[box type=”bio”] Learning Point of the Article: [/box]
Femoral head fractures require careful classification and pre-operative planning and replacement arthroplasty should be considered for Pipkin Type III femoral head fractures due to high risk of avascular necrosis.
Case Report | Volume 9 | Issue 5 | JOCR September – October 2019 | Page 11-15 | Mak Wai Keong, Hamid Rahmatullah Bin Abd Razak, Wong Merng Koon, Chew Chee Ping. DOI: 10.13107/jocr.2019.v09i05.1510
Authors: Mak Wai Keong[1], Hamid Rahmatullah Bin Abd Razak[1], Wong Merng Koon[1], Chew Chee Ping[1]
[1]Department of Orthopaedics, Sengkang General Hospital, 110 Sengkang East Way, Singapore.
Address of Correspondence:
Dr. Mak Wai Keong,
Sengkang General Hospital, 110 Sengkang East Way, 544886, Singapore.
E-mail: Waikeong.mak@mohh.com.sg
Abstract
Introduction: Femoral head fractures are rare injury compared to other hip pathologies and often associated with posterior hip dislocation. Such fractures are often fraught with complications even after successful surgical fixation. Pipkin described a classification system for such fractures, dividing them into four types, of which Type III (31C.3) fractures are associated with femoral neck fractures. These fractures are the least common and often associated with the worst outcomes.
Case Report: We report a rare case of Pipkin Type III fracture after attempted hip relocation and review literature on this topic. A 35-year-old female sustained a right posterior hip dislocation with femoral head fracture following a fall. After attempts of manipulation and reduction, she sustained an iatrogenic right femoral neck fracture resulting in a Pipkin III femoral head fracture. Open reduction and reduction of fracture achieved through headless compression screw of femoral head and cortical screws of femoral neck. Four months after surgery, the patient under osteonecrosis of the femoral head and subsequently required conversion to a right total hip arthroplasty.
Conclusion: Femoral head fractures have serious sequelae and should be treated with caution. A high index of suspicion is required; hence, if clinically suspicious, proper imaging is paramount to prevent iatrogenic injury to the femoral neck resulting in subsequent avascular necrosis.
Keywords: Femoral neck fracture, Femur head, Femoral fractures, Hip dislocation, Pipkin.
Introduction
Fracture of the femoral head was first reported by Birkett, in 1869 [1], but it was only until 1957 when Pipkin described a classification system [2] categorizing the various types of injuries. He divided femoral head fractures into four types. Type I fractures below the fovea, Type II fractures above the fovea, Type III associated with femoral neck fractures, and Type IV associated with acetabular fractures. According to this classification, Type III (Orthopaedic Trauma Association classification 31C.3 [3]) injuries had the worst outcome as compared to Type I and II [4]. In most cases, femoral head fractures are caused by high impact motor vehicle accidents and sometimes fall from great height [5]. In this case report, we report a curious case of a patient who sustained a femoral head fracture from low-energy trauma. We illustrate the unusual mechanism of injury resulting in a rare Pipkin Type III posterior fracture-dislocation of the femoral head and review literature pertaining to treatment and prognosis of this condition.
Case Report
