[box type=”bio”] Learning Point of the Article: [/box]
Limb salvage is an option even for advanced bone and soft tissue tumours with appropriate indications, to provide the best quality of life.
Case Report | Volume 9 | Issue 1 | JOCR January – February 2019 | Page 58-61| Pramod Chinder, Suraj Hindiskere, Srinath Doddarangappa, Utkarsh Pal, Kiran Tej Daggupati. DOI: 10.13107/jocr.2250-0685.1308
Authors: Pramod Chinder[1], Suraj Hindiskere[1, 2], Srinath Doddarangappa[1], Utkarsh Pal[1], Kiran Tej Daggupati[2]
[1]Department of Musculoskeletal Oncology, HCG Hospital, Bengaluru, India,
[2]Department of Orthopaedics, M S Ramaiah Medical College, Bangalore, India.
Address of Correspondence:
Dr. Suraj Hindiskere,
Department of Musculoskeletal Oncology, HCG Hospital, No 8, HCG Towers, P. Kalinga Rao Road, Sampangi Ram Nagar, Bengaluru, India.
E-mail: suraj.ortho@gmail.com
Abstract
Introduction: Ewing’s sarcoma (ES) is a malignant tumor of the bone and soft tissue arisingfrom the neuroectodermal cells. It commonly arises from the extremities of children and young adults and very rarely from flat bones like the scapula. Locally advanced disease with prior history of surgery and poor response to neoadjuvant chemotherapy in a bedridden patient is usually treated by forequarter amputation, considering the anatomical complexity of the shoulder girdle.
Case Report: A young adult diagnosed and previously operated forES of the left scapula,presented to us with a massive fungating mass over the left upper back, excruciating pain and inability to use the left upper limb. Limb salvage surgery was performed, followed by adjuvant radiotherapy, chemotherapy, and autologous stem-cell transplantation.The patient is disease freewith a functional limb on 3 years of follow-up.
Conclusion: ES of scapula is very rare. With meticulous surgery and multidisciplinary treatment approach, limb salvage can be achieved even in such advanced cases, thereby prolonging survival and providing better quality of life.
Keywords: Ewing’s sarcoma, limb salvage, multidisciplinary approach.
Introduction
Ewing’s sarcoma (ES) is a highly malignant small blue round cell tumor of bone and soft tissue, arising from the neuroectodermal cells. It is the second most common primary bone cancer in children and young adults[1]. It was first reported in 1921 by Ewing, as “diffuse endothelioma of bone,” while reporting a round cell sarcoma of the radius in a 14-year-old girl[2]. The tumor is more commonly seen in Caucasians with a male preponderance of 1.5 with majority of the patients in their second decade of life[3]. The tumor mainly affects the long bones (46%) and pelvis (26%) and less commonly skull, vertebra, and short tubular bones of hands and feet[4]. Primary bone tumors of the scapula are more likely to be malignant. ES of the scapula is very rare and very few cases have been reported in the literature[5].
