytosis. There are multiple reports in the literature of secondary femoral head TO transient osteoporosis; however, there is no case report of femoral head TO transient osteoporos is specifically secondary to essential thrombocytosis (ET) in literature. Herein, we present ET essential thrombocytosisas an unusual cause of TO transient osteoporosis of the femoral head.
Case Report: A 33-year-old male presented himself to our clinic with severe left hip pain. The patient has painful hip motions and itching after the bath and episodic chest pain. Family history is positive for hematological malignancy. Complete blood count (CBC)test showed an increased level of thyrombocytes and haematology opinion obtained. The genetic analysis was positive for Janus kinase 2JAK2V617F and patient was diagnonsed as ET essential thrombocytosis. Besides, to eliminate the symptoms of the hip, the surgical intervention had planned and the patient had a dramatic pain relief during follow-up.
Conclusion: ET Essential thrombocytosisis a myeloproliferative disorder and has a good prognosis. TO Transient osteoporosis could be accompanied with hematologic disorders, especially myeloproliferative diseases. Based on our review of literature, this is the first case with ET essential thrombocytosis and TO transient osteoporosis of the hip.
Keywords: Decompression, essential thrombocytosis, transient osteoporosis. transient osteoporosis, decompression, essential thrombocytosis
Introduction
Chronic myeloproliferative diseases are hematological malignities characterized by uncontrolled proliferation of myeloid precursor cells. These are, namely, chronic myeloid leukemia, polycythemia vera, chronic myelofibrosis, chronic eosinophilic leukemia, chronic neutrophilic leukemia, mastocytosis, and essential thrombocytosis (ET). About 80% of people with chronic myeloproliferative diseases have a contributing acquired gene mutation. This gene may involve the Janus kinase 2 (JAK2), calreticulin, or MPL gene mutation. The most common cause of death is due to thrombotic complications [1]. ET is a breakpoint cluster region-abelson (−) chronic myeloproliferative disease that presents with isolated thrombocytosis. It has the longest average survival among chronic myeloproliferative disorders. Patients are usually asymptomatic at the time of diagnosis. In cases of incidentally detected thrombocytosis, causes of reactive thrombocytosis must be excluded. Many conditions, physiological and pathological (infections, neoplasia, tissue damage, etc.) may cause thrombocytosis. Femoral head transient osteoporosis (TO) is a disease that usually affects people in the third decade. The exact prevalence of TO of the femoral head is unknown. A variety of traumatic and atraumatic factors contribute to the etiology of TO; however, third-trimester pregnancy is associated with most of the atraumatic cases. Avascular necrosis of the femoral head, septic arthritis, and some inflammatory joint diseases should be considered in the differential diagnosis. Mainly it is challenging to distinguish between avascular necrosis of the femoral head and TO of the hip [2]. Some authors declared that the TO of the hip might be an earlier phase of the avascular necrosis of the femoral head [3]. However, it is reported by Yamamoto et al., hematopoietic and fatty elements are affected through ischemic insult in TO of the hip, whereas cell deaths include osteocytes in femoral head avascular necrosis [4]. There are multiple reports in literature of transient secondary osteoporosis of the hip due to chronic myeloproliferative diseases; however, we have not encountered any case report of TO of the femoral head specifically secondary to ET in literature yet. We would like to present ET as an unusual cause of TO of the femoral head.
