[box type=”bio”] Learning Point of the Article: [/box]
Intramedullary nailing is a minimally invasive prophylactic and definitive treatment method of AFFs with less morbidity and hospital stay. High index of suspicion helps in identifying incomplete AFFs and prevents further morbidity of a complete fracture by prophylactic intramedullary nailing.
Case Report | Volume 9 | Issue 3 | JOCR May-June 2019 | Page 61-64 | Vivek Sodhai, Chetan Pradhan, Ashok Shyam. DOI: 10.13107/jocr.2250-0685.1422
Authors: Vivek Sodhai[1], Chetan Pradhan[1], Ashok Shyam[1], [2]
[1]Orthopaedic Surgeon, Department of Trauma, Sancheti Institute for Orthopaedics & Rehabilitation, Pune, Maharashtra. India .
[2]Department of Orthopaedics, Indian Orthopaedic Research Group, Thane, Maharashtra, India.
Abstract
Introduction: Atypical femoral fractures(AFF) are rare. To get more knowledge, these cases are being reported at an increasing rate in recent literature. Surgical treatment in these fractures is controversial.
Case Report: A 73-year-old lady, known rheumatoid and osteoporotic with a history of long-term bisphosphonate intake, presented with sudden onset right thigh pain after trivial trauma. We diagnosed a complete atypical femoral fracture, treated with closed intramedullary nailing. 4 months later, she presented with dull aching left thigh pain for 2 weeks. Radiographic features suggested an incomplete atypical femoral fracture, treated with prophylactic insitu intramedullary nailing. At 1 year follow-up, lady was walking well with stick support.
Conclusion: Our case highlights two important points. Intramedullary nailing is a minimally invasive treatment option for incomplete and complete AFF. We should have a high index of suspicion in diagnosing and recognizing warning signs of incomplete fractures such as prodromal thigh pain and isolated focal lateral cortical thickening, thereby preventing further progression and treatment with prophylactic nailing at an early stage.
Keywords: Atypical femoral fracture, Bisphosphonate, Prophylactic nailing.
Introduction
Atypical femoral fractures (AFF) are being reported at an increasing rate in recent literature. Etiology of these fractures is not well understood, but it has been reported to occur in patients who have been on a prolonged course of bisphosphonate administration for osteoporosis [1, 2] and excessive femoral bowing [3, 4]. The diagnosis follows major and minor criteria, which were originally described by the Task Force of the American Society for Bone and Mineral Research in 2010 and updated in 2013 [1]. The features of AFFs are location mainly in the subtrochanteric region and diaphysis; the lack of trauma history and comminution; and a transverse or short oblique configuration (Table 1). Furthermore, the definition discriminates complete fractures with typical medial spikes from incomplete fractures involving only the lateral cortex, correlating with the site of the highest biomechanical stress. Minor features include radiological signs such as periosteal reaction and increased cortical thickness, prodromal symptoms, bilateral occurrence, and delayed healing. Various surgical treatment options have been described for incomplete and complete AFFs. Intramedullary fixation is the preferred method in most cases [5, 6, 7], while plate fixation is useful in cases of excessive femoral bowing[8] and revision surgeries. We report a case of bilateral AFFs who was on prolonged bisphosphonate treatment, successfully treated with intramedullary nailing. This case highlights intramedullary nailing as a minimally invasive method of treatment of these fractures leading to earlier mobilization and reducing the hospital stay. This case also highlights the importance of identification of prodromal symptoms such as thigh pain and distinct radiological features of incomplete AFF of the contralateral femur.
