[box type=”bio”] Learning Point of the Article: [/box]
Osteoid oseteoma of cervical spine is a rare entity and CT guided navigation can aid in complete resection of tumor without recurrence.
Case Report | Volume 9 | Issue 1 | JOCR January – February 2019 | Page 78-81| Akshay Gadiya, Kunal Shah, Priyank Patel, Abhay Nene. DOI: 10.13107/jocr.2250-0685.1318
Authors: Akshay Gadiya[1], Kunal Shah[2], Priyank Patel[3], Abhay Nene[1]
[1]Department of Spine, Lilavati Hospital and Research Center, A-79, Bandra Reclamation, Bandra-West, Mumbai, Maharashtra, India,
[2]Department of Spine, Aarav Polyclinic, Ghatkopar, Mumbai, Maharashtra, India,
[3]Department of Spine, Jupiter Hospital, Thane, Maharashtra, India.
Address of Correspondence:
Dr. Akshay Gadiya,
Clinical and Research Fellow, The Spine Clinic, Lilavati Hospital and Research Center, A-79, Bandra Reclamation, Bandra-West, Mumbai – 400050, Maharashtra, India.
E-mail: akshaygadia@gmail.com
Abstract
Introduction: Osteoid osteoma of cervical spine is a rare clinical entity and accounts for 4% of cases of overall spinal osteoid osteoma. It has predilection for neural arch and complete resection is difficult task due to proximity to important neurovascular structures. Incomplete resection leads to recurrence in about 4.5% of patients. Computed tomography (CT)-based navigation may aid in resection of tumor without compromising stability, but whenever it inevitable fusion is mandatory.
Case Report: We report two cases of osteoid osteoma of cervical spine managed with surgical excision. Case1 had recurrence of tumor at the left C6 pedicle after minimally invasive intervention that was later managed by surgical excision with the help of CT-guided navigation. Case 2 had osteoid osteoma of the right C4 lateral mass that was treated with surgical excision and fusion.
Conclusion: Osteoid osteoma is a rare pathology in cervical spine. Surgical excision of cervical osteoid osteoma is a daunting task due to the proximity to neurovascular structures. Recurrence though less often is the result of inadequate excision.
Keywords: Osteoid osteoma, cervical spine, recurrence, surgical excision.
Introduction
Osteoid osteoma, as described by Jaffe, is a benign bone-forming skeletal neoplasm that usually presents in patients younger than 30 years of age[1, 2]. Although it can affect any bone in the body, spine is involved in 10% of cases, with lumbar spine being most common site followed by cervical spine contributing to about 50% of spinal osteoid osteoma[3]. About 4% of osteoid osteoma are localized to cervical spine[4]. In cervical spine, the scenario is more complicated as it is usually located in proximity to vertebral artery, spinal cord, or nerve root, and complete excision is difficult due to limited surgical approach[5]. About 4.5% of tumors have recurrence[6]. We report a series of two patients of osteoid osteoma of cervical spine and highlight the challenges in surgical management.
Statement of informed consent
Both the patients were informed that data concerning their case would be submitted for publication and both the patients have agreed for it.