A 35-year-old female who was training for a downhill running race was running at high-speed down a hill when she tripped over a log of wood and fell forward. She subsequently complained of severe pain in her right hip and was unable to mobilize. When brought to the local hospital, plain radiograph showed a right posterior hip dislocation associated with a femoral head fracture (Fig. 1). Manipulation and reduction (M and R) were attempted, approximately within 6 h to injury, to relocate the right hip and subsequent post M and R radiographs showed iatrogenic fracture of the femoral neck (Fig. 2). She was subsequently transferred to our center for further care. On arrival, it was 48 h from the time of her injury. An urgent computed tomographic scan was done which showed a fracture-dislocation of the right hip (Fig. 3). She underwent an open surgical dislocation of the hip and internal fixation of the femoral head that same day.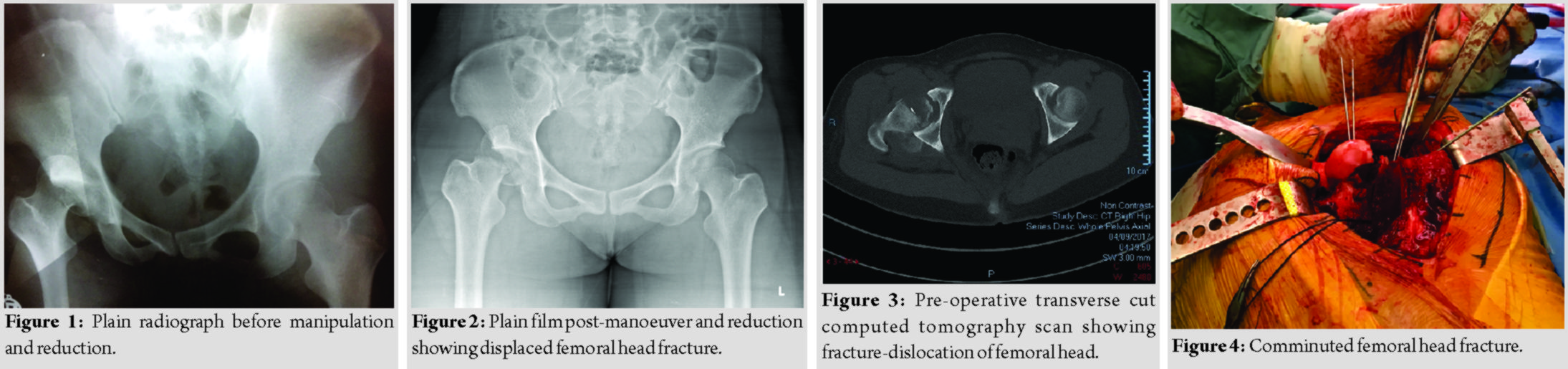
As per a standard Ganz’s osteotomy [6], with the patient placed in a lateral position and through Hardinge approach, we performed a trochanteric osteotomy flipping the osteotomized trochanteric fragment anteriorly. Ganz’s osteotomy was preferred as it allowed for full exposure of the femoral head conferring advantages in fracture reduction [6] and compared to the anterior and posterior approach had the lowest risk of avascular necrosis [4]. This approach allowed for Z-shaped anterosuperior capsulotomy to dislocate the femoral head for visualization and fixation of the fracture. The fracture line ran inferior to the fovea separating a main superior and grossly comminuted inferior fragment (Fig. 4 and 5). The largest femoral head fragment was fixed to the femoral neck with two 6.5mm Depuy Synthes (Depuy Synthes, Warsaw, IN) headless compression screws and the remaining femoral head fragments were reconstructed using4.5mm headless compression screws. The femoral head was then reduced within the acetabulum and the trochanteric flip osteotomy was fixed usingheadless and cortical screws (Fig. 6). Post-operative X-rays of the hip demonstrated good reduction of the femoral head and neck fracture. Rehabilitation was started immediately after surgery. She was kept on non-weight-bearing of the operated limb for 6 weeks with gradual increase in weight-bearing thereafter with eventual full weight-bearing status at 3 months post-surgery. Four months after surgery, the patient complained of persistent right hip pain with ambulation and was unable to wean off her crutches. Plain radiographs showed avascular necrosis of the femoral head with progressive shrink and collapse (Fig.7), resulting in prominent compression screws abutting against the acetabulum. Given the clinical picture, we counseled the patient for the removal of implants and conversion to the right total hip arthroplasty (Fig.8).The patient underwent surgery uneventfully. Rehabilitation was started immediately in the post-operative period. At 12 months following surgery, plain radiographs were satisfactory and the patient could ambulate freely without pain.
Informed consent was obtained from the patient for this case write up.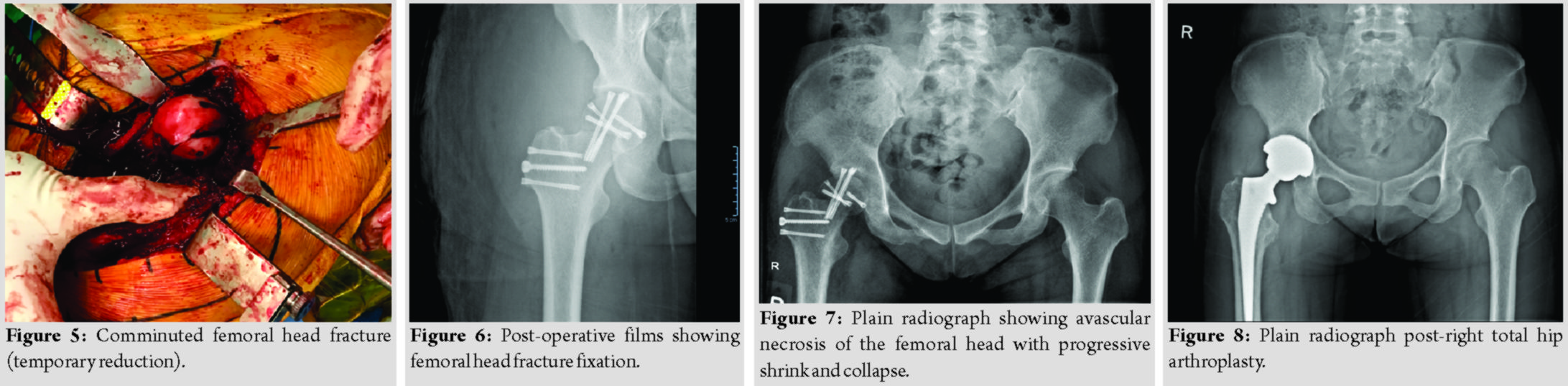
Discussion
Femoral head fractures are a rare injury compared to other hip joint pathologies and are often associated with posterior hip dislocations [7, 8, 9]. Following the first description by Birkett [1], there have been a few publications in literature in the form of case reports or series. Pipkin classifies femoral head fractures into fourtypes [2] and of those, Type III fractures were the least frequent only accounting for 8.6% of all femoral head fractures [4]. In Pipkin’s original series of patients, only 3 of 25 (12%) patients had a Type III fracture. Pipkin articulated that there are three elements in the Type 3 injury: Dislocation of the hip, fracture of the femoral head, and fracture of the femoral neck. He extrapolated the mechanism of this injury to include two forces. The first force produces the dislocation of the hip and the fracture of the femoral head; the second force then levers the dislocated head against the iliac wing so that the femoral neck is fractured. He also alluded that the pattern of this injury has been unintentionally reproduced in surgical fractures [2]. Pipkin advised that while theoretically, closed reduction