Case Report
A 73-year-old lady with no history of previous trauma presented to our trauma center with a history of sudden onset pain over the right thigh after a jerk while getting up from a chair. The patient gave the history of seropositive rheumatoid arthritis and osteoporosis with compression fractures of vertebrae for which she was on disease-modulating antirheumatoid drugs and bisphosphonate (Anti-resorptive) medications. The patient also received a dose of denosumab 60 mg subcutaneously 2 weeks before the incident. On admission, the radiographic examination of right femur showed complete fracture at the diaphyseal level of transverse/short oblique configuration without comminution with a medial spike and concomitant hypertrophic lateral cortex (Fig. 1a, b, c). Radiograph of the spine showed multiple osteoporotic vertebral fractures with severe kyphosis (Fig. 2). 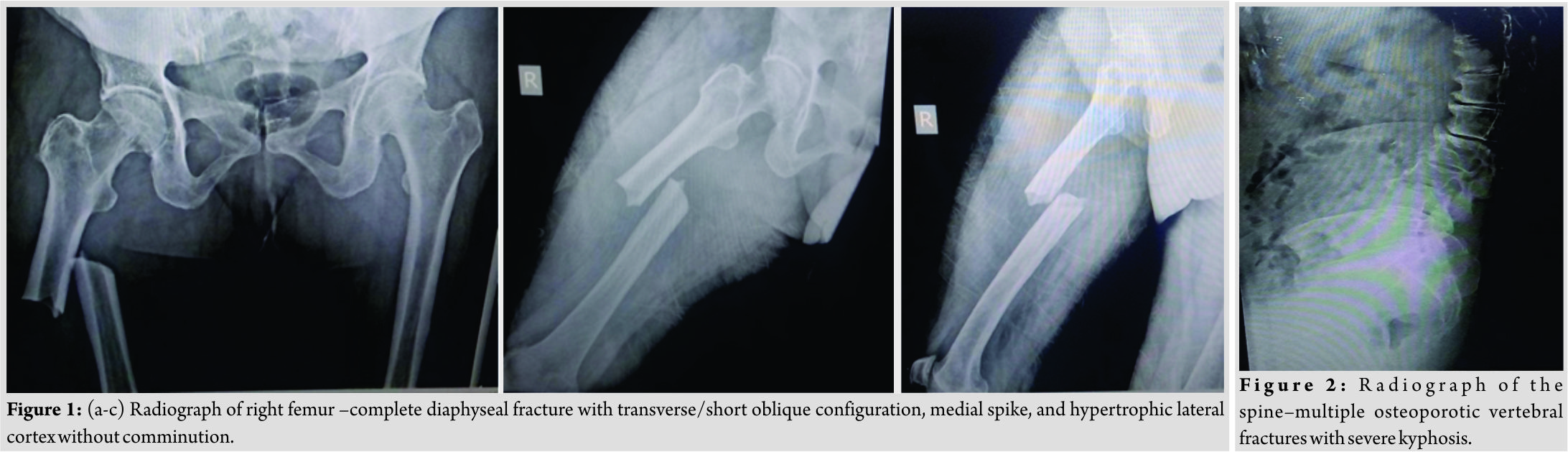 On further inquiry, the patient gave the history of pre-existing dull aching pain over the right thigh. All these features, radiographic as well as prodromal symptoms lead to a diagnosis of atypical femoral fracture as per criteria mentioned in [Table 1]. Patient’s blood count analysis and metabolic profile were within normal limits. Considering, AFF have been reported to occur commonly in subtrochanteric and diaphyseal region of the femur [1], the patient was treated with closed intramedullary nailing (Fig. 3a, b) and antiresorptive medications were stopped. Intraoperative and post-operative recovery was uneventful, and she was mobilized non-weight bearing with walker successfully and discharged on post-operative day 2. At 6 weeks, radiograph showed good callus formation (Fig. 4a, b), she was started on weight-bearing walking. The lady was walking well until 4 months later she presented to our outpatient department with dull aching pain over left thigh. The pain increased while walking and getting up from sitting position. Radiograph of contralateral left femur revealed endosteal reaction and focal area of lateral cortex hypertrophy at the isthmic region (Fig. 5a,b).