Case Report
A 33-year-old male patient presented to orthopedics and traumatology outpatient clinic with left hip pain. The pain started suddenly 3 months ago while walking and the patient were conservatively treated. Due to pain did not subside despite conservative therapy, magnetic resonance imaging (MRI) scan was performed. It showed bone marrow edema of the left femoral head, and consequently, the patient was referred to our tertiary clinic to have surgery. Patient’s history was significant for palpitations, itching after the bath and episodic chest pain starting approximately 3 months ago. The patient also complained of paresthesias at the hands, feet, and back of the neck 6–7 months ago and his medical history was unremarkable including steroids, and he did not have any concomitant diseases. Patients medical and surgical history were unremarkable; however, family history was positive for a hematological malignancy in his sibling. The patient was using crutches. Inspection of the hips and lower extremities was normal. Passive flexion and extension of the left hip elicited pain with normal range of motion. Internal rotation of the left hip was painful and restricted, while external rotation was normal with the full range of motion. The neurovascular examination was unremarkable. The anterior-posterior and lateral X-ray of the hips were taken (Fig. 1).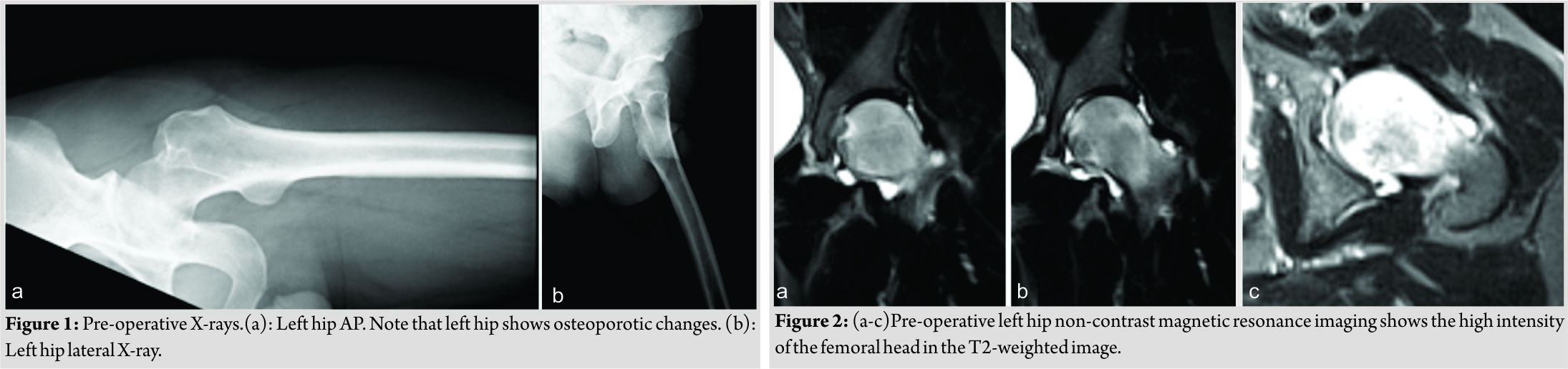 MRI shows increased intensity on T2-weighted images (Fig. 2). Patient’s complete blood count (CBC) done at another hospital showed thrombocyte count of 609 103/µL whereas other parameters were in normal range. At the time of presentation, CBC was normal except the thrombocyte level (644 103/µL). Considering the presenting symptoms and diagnostic tests of the patient, the initial diagnosis was established as ET, hematology opinion obtained. A genetic analysis was positive for JAK2 V617F. Repeated hemograms during the follow-up showed increasing thrombocyte counts (665 103/µL and 769 103/µL, respectively) which support the diagnosis. To prevent possible thrombotic complications, the patient was started on acetylsalicylic acid and hydroxyurea and the patient has scheduled a bone marrow biopsy. While protein electrophoresis was normal, bone scintigraphy showed significantly increased activity in the left femoral head and acetabular region. The patient was diagnosed with TO of the hip and core decompression was planned to eliminate compressive symptoms of the hip.
MRI shows increased intensity on T2-weighted images (Fig. 2). Patient’s complete blood count (CBC) done at another hospital showed thrombocyte count of 609 103/µL whereas other parameters were in normal range. At the time of presentation, CBC was normal except the thrombocyte level (644 103/µL). Considering the presenting symptoms and diagnostic tests of the patient, the initial diagnosis was established as ET, hematology opinion obtained. A genetic analysis was positive for JAK2 V617F. Repeated hemograms during the follow-up showed increasing thrombocyte counts (665 103/µL and 769 103/µL, respectively) which support the diagnosis. To prevent possible thrombotic complications, the patient was started on acetylsalicylic acid and hydroxyurea and the patient has scheduled a bone marrow biopsy. While protein electrophoresis was normal, bone scintigraphy showed significantly increased activity in the left femoral head and acetabular region. The patient was diagnosed with TO of the hip and core decompression was planned to eliminate compressive symptoms of the hip.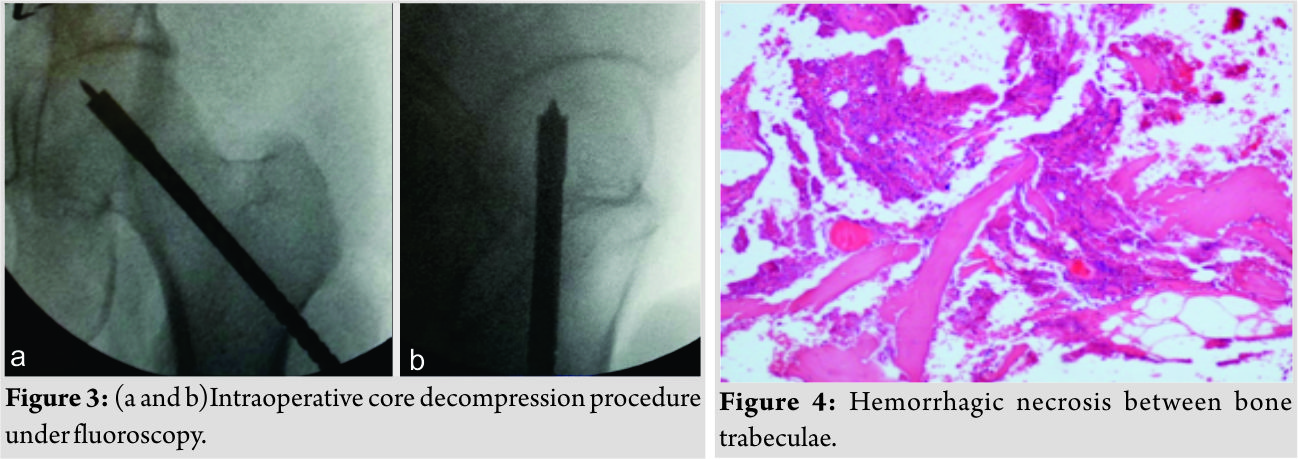
