[box type=”bio”] Learning Point of the Article: [/box]
Injury to the popliteal neurovascular structures is a rare but potentially catastrophic complication following closing wedge high tibial osteotomies, and its prompt recognition and treatment are of paramount importance for a good long-term outcome.
Case Report | Volume 9 | Issue 2 | JOCR March – April 2019 | Page 38-41 | Ricardo Santos-Pereira, Catarina Aleixo, Marco Bernardes, André Costa, Joaquim Fontes-Lebre, Paulo Jorge Carvalho. DOI: 10.13107/jocr.2250-0685.1360
Authors: Ricardo Santos-Pereira[1], Catarina Aleixo[1], Marco Bernardes[1], André Costa[1], Joaquim Fontes-Lebre[1], Paulo Jorge Carvalho[1]
[1]Department of Orthopedics, Centro Hospitalar Vila Nova de Gai /Espinho, Vila Nova de Gaia, Portugal.
Address of Correspondence:
Dr. Ricardo Santos-Pereira,
Department of Orthopedics, Centro Hospitalar Vila Nova de Gai/Espinho, Vila Nova de Gaia, Portugal.
E-mail: ricardo.s.pereira@gmail.com
Abstract
Introduction: High tibial osteotomy (HTO) is an adequate procedure for the treatment of medial unicompartmental knee arthritis in the varus knee. It is technically demanding and has a significant complication rate. Although rare, vascular injury is potentially the most serious complication.
Case Report: We present the case of a 50-year-old male who developed a popliteal artery pseudoaneurysm needing surgical intervention following closing wedge (CWHTO). The patient presented with worsening pain and progressive neurological symptoms. The osteotomy healed normally but the neurological symptoms showed only minor improvement over the 2-year follow-up period.
Conclusions: Even with proper surgical technique, CWHTO presents a small inherent risk of injury to the popliteal neurovascular structures. Prompt recognition and treatment of this injury are of paramount importance for a good long-term outcome. Further studies are necessary to determine if open wedge HTO would be a safer surgical option.
Keywords: Popliteal artery, Pseudoaneurysm, High tibial osteotomy, Knee.
Introduction
High tibial osteotomy (HTO) was previously one of the most popular procedures for treating unicompartmental knee osteoarthritis, especially in varus-aligned knees. The purpose of the surgery is to change the mechanical axis of the lower limb to unload the damaged medial compartment [1]. It is a technically demanding procedure with a significant complication rate and has gradually declined over time owing to the success of knee arthroplasty surgery. For a long time, the classical lateral valgus closing-wedge HTO (CWHTO) technique has been the preferred method but since the introduction of new implants that provide better fixation interest has resurged in the procedure and the medial valgus opening-wedge HTO (OWHTO) technique has become the most common technique [2]. The current controversy exists about the choice of technique but both CWHTO and OWHTO remain viable options in the treatment of isolated symptomatic medial compartment arthritis, especially in the young active patient. Even though its incidence is very low with very few reported cases in the literature, injury to the popliteal neurovascular bundle is considered to be the most severe complication associated an osteotomy [3]. We report a case of a vascular injury to the popliteal artery resulting in secondary neurological injury after CWHTO.