On further inquiry, the patient gave the history of pre-existing dull aching pain over the right thigh. All these features, radiographic as well as prodromal symptoms lead to a diagnosis of atypical femoral fracture as per criteria mentioned in [Table 1]. Patient’s blood count analysis and metabolic profile were within normal limits. Considering, AFF have been reported to occur commonly in subtrochanteric and diaphyseal region of the femur [1], the patient was treated with closed intramedullary nailing (Fig. 3a, b) and antiresorptive medications were stopped. Intraoperative and post-operative recovery was uneventful, and she was mobilized non-weight bearing with walker successfully and discharged on post-operative day 2. At 6 weeks, radiograph showed good callus formation (Fig. 4a, b), she was started on weight-bearing walking. The lady was walking well until 4 months later she presented to our outpatient department with dull aching pain over left thigh. The pain increased while walking and getting up from sitting position. Radiograph of contralateral left femur revealed endosteal reaction and focal area of lateral cortex hypertrophy at the isthmic region (Fig. 5a,b).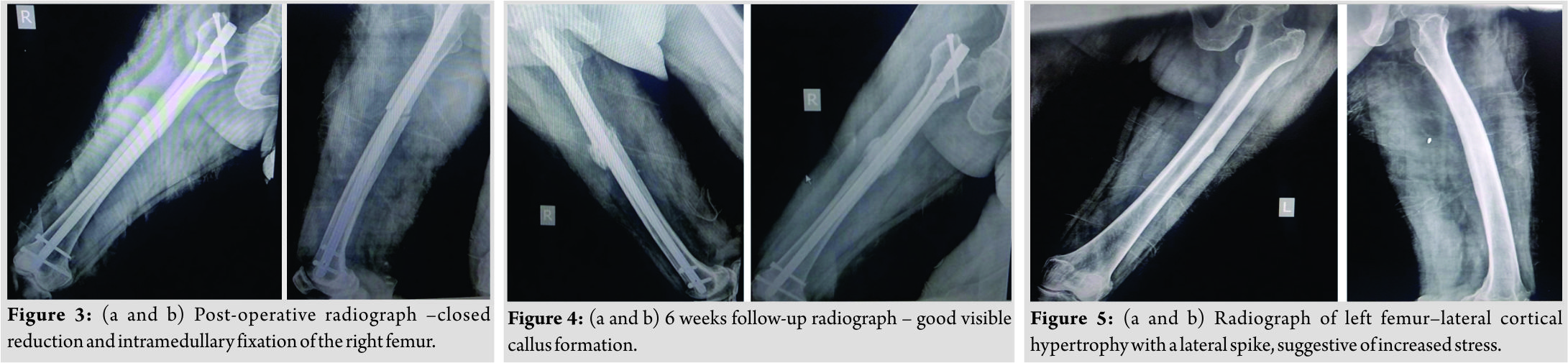 As per scoring system given by Min et al, the fracture on the left side is scored as – Site– 2(diaphyseal); pain– 2(Mild); contralateral– 1(Complete); radiolucent line– 1(Focal change),and the total score – 6 [9]. She was admitted and treated with prophylactic insitu intramedullary nailing (Fig. 6). Post-operative period was uneventful and she was mobilized full weight bearing with stick support successfully and discharged on post-operative day 1. At 6 weeks follow-up, the patient was relieved of the left-sided thigh pain and radiograph showed signs of healing (Fig. 7a, b). Right-sided complete AFF had healed well as seen in 1 year follow-up radiograph (Fig. 8a, b) and patient walks with stick support.
As per scoring system given by Min et al, the fracture on the left side is scored as – Site– 2(diaphyseal); pain– 2(Mild); contralateral– 1(Complete); radiolucent line– 1(Focal change),and the total score – 6 [9]. She was admitted and treated with prophylactic insitu intramedullary nailing (Fig. 6). Post-operative period was uneventful and she was mobilized full weight bearing with stick support successfully and discharged on post-operative day 1. At 6 weeks follow-up, the patient was relieved of the left-sided thigh pain and radiograph showed signs of healing (Fig. 7a, b). Right-sided complete AFF had healed well as seen in 1 year follow-up radiograph (Fig. 8a, b) and patient walks with stick support.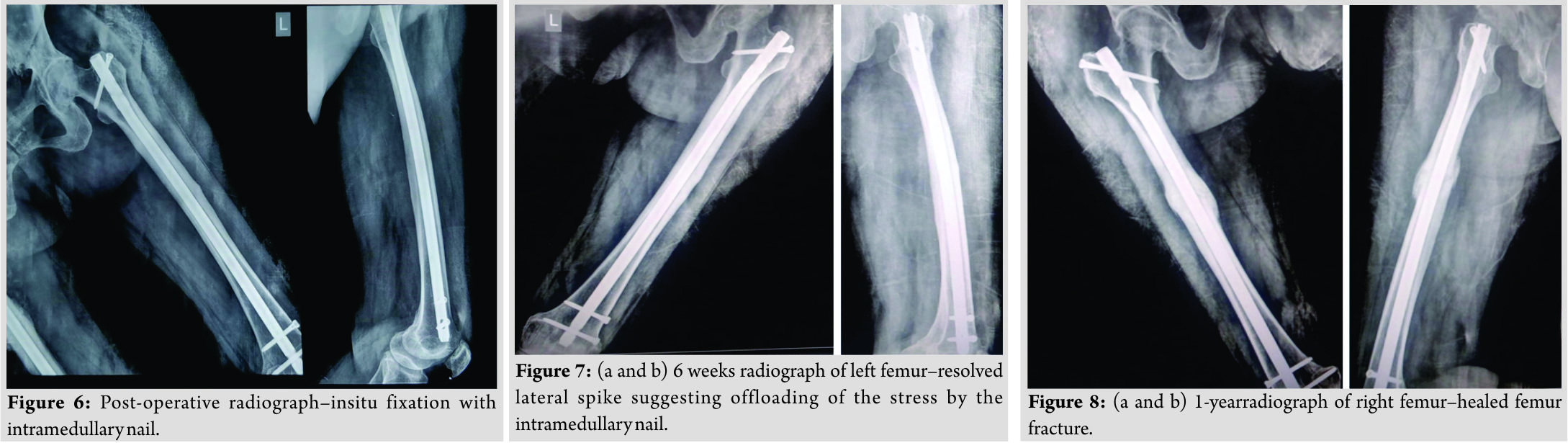