Procedure
The surgery was performed on the traction table. An 8 mm drill was used for decompression targeting femoral head (Fig. 3). During the procedure bone marrow, and femoral head biopsies were performed, and the materials were sent for histopathological examination. The results of the per-operative samples came out as “marrow parenchyma including fields of necrosis” and “hemorrhagic necrosis between bone trabeculae” (Fig. 4). The results of the bone marrow biopsy from the posterior iliac crest were“focal megakaryocytic dysplasia.” The symptoms, blood tests, and bone marrow biopsy were consistent with ET which was diagnosed by the hematologist. In the post-operative follow-up of the patient, there was no hip pain at 2years, and thrombocyte count was 463 103/µL. X-ray has no specific changes (Fig. 5), and MRI shows a decreasing of the intensity of edema (Fig. 6).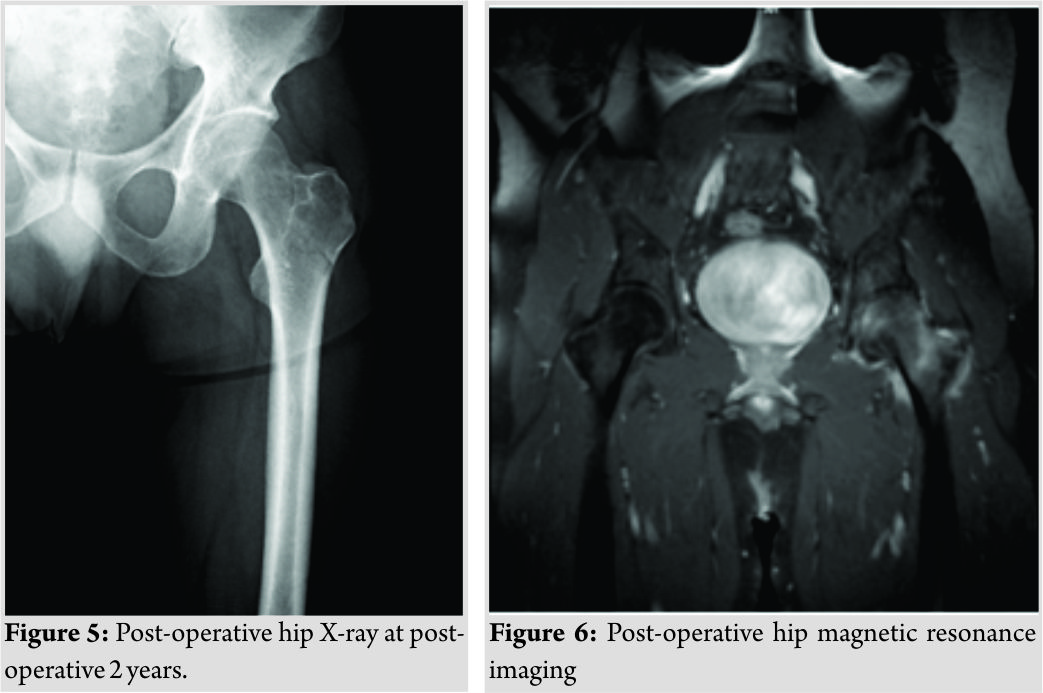
Discussion
Etis one of the chronic myeloproliferative diseases. The disease usually courses asymptomatic and must be considered in cases of isolated thrombocytosis noticed through routine blood work-up. Before making the diagnosis, the causes of reactive thrombocytosis must be excluded as well. The criteria for ET were revised in 2015 [5] while ET is known as the subtype among chronic myeloproliferative diseases with the best prognosis, thrombotic complications may be, and most of the mortality develops in this background [1]. Signs and symptoms depend on where the clot forms. Our patient has an unusual presentation with severe left hip pain. Blood tests showed high thrombocytes. In the patient’s history, itching after the shower was a clue to consider the ET. A sign and symptoms put together, we considered ET in the orthopedic outpatient clinic initially. The diagnosis was confirmed by the hematologist due to the fulfillment of the WHO criteria [5]. MRI without contrast is the gold standard in diagnosing osteonecrosis of the femoral head [6]. Technetium 99 bone scintigraphy and single-photon emission computed tomography (SPECT) is also useful in the diagnosis of avascular necrosis; with scintigraphy having a sensitivity of 78–83% and specificity 75–83%, and SPECT having a sensitivity of 92% and specificity of 78%, respectively [7, 8]. TO is an uncommon condition among the population. The exact prevalence of the TO is unknown; however, diagnosed more frequently in healthy middle-aged men with a male:female ratio of 3:1 [9, 10]. TO is a self-limiting condition, and the treatment in patients with TO of the hip mostly includes conservative modalities. Among non-operative strategies are decreasing weight load comes initially, then bisphosphonates (to decrease osteoclast activity), hyperbaric oxygen, and extracorporeal shock wave therapy treatment. As antilipolytic and anti-coagulant medications statins, anticoagulants and vasodilators can be used. Operative treatment options include core decompression, which the local pressure of the femoral head to extinguish the symptoms. The most commonly employed surgical treatment is core decompression for TO of the femoral head. The theoretical advantage of core decompression is relieving the intraosseous pressure, allowing increased vascularity and reduces edema. While there have been reports TO due to chronic myeloproliferative diseases in literature, we were unable to find any reports of femoral head TO due to ET. Therefore, although rare, ET must be considered in the differential diagnosis of the TO of the femoral head.