Case Report
Case 1
A 29-year-old female presented with complaints of neck pain with the left radiculopathy, gradually increasing for 10 months. The patient also complained of disturbed sleep due to pain that was responding to nonsteroidalanti-inflammatory drugs(NSAIDs). There were no signs of myelopathy. There was no sensory or motor deficit. Plain X-ray of cervical spine did not reveal any specific abnormality. Computed tomography (CT) scan of cervical spine patient had 6mm focal and expansileossific lesion on the inferior aspect of the left pedicle of C6 vertebrae along with focal osseous mass extending into the left C6-C7 neural foramen. On magnetic resonance imaging (MRI), in addition to above findings, there was asymmetrical soft tissue that was seen along the posterior aspect of the left vertebral artery that was indenting on the left C7 nerve root. Radionucleotide scan revealed well-defined nidus at the inferior aspect of the left pedicle of C6 vertebra with increased osseous activity. As a part of further investigation, the patient was subjected to CT-guided excisional biopsy. Histopathology, the patient had well-formed nidus of osteoid osteoma with no evidence of malignancy. Following procedure, CT scan shown complete excision of nidus with intact sclerotic rim. Symptoms improved dramatically following procedure; hence, surgical excision was deferred. The patient was asymptomatic for 13 months, but there was gradual increase in the intensity of axial neck pain and left upper limb radiculopathy. There was no neurological weakness. CT scan revealed recurrence of nidus at the left C6 pedicle with increased heterogeneous soft tissue extending into the left C6-C7 vertebral foramen. Bone scan concurred with CT findings and was suggestive of recurrence of osteoid osteoma. MRI had shown the recurrence of tumor with hyperintense and heterogeneous mass compressing the left C7 nerve root. The patient underwent surgical intervention for recurrent osteoid osteoma of the left C6 pedicle. C6 left hemilaminectomy was performed along with complete excision of nidus. Since the tumor was located in the close vicinity of the left vertebral artery, the approach was difficult due to the risk of vertebral artery injury. Tumor was approached cautiously under guidance of CT-based navigation. As it was revision excision of tumor, we could realize the distorted external bony landmark of the pedicle. Hence, using navigation in the present surgery was of paramount importance to ensure complete and precise excision of tumor while avoiding injury to vertebral artery. Since we were able to preserve the left C6-C7 facet joint, fusion was avoided. The patient had complete relief in the left upper limb radiculopathy immediately following surgery. On follow-up CT scan, there was complete excision of tumor. The patient has significant improvement in neck disability index score following surgery. There was no recurrence at 5-year follow-up. Images in [Fig. 1] are illustrative of Case 1.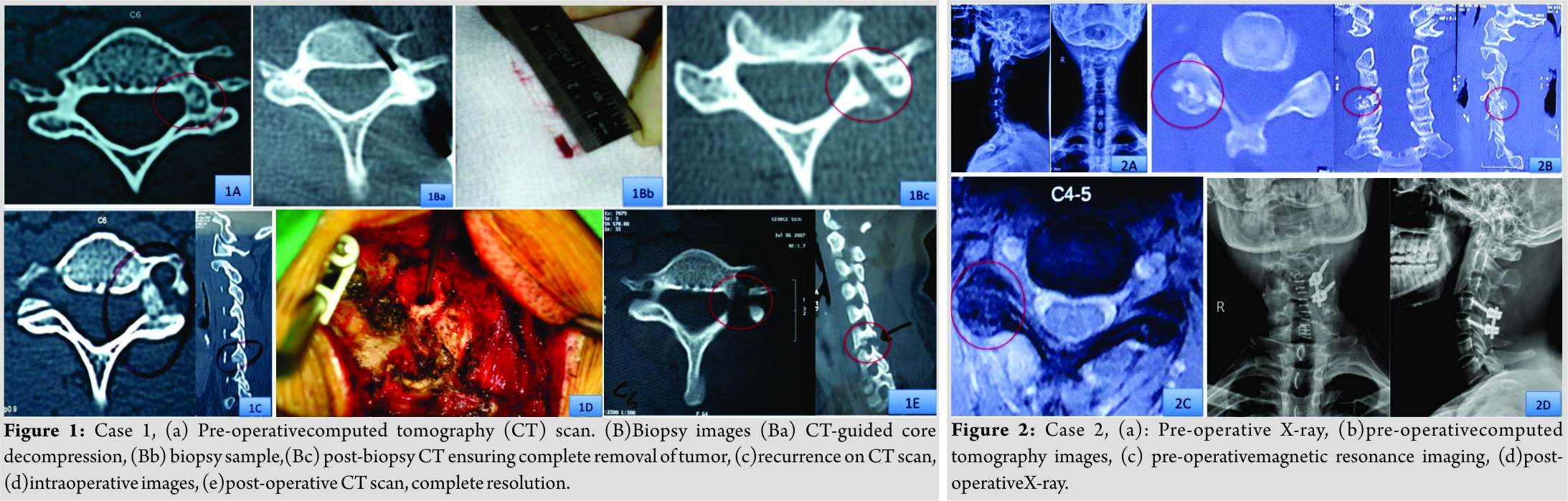
Case 2
A 29-year-old male patient presented with complaints of chronic recalcitrant neck pain and restricted neck movements not relieved with analgesics. Pain was diffuse in nature and was aggravated during night. Pain was radiating to the lateral aspect of the right shoulder. There were no signs of myelopathy or restriction of fine motor activity. On plain X-ray, there was increased radiolucency of the right C4 lateral mass. CT scan revealed a lytic lesion of 12mm × 11mm × 13 mm in size with heterogeneous soft tissue on the posterior aspect of the right facet and lamina of C4 vertebra along with central ossificnidus that was extending into the right C4-C5 neural foramen. Radionucleotide scan revealed well-defined nidus at the inferior aspect of the left pedicle of C6 vertebra with increased osseous activity. MRI demonstrated a heterogeneous mass on the posterior aspect of the right lateral mass of C4 that was extending into C4-C5 neural foramen indenting on the right C5 nerve root. The patient was subjected to surgical excision by posterior approach. The right hemilaminectomy of C4 vertebra was done along with complete excision of tumor and the right C4 facet. Posterior instrumented fusion of C4-C5 segment was done with the help of the left C4-C5 lateral mass fixation. Histopathological examination was suggestive of osteoid osteoma of the right C4 lateral mass. The patient had complete relief of the right upper limb radiculopathy immediately after surgery. There was no recurrence at 5-year follow-up. Images in [Fig. 2] are illustrative of Case 2.