Discussion
Patients receiving bisphosphonate medications for osteoporosis are at 0.006–1.1% risk of developing AFFs [1, 10]. A longer duration of bisphosphonate use is considered a risk factor for AFFs [1, 2, 11]. Cases with duration of <2 years have an approximate AFF incidence of 2 in 100,000, while cases with a duration of 8 or more years have an approximate AFF incidence of 78 in 100,000 [11].Various treatment methods have been described for complete AFFs. While most of the studies suggest intramedullary nailing as the preferred method of these fractures [5, 6, 7], few studies have reported the use of surface fixation in cases of AFFs with excessive femoral bowing [8]. Egol et al. reported delayed and reliable healing after bisphosphonate-associated complete femur fractures treated with intramedullary nailing [10]. Certain studies recommend protection of the whole femur including the femoral neck [12]; however, a recent study on prophylactic nailing of femoral neck conducted by Shieh et al. says: Prophylactic fixation of femoral neck using reconstruction nail with two screws along the femoral neck did not restore the strength of the proximal femur to pre-fracture levels. The study also says that there was no significant difference with an implant with two reconstruction screw compared to an intramedullary nail with a transverse proximal interlocking screw [13]. 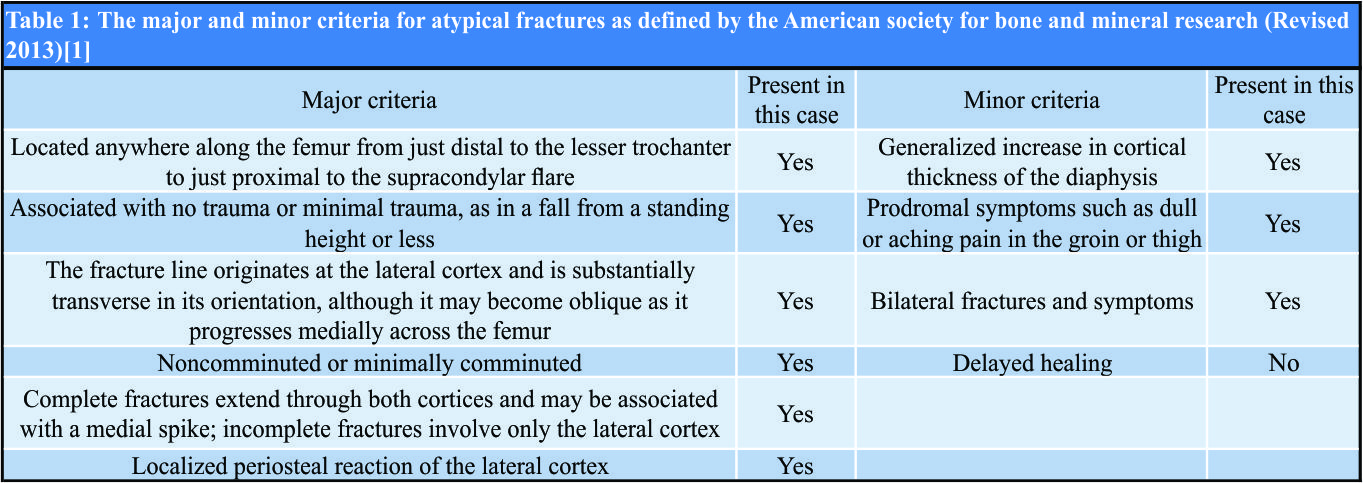 Few studies report activity modification like restricted weight bearing on the affected limb as an option, but it seems to be unreliable because the majority of these incomplete fractures progress to fracture completion [14, 15]. Capeci and Tejwani reported good outcomes in AFFs with prefracture lesions [16]. Ohet al. recommended prophylactic fixation of incomplete AFF with healing in all cases [6]. Patients who present with these fractures, usually present with prodromal thigh pain weeks or months before the development of complete AFF. Radiograph before an established complete fracture usually shows focal lateral cortical hypertrophy with or without a visible fracture line [17, 18].
