[box type=”bio”] Learning Point of the Article: [/box]
A multidimensional assessment should be made when planning the treatment of large defects at the head of the humeral head after recurrent or chronic shoulder dislocations and other treatment options should be kept in mind before the arthroplasty.
Case Report | Volume 9 | Issue 2 | JOCR March – April 2019 | Page 76-79 | Murat Gurger. DOI: 10.13107/jocr.2250-0685.1380
Authors: Murat Gurger[1]
[1]Department of Orthopedics and Traumatology, Faculty of Medicine, Firat University, Elazig, Turkey.
Address of Correspondence:
Dr. Murat Gurger,
Department of Orthopedics and Traumatology,Faculty of Medicine, Firat University, Elazig, Turkey.
E-mail: muratgurger@hotmail.com
Abstract
Introduction: This report highlights chronic locked posterior shoulder dislocation, which is of special interest because the patient who had a reverse Hill–Sachs and Hill–Sachs lesion, with >50% joint surface defects was treated with a shoulder-preserving surgery.
Case Report: A 42-year-old man presented to our clinic with complaints of pain and limited movement in his left shoulder. The patient’s complaints began after he experienced a fall 7 months ago. The patient was believed to have experienced posterior shoulder dislocation, and the clinical diagnosis was confirmed by radiological imaging. Computed tomography revealed a reverse Hill–Sachs lesion on the humeral head and on approximately 25% of the joint surface. During the McLaughlin procedure, because the osteoporotic humerus showed a collapse of approximately 30% on the posterior articular surface, an iatrogenic Hill–Sachs lesion was added to the reverse Hill–Sachs lesion at the beginning of the humeral head. The subscapularis tendon was transferred to the anterior defective area of the humeral head with three anchor sutures. Fixation was performed with a Kirschner wire, while the joint was in the reduction position. At the 62-month follow-up, constant shoulder score was calculated as 84. The patient was pleased with his results and was able to continue his routine activities.
Conclusion: Arthroplasty is the recommended treatment for patients manifesting >50% defect on the humeral head joint surface. However, when these defects are evaluated, factors such as their localization, size, depth, and orientations with respect to the glenoid should be considered. Only after this multifaceted evaluation, appropriate surgical interventions can be planned.
Keywords: Posterior shoulder dislocation, Severe joint surface loss, Preserving surgery.
Introduction
Posterior shoulder dislocation, a rare clinical condition, accounts for <2% of all glenohumeral dislocations and bilateral dislocation is observed in 15% of all cases [1, 2]. Approximately 50%–79% of patients with posterior shoulder dislocation also show chronic dislocation because this condition is usually undetectable and overlooked during initial application [2]. Reportedly, the average time from dislocation to diagnosis is 8 months [1]. The McLaughlin method is one of the recommended treatment methods when the defect on the humeral head (reverse Hill–Sachs lesion) is 20%–45% [3]. Arthroplasty is recommended in case with>50% loss of joint surface [1]. In this study, we have presented a case with a reverse Hill–Sachs and Hill–Sachs lesion, with >50% joint surface defects.
Case Report