Case Report
A 50-year-old male patient with no known medical comorbidities underwent CWHTO for isolated medial compartment osteoarthritis of the left knee. He had the same surgery performed on the right knee 3 years prior with excellent clinical outcome (Fig. 1). The patient was positioned supine on the operating table, and a thigh tourniquet was applied. Knee arthroscopy with partial medial meniscectomy was performed. Next, a slightly curved skin incision was made starting posteriorly at the lateral joint line and directed distally midway between the tibia and fibula. The fascia was incised, and the tibialis anterior muscle was detached and elevated off the proximal tibia and retracted laterally, exposing the proximal tibiofibular joint which was disrupted using 1 cm-wide osteotome. The periosteum over the proximal tibia was elevated, and a blunt retractor was inserted posteriorly around the bone. Under fluoroscopic control, the proximal bone cut was made 1.5 cm distal and parallel to the joint line above the tibial tubercle using an oscillating saw and broad osteotomes. The distal bone cut angled toward the first one was made similarly, removing a 10-mm bone wedge edge while preserving an intact medial cortical hinge. Valgus stress was applied to the knee to close the osteotomy, and stable fixation was achieved with a 4.5 mm basic fragment L-plate (Fig. 2a and b). 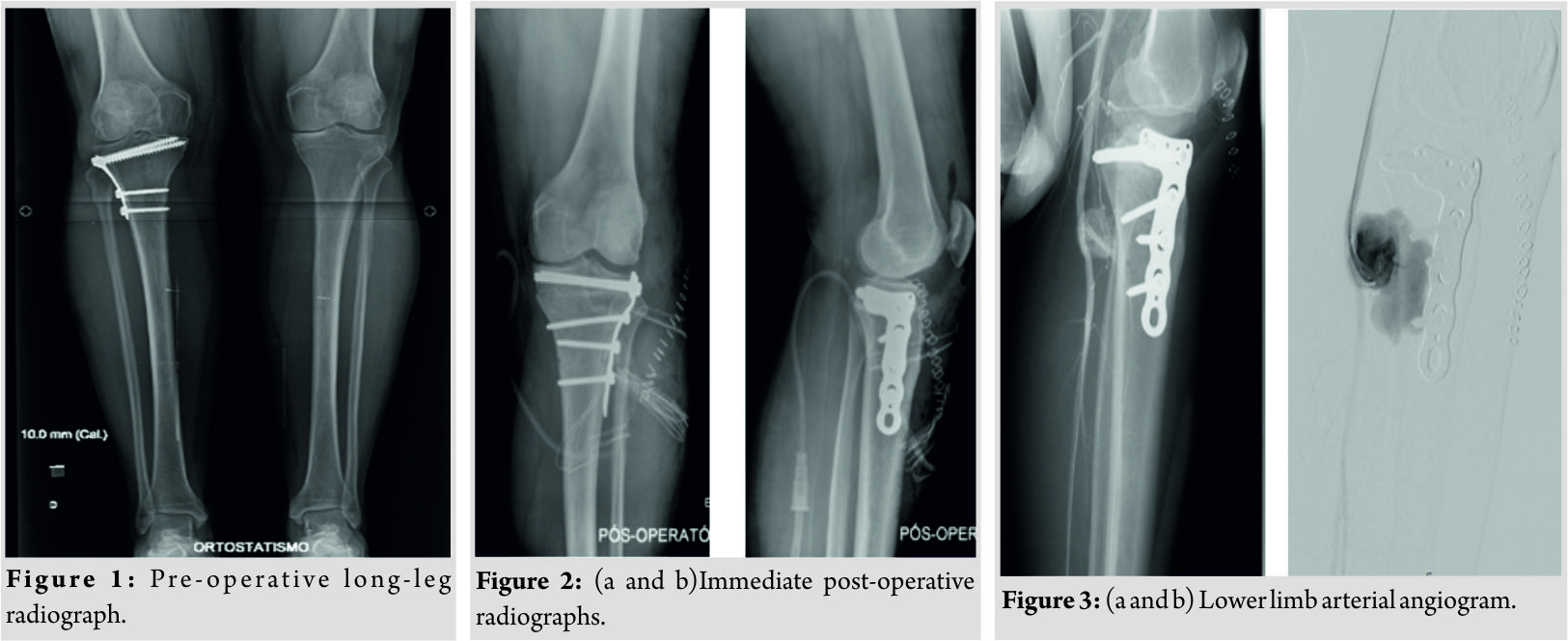 A suction drain was used but the tourniquet was not released before wound closure, as that was not standard practice in our institution. On the 1st post-operative day, the patient presented with an active ankle dorsiflexion deficit but maintained active toe flexion and extension and showed no neurologic deficits. The capillary refill time was <2 s, and he had palpable distal pulses. The suction drain had collected 650 cc of hematic fluid. He was diagnosed with partial common peroneal nerve palsy, and a Boxia-type ankle-footorthosis (AFO) was applied. On the 7th post-operative day, the patient complained of increasing pain and edema in is leg and de novo active toe extension deficit. Distal pulses remained palpable. Imaging studies revealed a pseudoaneurysm of the infra-articular popliteal artery just before the emergence of the anterior tibial artery at the osteotomy site (Fig. 3a, b and 4).