Few studies report activity modification like restricted weight bearing on the affected limb as an option, but it seems to be unreliable because the majority of these incomplete fractures progress to fracture completion [14, 15]. Capeci and Tejwani reported good outcomes in AFFs with prefracture lesions [16]. Ohet al. recommended prophylactic fixation of incomplete AFF with healing in all cases [6]. Patients who present with these fractures, usually present with prodromal thigh pain weeks or months before the development of complete AFF. Radiograph before an established complete fracture usually shows focal lateral cortical hypertrophy with or without a visible fracture line [17, 18].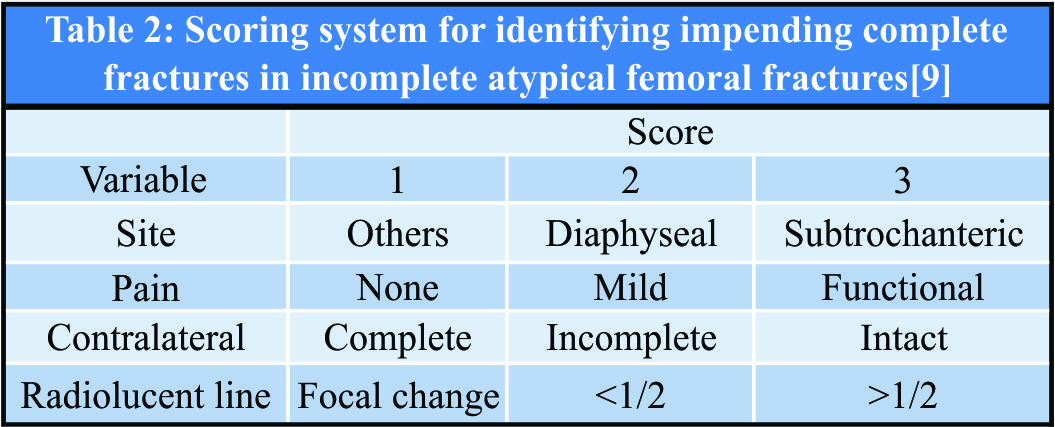
Conclusion
Our case shows highlight two important points while managing AFF. First, the case shows that intramedullary nailing can be recommended as the minimally invasive closed method treatment for prophylactic as well as definitive treatment of incomplete and complete AFF. Fractures heal well without any complications. It has less morbidity as compared to open reduction and surface plating and also reduces the hospital stay. However, surface plating can be used in extended indications such as excessive femoral bowing and revision surgeries of these cases. Second, managing these fractures requires a high index of suspicion in identifying the prodromal symptoms of thigh pain and radiological features of isolated lateral cortical thickening. These are the warning signs of incomplete AFFs and intervening at this time will prevent the fracture progression to complete AFF. In situ intramedullary nailing can be done in these cases.
Clinical Message
Intramedullary nailing as a minimally invasive prophylactic and definitive treatment method of AFFs with less morbidity and hospital stay. A high index of suspicion in treating these fractures helps in identifying incomplete AFFs and prevents further morbidity by prophylactic intramedullary nailing.