Case Report
A 24-year-old female presented with a massive fungating mass over the left upper back and shoulder. The patient gave a history of swelling over the left upper back, which was insidious in onset and gradually progressed over the past 2 years. Incisional biopsy over the most prominent aspect of the swelling was performed elsewhere about 1 year ago, a provisional diagnosis of ES of the left scapula was made and the patient was started on chemotherapy and operated following 3months of chemotherapy. The wound following surgery did not heal and an ulcer developed over the operated site which rapidly increased in size. Neoadjuvant chemotherapy was started and the regimen was changed multiple times over the next 9months as the tumor did not respond and swelling continued to progress in size. In view of the size and nature of the lesion, wound, and associated complications, the patient was advised forequarter amputation of the left upper limb at multiple centers in her country, which she refused and was finally referred to our hospital for further management. On presentation, a huge fungating mass was noticed over the left upper back and shoulder region with active bleeding and foul-smelling discharge from the ulcer (Fig. 1).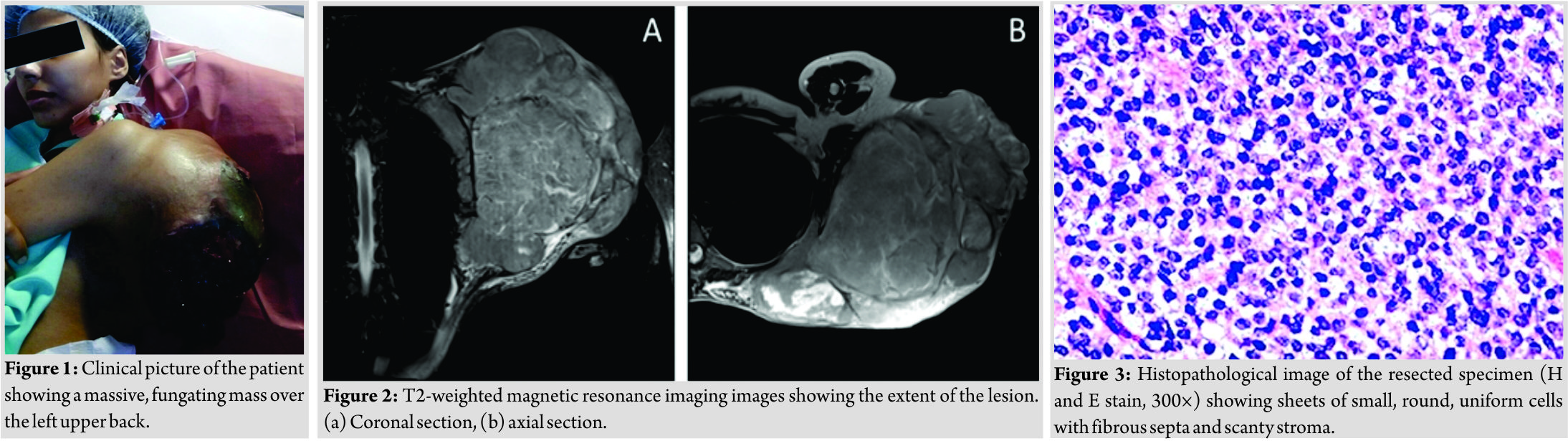 The patient was febrile and unable to use the left upper limb due to the size of the lesion and excruciating pain. Magnetic resonance imaging of the shoulder and upper back showed a T1 isointense and T2 heterogeneous high-signal intensity lesion which measured 18 cm ×27cm × 26cmin size, with multiple fluid levels, degenerative cystic changes, hemorrhage, areas of necrosis, and infiltration of periscapular musculature (Fig. 2). On computed tomography (CT) scan, tumor was ill defined with heterogeneous attenuation, multiple areas of cystic changes, and gross osteolysis of the scapula. However, the shoulder joint, chest wall,and the brachial plexus were not involved, axillary vascular bundle was displaced anteriorly without signs of infiltration. Whole body positron emission tomography-CT scan showed no signs of pulmonary or distant metastasis. Diagnosis of Ewing’s sarcoma was made by histopathological examination of needle biopsy sample from the swelling, which showed sheets of small, round, and uniform cells with scanty cytoplasm, separated by fibrous strands with few mitosis and minimal stroma (Fig. 3). CD99 was positive on immunohisto chemistry. In view of the clinical condition of the patient up front surgery was performed, following antibiotics to control infection, blood transfusions to correct anemia, and selective arterial embolization of feeding vessels. The patient underwent enbloc excision of the tumor mass by total scapulectomy. The ulcer was covered with an adhesive sterile surgical drape; circumferential incision was made around the tumor mass including 3cm of pinchable uninvolved skin. Axillary vascular bundle and the brachial plexus were dissected and isolated from the tumor mass. Arthrotomy of the left shoulder was performed as a layer of the capsule of the joint was also removed. Periscapular musculature was also removed along with the tumor mass. Frozen section from the surrounding soft tissue and chest wall was negative for residual tumor cells. The humeral head was secured to the lateral end of the clavicle (Fig. 4), and the defect over the back following resection was closed by negative pressure dressing and subsequentlycovered2days later with latissimus dorsi free pedicle flap (Fig. 5). The humeral head was plain radiograph of the left shoulder region following resection.Diagnosis of ES was confirmed by histopathological examination of the resected specimen and all the resected surgical margins were free of tumor (Fig. 6). 3 weeks after surgery, concomitant radiotherapy and adjuvant chemotherapy (6 cycles of vincristine, doxorubicin, and cyclophosphamide alternating with ifosfamide and etoposide) were started.The patient also underwent autologous stem cell transplantation following adjuvant chemotherapy. There were no neurological or vascular deficits in the operated limb following the procedure and the patient on follow-up had good functional range of motion of the left shoulder and full range of motion of the left elbow, wrist, and fingers. On final follow-up of 3 years, the patient showed no signs of local recurrence (LR) or metastasis and had returned to her prior vocational status (Fig. 7).