A suction drain was used but the tourniquet was not released before wound closure, as that was not standard practice in our institution. On the 1st post-operative day, the patient presented with an active ankle dorsiflexion deficit but maintained active toe flexion and extension and showed no neurologic deficits. The capillary refill time was <2 s, and he had palpable distal pulses. The suction drain had collected 650 cc of hematic fluid. He was diagnosed with partial common peroneal nerve palsy, and a Boxia-type ankle-footorthosis (AFO) was applied. On the 7th post-operative day, the patient complained of increasing pain and edema in is leg and de novo active toe extension deficit. Distal pulses remained palpable. Imaging studies revealed a pseudoaneurysm of the infra-articular popliteal artery just before the emergence of the anterior tibial artery at the osteotomy site (Fig. 3a, b and 4). 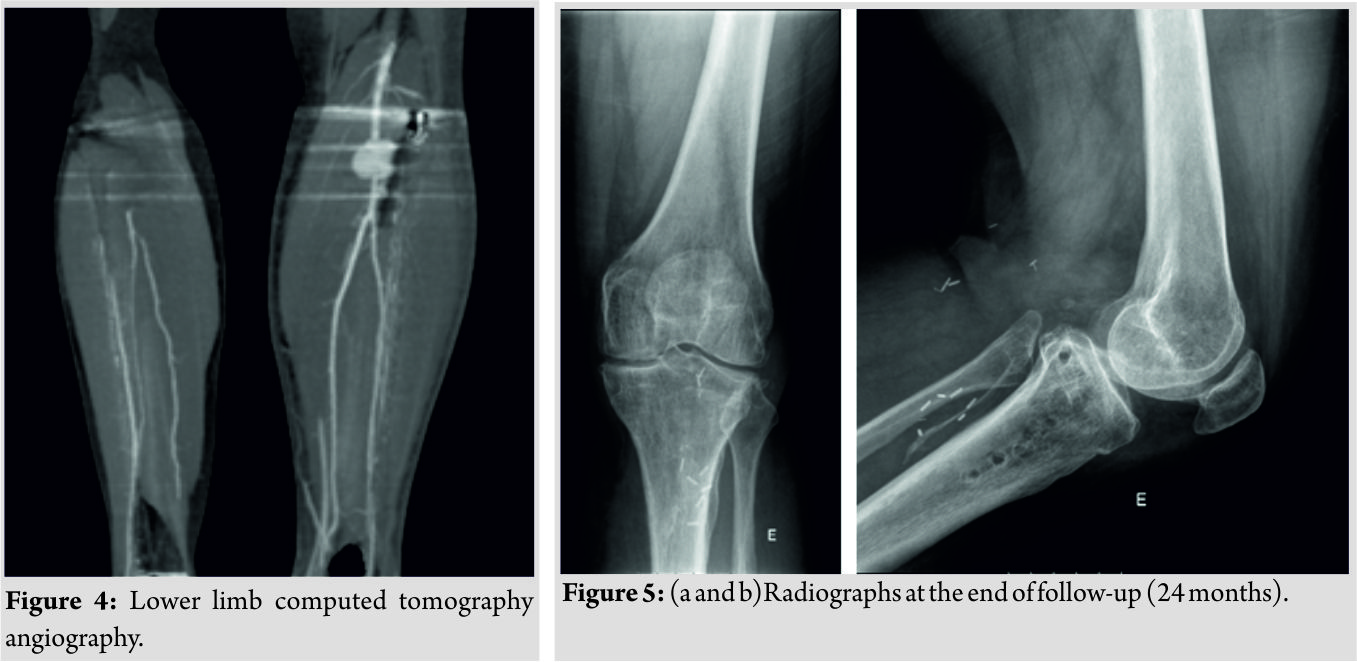 The pseudoaneurysm was subsequently excised and the vessel repaired using an interposed saphenous vein graft between the infra-articular popliteal artery and the tibioperoneal trunk. The anterior tibial artery was deemed irreparable and had to be ligated. Fasciotomy of the anterior leg compartment was performed at the same operative time. There was no observable section of the tibial or proximal common peroneal nerves. Six weeks after the previous vascular surgery, the patient had surgery again to correct another pseudoaneurysm that had developed in the infra-articular popliteal artery, 3 mm proximal to the anastomosis. It was excised with no need for further revascularization procedures. This surgery was complicated by wound dehiscence and infection by methicillin-sensitive Staphylococcus aureus with the need for intravenous antibiotics and two further surgical debridements in the following months. Nevertheless, the osteotomy healed uneventfully and the infection resolved after removal of the osteosynthesis plate 4,5 months after index surgery (Fig. 5a and b). Basal electromyography performed 3 months after the index procedure revealed a complete lesion of the common peroneal nerve with a total denervation pattern. Serial electromyographic evaluations revealed severe compression neuropathy of the common peroneal nerve but showed neurophysiological signs of reinnervation, with the active voluntary activity of all the muscles (severe axonotmesis). At final follow-up (24 months),however, the patient maintained the foot drop with the need of an AFO for ambulation and chronic diffuse lower leg pain. The knee showed satisfactory function with no inflammatory signs and 0–120° range of motion. Erythrocyte sedimentation rate and serum C-reactive protein level were within normal values. The ankle–brachial index was 1.00 on the right, and 0.89 on the left and distalpulses were present.