Discussion
Osteoid osteoma is benign skeletal neoplasm and majority of the patient presents with localized neck pain that is continuous and is typically aggravated at night [7, 8]. Sometimes, the patients may also present with torticollis and deformity of neck. This non-structural deformity is speculated because of inflammatory effect of lesion[9, 10]. Neurological deficits are less frequently encountered in osteoid osteoma as compared to osteoblastoma. Frequently, the patients with osteoid osteoma of cervical spine may present with pain radiating to shoulder and arms due to compression of nerve roots. This is often attributed to the frequent localization of tumor near neural foramen. Clinical features often mimic other pathologies; hence, there is often delay in diagnosis of this tumor [9, 10]. Osteoid osteoma is often missed on plain radiographs as symptoms often precede the radiological changes on radiographs [1,6]. Radionucleotide bone scans are more sensitive than conventional radiographs for diagnosing osteoid osteoma. Typically, there is focal uptake of dye in nidus surrounded by reduced uptake due to increased osteoblastic activity in nidus surrounded by sclerotic bone that is often referred to “double density sign” [11]. Both the patients in the present series had this characteristic lesion on radionucleotide scans. Computerized tomography (CT) scan is the most sensitive investigation for diagnosing osteoid osteoma [12]. Lytic lesion having sclerotic rim of bone along with central calcified nidus is typically noted on CT scan. Osteoid osteoma most commonly affects the posterior elements of vertebra [13]. Both the patients in the present series had a characteristic lesion on CT scan. MRI will demonstrate the heterogeneous lesion and is important to know the compression on the nerve root or spinal cord. Nidus is less conspicuous on MRI because the calcification within the nidus is of low-signal intensity on short repetition time and long repetition time images [14]. In contrast, inflammation in adjacent soft tissue and bone marrow is overwhelmingly seen on MRI. In the present series, both the patients had heterogeneous tissue on MRI around the posterior elements that were extending into neural foramen and compressing the respective exiting nerve roots. On histology, there is a central ossificnucleus that is usually surrounded by sclerotic rim. Osteoblastomas are differentiated from osteoid osteoma by the feature that former is more than 15mm in diameter, expansile, and locally aggressive tumors[15]. Both the patients in the present series had these characteristic features of osteoid osteoma on histopathological examination. Osteoid osteoma though benign and is reported to respond to NSAIDs; it is usually resistant to conservative treatment. Various surgical treatments have been described for the management of osteoid osteoma including percutaneous radio frequency coagulation, mini-invasive excision of tumor, and complete surgical resection of tumor [10, 16]. Radio frequency coagulation involves the percutaneous thermal coagulation of neoplastic tissue under the guidance of CT scan under local anesthesia [16]. Although the role of radio frequency coagulation has been described widely in osteoid osteomas of appendicular skeleton, its role in spinal pathologies is scarcely reported. Moreover, due to strategic location of osteoid osteomas in the vicinity of spinal cord and vertebral artery makes coagulation risky [17]. [Table 1] highlights the algorithm followed by authors in their clinical practice. As osteoid osteomas are frequently localized in the vicinity of important neurovascular structure, “mini-invasive” excision of these tumors is usually a daunting task and can lead to injury to the vital structures [10, 18]. Removal of these tumors with minimally invasive approach has often led to recurrences due to incomplete excision. Recurrence rate is reported in about 4.5% of patients [4]. One of the patients in the present case series had CT-guided core decompression that eventually had recurrence. It may be because of incomplete removal of sclerotic rim.