The patient was febrile and unable to use the left upper limb due to the size of the lesion and excruciating pain. Magnetic resonance imaging of the shoulder and upper back showed a T1 isointense and T2 heterogeneous high-signal intensity lesion which measured 18 cm ×27cm × 26cmin size, with multiple fluid levels, degenerative cystic changes, hemorrhage, areas of necrosis, and infiltration of periscapular musculature (Fig. 2). On computed tomography (CT) scan, tumor was ill defined with heterogeneous attenuation, multiple areas of cystic changes, and gross osteolysis of the scapula. However, the shoulder joint, chest wall,and the brachial plexus were not involved, axillary vascular bundle was displaced anteriorly without signs of infiltration. Whole body positron emission tomography-CT scan showed no signs of pulmonary or distant metastasis. Diagnosis of Ewing’s sarcoma was made by histopathological examination of needle biopsy sample from the swelling, which showed sheets of small, round, and uniform cells with scanty cytoplasm, separated by fibrous strands with few mitosis and minimal stroma (Fig. 3). CD99 was positive on immunohisto chemistry. In view of the clinical condition of the patient up front surgery was performed, following antibiotics to control infection, blood transfusions to correct anemia, and selective arterial embolization of feeding vessels. The patient underwent enbloc excision of the tumor mass by total scapulectomy. The ulcer was covered with an adhesive sterile surgical drape; circumferential incision was made around the tumor mass including 3cm of pinchable uninvolved skin. Axillary vascular bundle and the brachial plexus were dissected and isolated from the tumor mass. Arthrotomy of the left shoulder was performed as a layer of the capsule of the joint was also removed. Periscapular musculature was also removed along with the tumor mass. Frozen section from the surrounding soft tissue and chest wall was negative for residual tumor cells. The humeral head was secured to the lateral end of the clavicle (Fig. 4), and the defect over the back following resection was closed by negative pressure dressing and subsequentlycovered2days later with latissimus dorsi free pedicle flap (Fig. 5). The humeral head was plain radiograph of the left shoulder region following resection.Diagnosis of ES was confirmed by histopathological examination of the resected specimen and all the resected surgical margins were free of tumor (Fig. 6). 3 weeks after surgery, concomitant radiotherapy and adjuvant chemotherapy (6 cycles of vincristine, doxorubicin, and cyclophosphamide alternating with ifosfamide and etoposide) were started.The patient also underwent autologous stem cell transplantation following adjuvant chemotherapy. There were no neurological or vascular deficits in the operated limb following the procedure and the patient on follow-up had good functional range of motion of the left shoulder and full range of motion of the left elbow, wrist, and fingers. On final follow-up of 3 years, the patient showed no signs of local recurrence (LR) or metastasis and had returned to her prior vocational status (Fig. 7).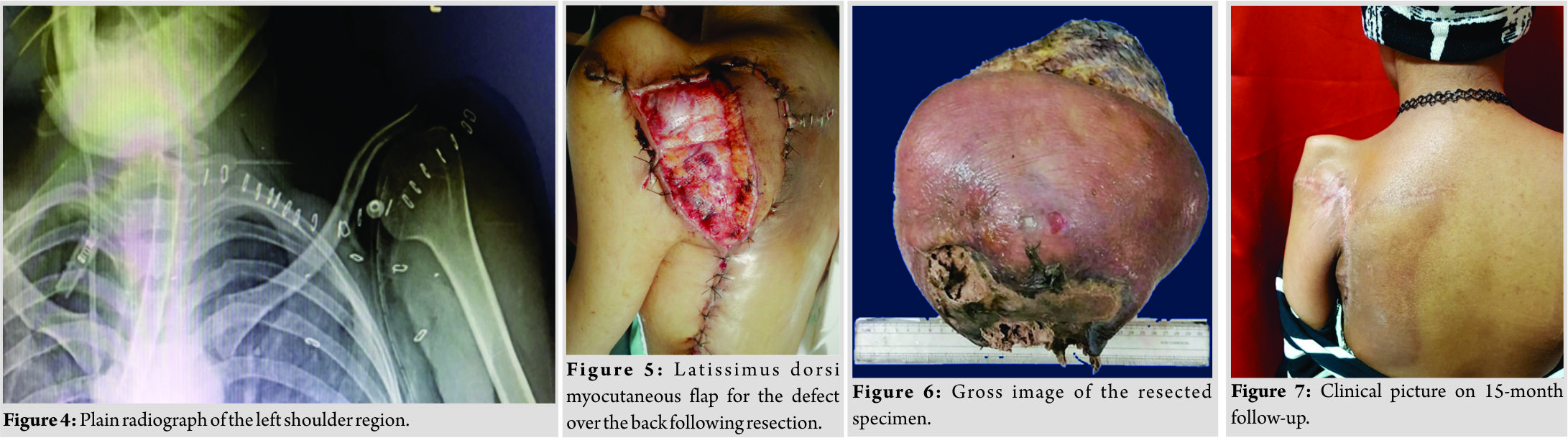