A 42-year-old man presented to our clinic with complaints of pain and limited movement in his left shoulder. The patient’s complaints began after he experienced a fall 7 months ago. At that time, radiography of his shoulder revealed soft tissue trauma, which was treated. However, his complaints showed no improvement, and he visited another hospital 3 days later. After radiography, the patient was administered a sling and analgesic, following soft tissue trauma diagnosis. The patient applied to our clinic approximately 7 months after the initial trauma. Subsequently, his left shoulder was fixed in internal rotation, but his passive shoulder movements were extremely limited and painful. Notably, the patient’s neurovascular examination was normal. Therefore, the patient was believed to have experienced posterior shoulder dislocation, and the clinical diagnosis was confirmed by radiological imaging (Fig. 1). Computed tomography (CT) revealed a reverse Hill–Sachs lesion on the humeral head and on approximately 25% of the joint surface. In addition, no associated fractures were noted. The patient was scheduled for the McLaughlin surgical procedure. Open reduction was performed through a deltopectoral approach. When the posteriorly locked humeral head was difficult to reduce, a small Darrach retractor was used. However, during this procedure, because the osteoporotic humerus showed a collapse of approximately 30% on the posterior articular surface, an iatrogenic Hill–Sachs lesion was added to the reverse Hill–Sachs lesion at the beginning of the humeral head (Fig. 2). 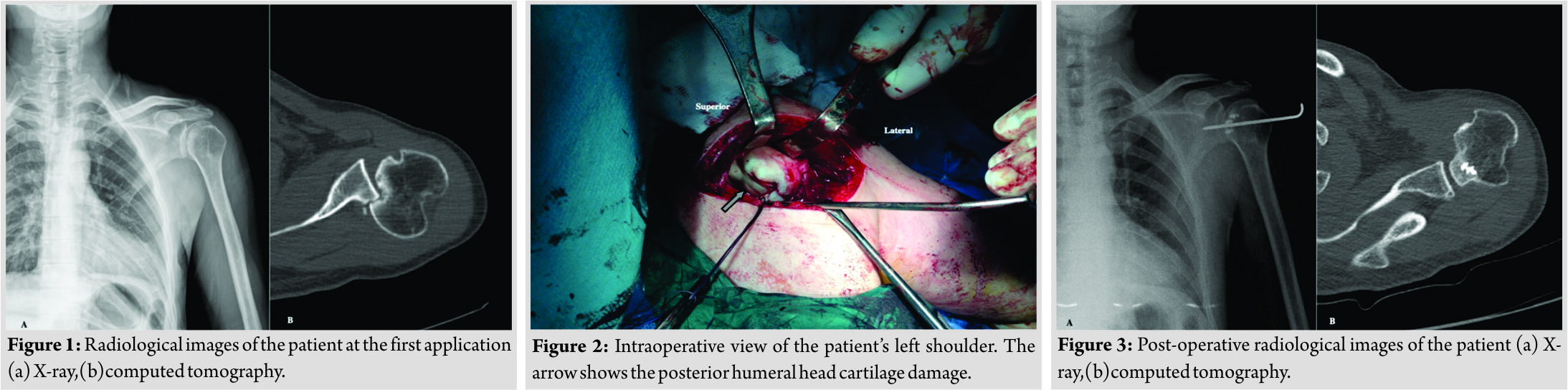 When the glenoid was examined intraoperatively, there was minimal cartilaginous damage on the anterior and posterior glenoid rim cartilage. The patient was intraoperatively reevaluated, and previously, planned surgical procedure was performed. The subscapular is tendon was transferred to the anterior defective area of the humeral head with three anchor sutures, and stability was tested with shoulder movements. In external rotation and abduction, the shoulder was found to be anteriorly subluxed. Although the defect in the posterior humeral head covered approximately 30% of the joint surface, the lesion was not deep; this defect was type 2 according to Calandra et al. [4] classification system. No anterior glenoid rim defect was noted. Considering the possibility that this partial engaging lesion could develop into a non-engaging lesion, fixation was performed with a Kirschner wire, while the joint was in the reduction position (Fig. 3). The patient was administered a sling, and his left shoulder was immobilized for 4 weeks. 1-month post-operation, the wire was removed, and the shoulder movement was initiated under the guidance of a physiotherapist. At the 62-month follow-up, CT images were transformed into three-dimensional format, and the defective joint surface area was calculated using the Image J program (Version 1.51s, NIH, USA). The measurements revealed a defective area of approximately 25% in the anterior part of the humeral head and 30% in the posterior part (Fig. 4). At the final follow-up, the patient reported no pain and active shoulder movements (flexion: 150°, extension: 20°, abduction: 120°, internal rotation: 60°, and external rotation 60°) (Fig. 5). Constant shoulder score was calculated as 84. The patient was pleased with his results and was able to continue his routine activities.