References
1. Shane E, Burr D, Abrahamsen B, Adler RA, Brown TD, Cheung AM, et al. Atypical subtrochanteric and diaphyseal femoral fractures: Second report of a task force of the American society for bone and mineral research. J Bone Miner Res 2014;29:1-23.
2. Neviaser A, Lane J, Lenart B, Edobor-Osula F, Lorich D. Low-energy femoral shaft fractures associated with alendronate use. J Orthop Trauma 2008;22:346-50.
3. Kim JW, Kim JJ, Byun YS, Shon OJ, Oh HK, Park KC, et al. Factors affecting fracture location in atypical femoral fractures: A cross sectional study with 147 patients. Injury 2017;48:1570-4.
4. Yoo H, Cho Y, Park Y, Ha S. Lateral femoral bowing and the location of atypical femoral fractures. Hip Pelvis 2017;29:127-32.
5. Egol K, Park J, Prensky C, Rosenberg Z, Peck V, Tejwani N. Surgical treatment improves clinical and functional outcomes for patients who sustain incomplete bisphosphonate related femur fractures. J Orthop Trauma 2013;6:331-5.
6. Oh C, Oh J, Park K, Kim J, Yoon Y. Prophylactic nailing of incomplete atypical femoral fractures. Sci World J 2013;2013:450148.
7. Ward W, Carter C, Wilson S, Emory C. Femoral stress fractures associated with long-term bisphosphonate treatment. Clin Orthop Relat Res 2012;3:759-65.
8. Kharazmi M, Michaëlsson K, Hallberg P, Schilcher J. Lateral fixation: An alternative surgical approach in the prevention of complete atypical femoral fractures. Eur J Orthop Surg Traumatol 2018;28:299-304.
9. Min BW, Koo KH, Park YS, Oh CW, Lim SJ. Scoring system for identifying impending complete fractures in incomplete atypical femoral fractures. J Clin Endocrinol Metab 2017;102:545-50.
10. Egol K, Park J, Prensky C, Rosenberg Z, Peck V, Tejwani N. Healing delayed but generally reliable after bisphosphonate-associated complete femur fractures treated with IM nails. Clin Orthop Relat Res 2014;472:2728-34.
11. Dell R, Adams A, Greene D, Funahashi TT, Silverman SL, Eisemon EO, et al. Incidence of atypical nontraumatic diaphyseal fractures of the femur. J Bone Miner Res 2012;27:2544-50.
12. Koh A, Guerado E, Giannoudis PV. Atypical femoral fractures related to bisphosphonate treatment: Issues and controversies related to their surgical management. Bone Joint J 2017;99-B:295-302.
13. Shieh AK, Refaat M, Heyrani N, Garcia-Nolen TC, Lee MA, Eastman J. Are piriformis reconstruction implants ideal for prophylactic femoral neck fixation? Injury Int J Care Injured 2019;50(3):703-707.
14. Banfyy M, Vrahas M, Ready J, Abraham J. Nonoperative versus prophylactic treatment of bispohonate-associated femoral stress fractures. Clin Orthop Relat Res 2011;469:2028-34.
15. Ha Y, Cho M, Park K, Kim S, Koo K. Is surgery necessary for femoral insufficiency fractures after long-term bisphosphonate therapy? Clin Orthop Relat Res 2010;468:3393-98.
16. Capeci C, Tejwani N. Bilateral low-energy simultaneous or sequential femoral fractures in patients on long-term alendronate therapy. J Bone Joint Surg Am 2009;91:2556-61.
17. Chan S, Rosenberg Z, Chan K, Capeci C. Subtrochanteric femoral fractures in patients receiving long-term alendronate therapy: Imaging features. AJR Am J Roentgenol 2010;194:1581-6.
18. Sellmeyer D. Atypical fractures as a potential complication of long-term bisphosphonate therapy. JAMA 2010;304:1480-4.
 |
 |
 |
| Dr. Vivek Sodhai | Dr. Chetan Pradhan | Dr. Ashok Shyam |
| How to Cite This Article: Sodhai V, Pradhan C, Shyam A. Intramedullary Nailing: Definitive as well as Prophylactic Fixation Method in a Case of Bilateral Atypical Femoral Fractures – A Case Report. Journal of Orthopaedic Case Reports 2019 May-June; 9(3): 61-64. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com