Discussion
Surgery for malignant bone and soft tissue tumors around the shoulder is technically demanding due to the anatomical challenges unlike the extremities. The decision to salvage a limb depends on the location of the tumor, status of the neurovascular structures, involvement of the functional group of muscles around the tumor, and also the ability to restore movements following reconstruction of the salvaged limb [6, 7]. Although Malawar et al. provided a comprehensive surgical classification for limb salvage procedures around the shoulder girdle, it does not include large and aggressive tumors with soft tissue extension beyond the shoulder abductor mechanism and the data available regarding management of such locally advanced tumors around the shoulder are limited [8, 9]. The primary goal for any surgery in musculoskeletal oncology is local tumor control as the old dictum “life over limb” and under no circumstances, a suboptimal tumor resection should be considered at the cost of preserving the limb or its function. With formidable advancement in imaging and surgical techniques in the recent times, forequarter amputation is not commonly performed and is reserved for selective cases with advanced, large, multifocal, or recurrent tumors [10]. Lesensky et al. presented an approach on surgical management of patients with locally advanced sarcomas of the shoulder girdle and emphasized on the need for individualized treatment strategy [11]. Decision for limb salvage over amputation is multifactorial and should include the nature and extent of the tumor, patient characteristics, and the ability to preserve the vascularity, innervation, and function of the limb to be preserved. The possible complication of limb salvage should also be anticipated and the final decision of surgery should be taken only after through counseling of the patient. The role of adjuvant chemotherapy following surgery for ES even in adults has been well established to significantly prolong the relapse-free survival as well as overall survival [12, 13]. High doses of chemotherapeutic agents, particularly alkylating agents, cause dose-limiting myelosuppression, which can be circumvented by simulating hematopoietic recovery by autologous marrow transplantation [14]. Myeloablative chemotherapy and hematopoietic stemcell transplantation are widely used as part of intensive treatment protocol for ES, especially in advanced cases [15, 16]. Tenneti et al., in their review of treatment protocol for relapsed ES, reported an increased 5-year event-free survival and overall survival in patients treated with high-dose chemotherapy followed by autologous stem cell transplantation over conventional chemotherapy [17]. There is,hence,a definite role of autologous stem cell transplantation and adjuvant radiotherapy following surgery for ES, especially in patients with massive tumors, where wide margins resection may not be achievable in all planes. Albergo et al. reported that the LRof ES was significantly reduced (P=0.044) with