When the glenoid was examined intraoperatively, there was minimal cartilaginous damage on the anterior and posterior glenoid rim cartilage. The patient was intraoperatively reevaluated, and previously, planned surgical procedure was performed. The subscapular is tendon was transferred to the anterior defective area of the humeral head with three anchor sutures, and stability was tested with shoulder movements. In external rotation and abduction, the shoulder was found to be anteriorly subluxed. Although the defect in the posterior humeral head covered approximately 30% of the joint surface, the lesion was not deep; this defect was type 2 according to Calandra et al. [4] classification system. No anterior glenoid rim defect was noted. Considering the possibility that this partial engaging lesion could develop into a non-engaging lesion, fixation was performed with a Kirschner wire, while the joint was in the reduction position (Fig. 3). The patient was administered a sling, and his left shoulder was immobilized for 4 weeks. 1-month post-operation, the wire was removed, and the shoulder movement was initiated under the guidance of a physiotherapist. At the 62-month follow-up, CT images were transformed into three-dimensional format, and the defective joint surface area was calculated using the Image J program (Version 1.51s, NIH, USA). The measurements revealed a defective area of approximately 25% in the anterior part of the humeral head and 30% in the posterior part (Fig. 4). At the final follow-up, the patient reported no pain and active shoulder movements (flexion: 150°, extension: 20°, abduction: 120°, internal rotation: 60°, and external rotation 60°) (Fig. 5). Constant shoulder score was calculated as 84. The patient was pleased with his results and was able to continue his routine activities.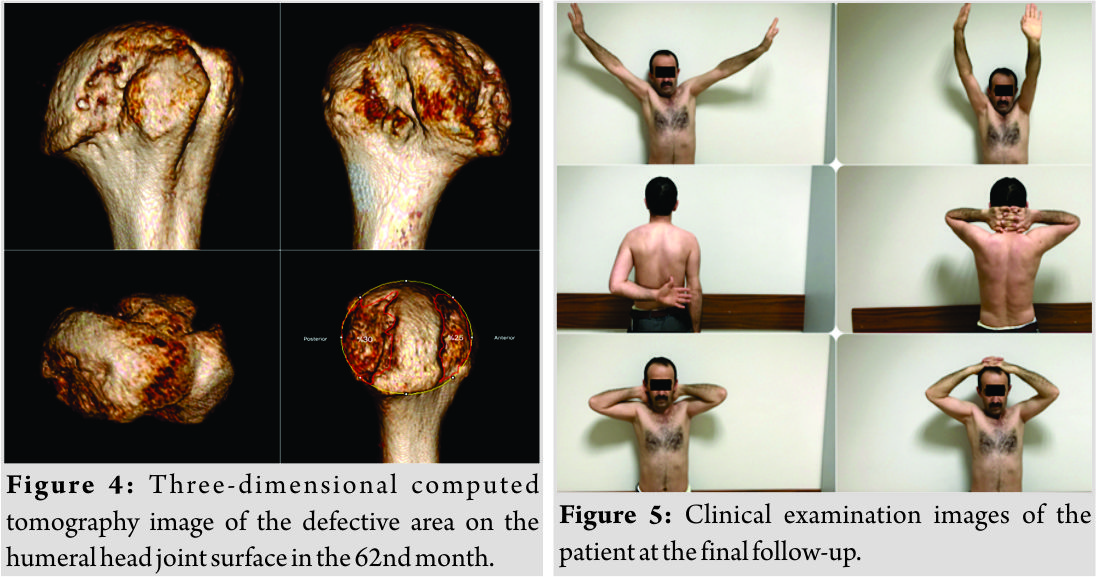
Discussion
Due to the difficulties in diagnosing posterior shoulder dislocation, McLaughlin referred to this injury as a diagnostic trap [5]. Once diagnosed, the treatment strategy depends on the size of the defect in the humeral head and the duration of the dislocation. If the impaction fracture covers <25% of the humeral head joint surface and the dislocation occurred<3 weeks ago, the patient can be treated with closed reduction and immobilization in the external rotation position; however, the success rate of closed reduction is low in chronic dislocations. Arthroplasty is the recommended treatment for defects involving >50% of the joint surface [6]. McLaughlin [5]was the first to describe the technique of transposing the subscapularis tendon to the reverse Hill–Sachs lesion in patients with posterior shoulder dislocation. Since then, this technique has been modified by other authors. For instance, Hawkins et al. [7] fixed the lesser tuberosity with the attached subscapularis tendon in the defective area. Charalambous et al. [8] defined tendon plication in the defective area with the suture anchors without detaching the subscapularis tendon from lesser tuberosity. However, for this injury, anatomical reconstruction of the humeral head with autogenous bone graft or allograft or rotational osteotomies is the other treatment modalities [6]. In our case, although the McLaughlin surgical method was scheduled, a Hill–Sachs-like lesion occurred during the reduction of the posteriorly locked humeral head. After the development of this complication, a defect of >50% was noted on the joint surface. The classic Hill–Sachs lesion is the compression fracture generated in the posterolateral portion of the humeral head by the anterior margin of the glenoid during anterior shoulder dislocation [9]. When a treatment is scheduled, the shape, size, depth, and location of the Hill–Sachs lesion should be considered [9]. This lesion can be observed in 67%–93% of the cases with anterior shoulder dislocation, although not every lesion is symptomatic (1.5%–34%) [10]. Although the general conclusion is that the Hill–Sachs lesion is clinically significant, covering >25% of the joint surface, less massive Hill–Sachs lesions may be symptomatic in cases of concomitant glenoid defects [10]. In the present case, this Hill–Sachs-like lesion covered approximately 30% of the joint surface, but it was not very deep. However, the orientation of the lesion on the humeral head was partially diagonal as compared with the glenoid anterior margin. On considering all these observations, the surgical treatment, i.e., the McLaughlin method was planned for the patient. Burkhart and De Beer were the first to describe the engaging and non-engaging Hill–Sachs lesion concept [11]. In the engaging Hill–Sachs lesion, the orientation of the defect at the humeral head is parallel to the anterior margin of the glenoid, leading to the attachment of the humeral head to the glenoid. On the other hand, in the non-engaging Hill–Sachs lesion, the defect on the humeral head is diagonal to the anterior edge of the glenoid, creating a contact between the humeral head and the glenoid articular surface [11]. Engagement is directly related to the “glenoid track concept,” as described by Yamamoto et al. [12]. This concept defines the joint surface as a humeral head contact on the glenoid during abduction and external rotation movement [13]. A lesion expressed off-track is indicative of engaging lesion. However, the on-track lesion defines a non-engaging lesion [10]. In our case, the glenoid track was evaluated after the anterior defect of the humeral head was treated by the McLaughlin method and the posterior defect was considered to be partially engaging, hence the glenohumeral joint was fixed with a Kirschner wire (3-mm length) in the neutral position and held in place for 4 weeks.