Conclusion
To of the hip is a rare diagnosis in middle-aged population and places a significant burden on the workforce. In patients with femoral head TO, underlying conditions must be inquired, and the treatment should take a multidisciplinary approach according to the etiology. ET, one of the rare reasons for the TO of femoral head, should be considered in the differential diagnosis.
Clinical Message
Toof the femoral head is seen rarely and often overlooked. In some hematologic disorders; involvement of the femoral head is common and could be the major cause of the disability and patient dissatisfaction. TO of the femoral head should always be kept in mind in patients with hematologic disorders, especially in myeloproliferative disorders.
References
1. Harrison CN. Current trends in essential thrombocythaemia. Br J Haematol 2002;117:796-808.
2. Reddy KB, Sareen A, Kanojia RK, Prakash J. Transient osteoporosis of the hip in a non-pregnant woman. BMJ Case Rep 2015;2015:bcr2015209287.
3. Ma FY, Falkenberg M. Case reports: Transient osteoporosis of the hip: An atypical case. Clin Orthop Relat Res 2006;445:245-9.
4. Yamamoto T, Kubo T, Hirasawa Y, Noguchi Y, Iwamoto Y, Sueishi K, et al. A clinicopathologic study of transient osteoporosis of the hip. Skeletal Radiol 1999;28:621-7.
5. Barbui T, Thiele J, Vannucchi AM, Tefferi A. Rationale for revision and proposed changes of the WHO diagnostic criteria for polycythemia vera, essential thrombocythemia and primary myelofibrosis. Blood Cancer J 2015;5:e337.
6. Amanatullah DF, Strauss EJ, Di Cesare PE. Current management options for osteonecrosis of the femoral head: Part 1, diagnosis and nonoperative management. Am J Orthop (Belle Mead NJ) 2011;40:E186-92.
7. Beltran J, Burk JM, Herman LJ, Clark RN, Zuelzer WA, Freedy MR, et al. Avascular necrosis of the femoral head: Early MRI detection and radiological correlation. Magn Reson Imaging 1987;5:431-42.
8. Oshima M, Yoshihasi Y, Ito K, Asai H, Fukatsu H, Sakuma S, et al. Initial stage of legg-calve-perthes disease: Comparison of three-phase bone scintigraphy and SPECT with MR imaging. Eur J Radiol 1992;15:107-12.
9. Hadidy AM, Al Ryalat NT, Hadidi ST, Tarawneh ES, Hadidi MT, Samara OA, et al. Male transient hip osteoporosis: Are physicians at a higher risk? Arch Osteoporos 2009;4:41-5.
10. Niimi R, Sudo A, Hasegawa M, Fukuda A, Uchida A. Changes in bone mineral density in transient osteoporosis of the hip. J Bone Joint Surg Br 2006;88:1438-40.
 |
 |
 |
 |
| Dr. Serkan Bayram | Dr. Ahmet Salduz | Dr. Emre Özmen | Dr. Mehmet Ekinci |
| How to Cite This Article: Altan M, Bayram S, Salduz A, Özmen E, Ekinci M. An Unusual Cause of the Transient Osteoporosis of the Femoral Head: Essential Thrombocytosis. Journal of Orthopaedic Case Reports 2019 Jan-Feb; 9(1): 41-44. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com