adjuvant radiotherapy in patients with marginal resection and the 5-year LR-free survival was 96% [18]. Fraser et al. reported an overall 3-year survival of 54% in children and young adults with ES following autologous stem cell transplantation [19]. In a retrospective review of 388 patients with ES by Albergo et al., 15% developed LR and the mean time period for LR was 27 months following surgery. For patients with LR,age >16years (P=0.001), size of the tumor >80mm (P<0.001), limb salvage surgery (P=0.02), and central location of the tumor (P<0.001) were all reported as poor prognostic factors for overall survival [18]. Since all these characteristics are seen in our patient, although she has been currently LR free for 3 years, long-term follow-up is warranted.
Conclusion
This case was reported as first the incidence of ES of the scapula is rare and second to highlight the attainability and importance of limb salvage surgery even in such massive, fungating, previously operated, and chemoresistant malignant tumors. In advanced tumors, we strongly advocate a multidisciplinary approach and a personalized strategy to accommodate the extension of the tumor, status of the surrounding anatomical structures, and also the patient condition and characteristics to decide the type of surgical resection and reconstruction, without compromising on oncological principles of resection, to provide better outcome and better quality of life.
Clinical Message
While treating advanced bone and soft tissue tumors, a multidisciplinary approach and a personalized treatment strategy are essential. To provide the best quality of life and outcome following surgical resection and reconstruction for such tumors, along with anatomical aspects of the tumor, the patient’s condition and characteristics also have to be considered. Limb salvage can be performed even in such massive tumors without compromising on the oncological principles of surgical resection with meticulous surgical planning and execution.
References
1. Obata H, Ueda T, Kawai A, Ishii T, Ozaki T, Abe S, et al. Clinical outcome of patients with ewing sarcoma family of tumors of bone in Japan: The Japanese musculoskeletal oncology group cooperative study. Cancer 2007;109:767-75.
2. Ewing J. The classic: Diffuse endothelioma of bone. Proceedings of the New York pathological society 1921;12:17. Clin OrthopRelat Res 2006;450:25-7.
3. Bölling T, Hardes J, Dirksen U. Management of bone tumours in paediatric oncology. Clin Oncol (R Coll Radiol) 2013;25:19-26.
4. Werier J, Yao X, Caudrelier JM, Di Primio G, Ghert M, Gupta AA, et al. A systematic review of optimal treatment strategies for localized ewing’s sarcoma of bone after neo-adjuvant chemotherapy. Surg Oncol 2016;25:16-23.
5. Shahid M, Varshney M, Maheshwari V, Mubeen A, Siddiqui MA, Julfiqar J, et al. Ewing’s sarcoma of scapula: A rare entity. BMJ Case Rep 2011;2011:bcr0220113810.
6. Unni KK, Inwards CY. Mayo foundation for medical E, research. In: Dahlin’s Bone Tumors: General Aspects and Data on 10,165 Cases. Philadelphia, PA: Wollters Kluwer Health/Lippincott Williams And Wilkins; 2010.