The pseudoaneurysm was subsequently excised and the vessel repaired using an interposed saphenous vein graft between the infra-articular popliteal artery and the tibioperoneal trunk. The anterior tibial artery was deemed irreparable and had to be ligated. Fasciotomy of the anterior leg compartment was performed at the same operative time. There was no observable section of the tibial or proximal common peroneal nerves. Six weeks after the previous vascular surgery, the patient had surgery again to correct another pseudoaneurysm that had developed in the infra-articular popliteal artery, 3 mm proximal to the anastomosis. It was excised with no need for further revascularization procedures. This surgery was complicated by wound dehiscence and infection by methicillin-sensitive Staphylococcus aureus with the need for intravenous antibiotics and two further surgical debridements in the following months. Nevertheless, the osteotomy healed uneventfully and the infection resolved after removal of the osteosynthesis plate 4,5 months after index surgery (Fig. 5a and b). Basal electromyography performed 3 months after the index procedure revealed a complete lesion of the common peroneal nerve with a total denervation pattern. Serial electromyographic evaluations revealed severe compression neuropathy of the common peroneal nerve but showed neurophysiological signs of reinnervation, with the active voluntary activity of all the muscles (severe axonotmesis). At final follow-up (24 months),however, the patient maintained the foot drop with the need of an AFO for ambulation and chronic diffuse lower leg pain. The knee showed satisfactory function with no inflammatory signs and 0–120° range of motion. Erythrocyte sedimentation rate and serum C-reactive protein level were within normal values. The ankle–brachial index was 1.00 on the right, and 0.89 on the left and distalpulses were present.
Discussion
A HTO is a surgical option for patients with isolated medial compartment osteoarthritis and varus knee alignment. For the traditional CWHTO, the complication rate ranges from 5.6% to 34% [4], with the most frequent complications being a nonunion, hardware failure and inadequate or loss of correction [3]. The most frequent neurovascular complication in CWHTO is peroneal nerve palsy, with the incidence of up to 20% in the literature [4]. This complication is significantly reduced in OWHTO since this procedure avoids interference with the peroneal nerve, proximal tibiofibular joint and the anterior leg compartment [5]. Its other advantages include easier surgical technique and more predictable angular correction. Like many other surgeons, we have since gradually shifted our surgical practice toward OWHTO. Vascular complications are rare but may initially present acutely or insidiously with neurological deficit, as they can induce lower limb compartment syndrome, which may, in turn, induce neural lesions [6]. The surgeon should be aware of this association, and vascular injury should be suspected when there is excessive drainage postoperatively, and the patient develops edema and distal neurovascular symptoms [5]. False aneurysms of the popliteal artery and the inferior lateral geniculate artery have been reported as complications of HTO [7, 8]. Femoral arteriogram or computed tomography angiogram helps in confirming the diagnosis. Surgical intervention is mandatory in these cases [5]. In our case, the vascular injury was only suspected when neurological symptoms resulting from nerve compression by the pseudoaneurysm worsened 1 week after surgery. We hypothesize that this delay in diagnosis may have been at least partially responsible for the incomplete neurological recovery at final follow-up. Furthermore, releasing the tourniquet to check hemostasis before wound closure might have revealed severe active bleeding form deosteotomy site, raising earlier suspicion for vascular injury. This has since become standard practice at our institution. Vascular injury is most likely due to the use of oscillating saw or osteotome when performing the tibial bone cuts [9]. To lessen the risk, the osteotomy should be performed with caution, with the knee in 90° of flexion and with a protective retractor placed in direct contact with the posterior tibial cortex. Strictly following these recommendations in our case, was still insufficient to avoid vascular injury. In fact, in an anatomical study, the major blood vessels around the knee were found to be at risk of injury during OWHTO or CWHTO despite adequate surgical technique [10]. As it only necessitates one bone cut, OWHTO might theoretically pose less risk to the vascular structures comparing to CWHTO, but to this date, there are no studies directly comparing the rates of vascular injury between the two types of procedures. Infection is also a frequent complication following HTO with a reported rate of superficial infection of 1–9% and deep infection of 0.5% and 4.7% [11]. In our case, the two vascular surgeries needed after HTO may have contributed to increased infection risk. Nevertheless, with proper management, infection did not seem to adversely affect the final outcome.