Conclusion
Arthroplasty is the recommended treatment for patients manifesting >50% defect on the humeral head joint surface. However, when these defects are evaluated, factors such as their localization, size, depth, and orientations with respect to the glenoid should be considered. Only after this multifaceted evaluation, appropriate surgical interventions can be planned.
Clinical Message
In the neglected posterior shoulder dislocations, humeral head defects detected by pre-operative imaging methods may increase during intraoperative interventions. Therefore, this should be kept in mind during pre-operative planning.
References
1. Castagna A, Delle Rose G, Borroni M, Markopoulos N, Conti M, Maradei L, et al. Modified macLaughlin procedure in the treatment of neglected posterior dislocation of the shoulder. Chir Organi Mov 2009;93 Suppl 1:S1-5.
2. Singh S, Tan CK, Sinopidis C, Frostick S, Brownson P. Missed posterior dislocation of the shoulder after intramedullary fixation of humeral fractures: A report of three cases. J Shoulder Elbow Surg 2009;18:e33-7.
3. Konda SR, Fisher N, Gage M, Egol KA. Posterior fracture dislocation of the shoulder: A Modified mcLaughlin procedure. J Orthop Trauma 2017;31 Suppl 3:S36-S37.
4. Calandra JJ, Baker CL, Uribe J. The incidence of hill-sachs lesions in initial anterior shoulder dislocations. Arthroscopy 1989;5:254-7.
5. McLaughlin HL. Posterior dislocation of the shoulder. J Bone Joint Surg Am 1952;24 A:584-90.
6. Kokkalis ZT, Mavrogenis AF, Ballas EG, Papanastasiou J, Papagelopoulos PJ. Modified mcLaughlin technique for neglected locked posterior dislocation of the shoulder. Orthopedics 2013;36:e912-6.
7. Hawkins RJ, Neer CS 2nd, Pianta RM, Mendoza FX. Locked posterior dislocation of the shoulder. J Bone Joint Surg Am 1987;69:9-18.
8. Charalambous CP, Gullett TK, Ravenscroft MJ. A modification of the mcLaughlin procedure for persistent posterior shoulder instability: Technical note. Arch Orthop Trauma Surg 2009;129:753-5.
9. Morsy MG. Arthroscopic remplissage: Is it still an option? EFORT Open Rev 2017;2:478-83.
10. Fox JA, Sanchez A, Zajac TJ, Provencher MT. Understanding the hill-sachs lesion in its role in patients with recurrent anterior shoulder instability. Curr Rev Musculoskelet Med 2017;10:469-79.
11. Burkhart SS, De Beer JF. Traumatic glenohumeral bone defects and their relationship to failure of arthroscopic bankart repairs: Significance of the inverted-pear glenoid and the humeral engaging hill-sachs lesion. Arthroscopy 2000;16:677-94.
12. Yamamoto N, Itoi E, Abe H, Minagawa H, Seki N, Shimada Y, et al. Contact between the glenoid and the humeral head in abduction, external rotation, and horizontal extension: A new concept of glenoid track. J Shoulder Elbow Surg 2007;16:649-56.
13. Di Giacomo G, Itoi E, Burkhart SS. Evolving concept of bipolar bone loss and the hill-sachs lesion: From “engaging/non-engaging” lesion to “on-track/off-track” lesion. Arthroscopy 2014;30:90-8.
 |
| Dr. Murat Gurger |
| How to Cite This Article: Gurger M. Shoulder Preserving Surgery in Case of Defect of more than half of the Joint Surface: A Case Report. Journal of Orthopaedic Case Reports 2019 Mar-Apr;9(2): 76-79. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com