7. Khan Z, Gerrish AM, Grimer RJ. An epidemiological survey of tumour or tumour like conditions in the scapula and periscapular region. SICOT J 2016;2:34.
8. Wong JC, Abraham JA. Upper extremity considerations for oncologic surgery. Orthop Clin North Am 2014;45:541-64.
9. Malawer M, Wittig J. Overview of resections around the shoulder girdle: Anatomy, surgical considerations and classification. In: Malawer M, Sugarbaker PH, editors. Musculoskeletal Cancer Surgery: Treatment of Sarcomas and Allied Diseases. Dordrecht, Netherlands: Springer; 2001. p. 179-202.
10. Qadir R, Sidhu S, Romine L, Meyer MS, Duncan SF. Interscapulothoracic (forequarter) amputation for malignant tumors involving the upper extremity: Surgical technique and case series. J Shoulder Elbow Surg 2014;23:e127-33.
11. Lesenský J, Mavrogenis AF, Igoumenou VG, Matejovsky Z Jr.,Nemec K, Papagelopoulos PJ, et al. Complex surgery for locally advanced bone and soft tissue sarcomas of the shoulder girdle. Eur J Orthop Surg Traumatol2017;27:777-86.
12. Biermann JS, Chow W, Reed DR, Lucas D, Adkins DR, Agulnik M, et al. NCCN guidelines insights: Bone cancer, version 2.2017. J Natl ComprCancNetw2017;15:155-67.
13. Wagner MJ, Gopalakrishnan V, Ravi V, Livingston JA, Conley AP, Araujo D, et al. Vincristine, ifosfamide, and doxorubicin for initial treatment of ewing sarcoma in adults. Oncologist 2017;22:1271-7.
14. Seeger RC, Reynolds CP. Treatment of high-risk solid tumors of childhood with intensive therapy and autologous bone marrow transplantation. Pediatr Clin North Am 1991;38:393-424.
15. Burdach S, van Kaick B, Laws HJ, Ahrens S, Haase R, Körholz D, et al. Allogeneic and autologous stem-cell transplantation in advanced ewing tumors. An update after long-term follow-up from two centers of the european intergroup study EICESS. Stem-cell transplant programs at düsseldorf university medical center, Germany and st. Anna kinderspital, Vienna, Austria. Ann Oncol 2000;11:1451-62.
16. Atra A, Whelan JS, Calvagna V, Shankar AG, Ashley S, Shepherd V, et al. High-dose busulphan/melphalan with autologous stem cell rescue in ewing’s sarcoma. Bone Marrow Transplant 1997;20:843-6.
17. Tenneti P, Zahid U, Sagar F, Usman M, Anwer F. Role of high-dose chemotherapy and autologous stem cell transplantation for relapsed ewing’s sarcoma: A case report with focused review of literature. Cureus 2018;10:e2581.
18. Albergo JI, Gaston CL, Parry MC, Laitinen MK, Jeys LM, Tillman RM, et al. Risk analysis factors for local recurrence in ewing’s sarcoma: When should adjuvant radiotherapy be administered? Bone Joint J 2018;100-B:247-55.
19. Fraser CJ, Weigel BJ, Perentesis JP, Dusenbery KE, DeFor TE, Baker KS, et al. Autologous stem cell transplantation for high-risk ewing’s sarcoma and other pediatric solid tumors. Bone Marrow Transplant 2006;37:175-81.
 |
 |
 |
 |
 |
| Dr. Pramod Chinder | Dr. Suraj Hindiskere | Dr. Srinath Doddarangappa | Dr. Utkarsh Pal | Dr. Kiran Tej Daggupati |
| How to Cite This Article: Chinder P, Hindiskere S, Doddarangappa S, Pal U, Daggupati K T. Massive Fungating Ewing’s Sarcoma of Scapula Treated by Limb Salvage Surgery: A Case Report. Journal of Orthopaedic Case Reports 2019 Jan-Feb; 9(1): 58-61. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com