Conclusion
CWHTO is a time-proven procedure in the treatment of medial compartment osteoarthritis but with a significant complication rate and a small but inherent risk to the popliteal neurovascular structures. This risk can be decreased through detailed preoperative planning, judicious technique, and precautions during surgery, and careful postoperative monitoring. Awareness of this potentially catastrophic complication should always be present as its prompt management is imperative for satisfactory outcomes. Further studies are needed to evaluate if OWHTO might be a better surgical option for decreasing the frequency of neurovascular injuries.
Clinical Message
With this paper, the authors present a rare case of popliteal neurovascular injury following CWHTO for the treatment of medial compartment knee osteoarthritis. Surgical tips to minimize the incidence of this complication are discussed as well as its diagnostic evaluation and treatment.
References
1. Coventry MB. Osteotomy of the upper portion of the tibia for degenerative arthritis of the knee. A preliminary report. J Bone Joint Surg Am 1965;47:984-90.
2. Attinger MC, Behrend H, Jost B. Complete rupture of the popliteal artery complicating high tibial osteotomy. J Orthop2014;11:192-6.
3. Vena G, D’Adamio S, Amendola A. Complications of osteotomies about the knee. Sports Med Arthrosc Rev 2013;21:113-20.
4. Tunggal JA, Higgins GA, Waddell JP. Complications of closing wedge high tibial osteotomy. Int Orthop2010;34:255-61.
5. Chae DJ, Shetty GM, Wang KH, Montalban AS Jr., Kim JI, Nha KW, et al. Early complications of medial opening wedge high tibial osteotomy using autologous tricortical iliac bone graft and T-plate fixation. Knee 2011;18:278-84.
6. Georgoulis AD, Makris CA, Papageorgiou CD, Moebius UG, Xenakis T, Soucacos PN, et al. Nerve and vessel injuries during high tibial osteotomy combined with distal fibular osteotomy: A clinically relevant anatomic study. Knee Surg Sports TraumatolArthrosc1999;7:15-9.
7. Rubens F, Wellington JL, Bouchard AG. Popliteal artery injury after tibial osteotomy: Report of two cases. Can J Surg 1990;33:294-7.
8. Tandon SC, Kharbanda Y, Fraser AM. Aneurysm complicating high tibial osteotomy: A case report. Acta OrthopScand1996;67:73-4.
9. Darnis A, Villa V, Debette C, Lustig S, Servien E, Neyret P, et al. Vascular injuries during closing-wedge high tibial osteotomy: A cadaveric angiographic study. OrthopTraumatol Surg Res 2014;100:891-4.
10. Bisicchia S, Rosso F, Pizzimenti MA, Rungprai C, Goetz JE, Amendola A, et al. Injury risk to extraosseous knee vasculature during osteotomies: A cadaveric study with CT and dissection analysis. Clin OrthopRelat Res 2015;473:1030-9.
11. Anagnostakos K, Mosser P, Kohn D. Infections after high tibial osteotomy. Knee Surg Sports TraumatolArthrosc2013;21:161-9.
 |
 |
 |
 |
 |
| Dr. Ricardo Santos-Pereira | Dr. Catarina Aleixo | Dr. Marco Bernardes | Dr. Joaquim Fontes-Lebre | Dr. Paulo Jorge Carvalho |
| How to Cite This Article: Santos-Pereira R, Aleixo C, Bernardes M, Costa A, Fontes-Lebre J, Carvalho PJ. Popliteal Artery Pseudoaneurysm after Closing Wedge High Tibial Osteotomy. Journal of Orthopaedic Case Reports 2019 Mar-Apr; 9(2): 38-41. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com