Conclusion
Osteoid osteoma of cervical spine is a rare entity and seldom reported in literature. Surgical excision is bit complicated due to complex native anatomy and proximity to neurovascular structures. Complete excision of nidus along with heterogeneous osseous mass and sclerotic rim is absolutely important to prevent recurrence.
Clinical Message
Complete resection of osteoid osteoma is a difficult task due to proximity of neurovascular structures. Use of CT-based navigation ensures complete resection of tumor without compromising stability and injuring vertebral artery or nerve root and thus preventing fusion.
References
1. Pettine KA, Klassen RA. Osteoid-osteoma and osteoblastoma of the spine. J Bone Joint Surg Am 1986;68:354-61.
2. Jaffe HL. Osteoid osteoma: A benign osteoblastic tumor composed of osteoid and a typical bone. Arch Surg 1935;31:709-28.
3. Raskas DS, Graziano GP, Herzenberg JE,Heidelberger KP, Hensinger RN. Osteoid osteoma and osteoblastoma of the spine. J Spinal Disord 1992;5:204-11.
4. Campanacci M. Bone and Soft Tissue Tumors. Bologna: AuloGaggi; 1990. p. 355-374.
5. Laus M. Zappoli FA, Malaguti MC, Alfonso C. Surgery of Primary Bone Tumors Close to the Vertebral Artery. Burgenstock Estate, Switzerland: XIII Meeting Cervical Spine Research Society, European Section; 1997. p. 31.
6. Jackson RP, Reckling FW, Mants FA. Osteoid osteoma and osteoblastoma. Similar histologic lesions with different natural histories. ClinOrthop 1977;128:303-13.
7. Bruneau M, Cornelius JF, George B. Osteoid osteomas and osteoblasomas of the occipitocervical junction. Spine 2005;30:E567-71.
8. Myles ST, MacRae ME. Benign osteoblastoma of the spine in childhood. J Neurosurg 1988;68:884-8.
9. Zileli M, Cagli S, Basdemir G, Ersahin Y. Osteoid osteomas and osteoblastomas of the spine. Neurosurg Focus 2003;15:E5.
10. Ozaki T, Liljeqvist U, Hillmann A, Halm H, Lindner N, Gosheger G, et al. Osteoid osteoma and osteoblastoma of the spine: Experience with 22 patients. ClinOrthopRel Res 2002;357:394-402.
11. IIelms CA. Osteoid osteoma, the double density sign. ClinOrthop 1987;222:167-73.
12. Gamba JL, Martinez S, Apple J, Harrelson JM, Nunley JA. Computed tomography of axial skeletal osteoid osteomas. AJR Am J Roentgenol 1984;142:769-72.
13. Marcove RC, Heelan RT, Huvos AG, Healey J, Lindeque BG. Osteoid osteoma: Diagnosis, localization and treatment. ClinOrthopRelat Res 1991;267:197-201.
14. Glass RB, Poznanski AK, Fisher MR, Shkolnik A, Dias L. MR imaging of osteoid osteoma. J Comput Assist Tomogr 1986;10:1065-7.
15. Kchouk M, Mrabet A, Touibi S, Douik M, Siala M, Slimen N. Osteoid osteoma of the spine. Radiological study of 21 cases. J Radiol 1993;74:135-42.
16. Pinto CH, Taminiau AH, Vanderschueren GM, Hogendoorn PC, Bloen JL, Obermann WR. Technical consideration in CT-guided radiofrequency thermal ablation of osteoid osteoma: Tricks of the trade. AJR Am J Roentgenol 2002;1633:1642.
17. Laus M, Albisinni U, Alfonso C, Zappoli FA. Osteoid osteomas of the cervical spine: Surgical treatment or percutaneous radiofrequency coagulation? Eur Spine J 2007;16:2078-82.
18. The Cervical Spine Research Society. The Cervical Spine. 3rded. New York: Lippincott; 1998. p. 634-5.
 |
 |
 |
 |
| Dr. Akshay Gadiya | Dr. Kunal Shah | Dr. Priyank Patel | Dr. Abhay Nene |
| How to Cite This Article: Gadiya A, Shah K, Patel P, Nene A. Osteoid Osteoma of Cervical Spine: A Case Report and Review of Literature. Journal of Orthopaedic Case Reports 2019 Jan-Feb; 9(1): 78-81. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com