is possible, an open procedure in which the neck fracture is pinned is more practical. In our patient, a femoral neck fracture was created iatrogenically after attempts at closed reduction, as this was done at a foreign hospital, we are unable to obtain information or records at the reduction techniques attempted. The increased risk of iatrogenic femoral neck fracture after closed reduction of irreducible hip dislocations compared with that after routine femoral head fracture-dislocations suggests the need for different therapeutic strategies to avoid this complication [2, 10, 11]. In recent study by Park et al. [12], it was reported that five of nine patients experienced femoral neck fractures after attempts at closed reduction. All five patients underwent hip arthroplasty at the time of injury or after developing avascular necrosis of the femoral head. Analysis of radiographs and computed tomography (CT) scans revealed that the fractured femoral head was perched on the sharp angle of the posterior wall of the acetabulum in the irreducible hips. After recognizing the irreducibility, the other four cases underwent immediate open reduction without further attempts at closed reduction, which saved the native hip without an iatrogenic neck fracture or avascular necrosis. Through their experience, the authors suggested that before attempting reduction, careful examination of plain radiographs, and CT images might be helpful for determining the safest treatment strategy. In retrospect, the CT images of our patient show features of irreducibility, and hence, imminent open reduction and fixation as opposed to closed reduction may have prevented the iatrogenic femoral neck fracture. In open treatment of such injuries, there is controversy over the optimal surgical approach. While some argue for a posterior approach due to purported lesser disruption to femoral head blood supply [10], others argued that the anterior Smith-Peterson approach offered easier access to the femoral head with successful outcomes [13, 14, 15]. Most recently, a trochanteric flip osteotomy, as performed in our case, has been described in literature [6, 16, 17, 18]. Correlating these approaches to functional scores (Thompson-Epstein criteria), trochanteric flip osteotomy was superior to posterior approach. There was no statistical significance in outcomes betweenthe three approaches [4]. However, higher rates of heterotrophic ossification have been reported with a trochanteric flip osteotomy as compared to the anterior or posterior approaches. Despite this, the trochanteric flip osteotomy demonstrated lower incidences of post-traumatic osteoarthritis with no compromise of final functional outcome [4]. Therefore, authors of this paper believed that trochanteric flip osteotomy is preferable and hence adopted this approach for our patient. Femoral head fractures are fraught with complications even after successful surgical treatment. Giannoudis et al., after analysis of 153 surgical cases from 11 articles [4], reported high complications rate including infection, post-traumatic osteoarthritis, heterotrophic ossification, and avascular necrosis. Scolaro et al. reported9% rate of avascular necrosis in their study of 69 patients with femoral head fractures [19] while others have described rates of up to 25% [10]. In the original article describing Ganz trochanteric flip osteotomy for femoral head fractures, they reported 7.7% rate of avascular necrosis from the 13 femoral head fractures they operated on Masse et al. [6]. However, it is important to note in that study, none of the patients had Pipkin Type III fractures. To the best of the author’s knowledge, there is no study describing avascular necrosis rate specifically in Type III fractures, likely due to rarity of this fracture configuration. Scolaro et al. [19] studied a series of 147 Pipkin injuries, in that series, all 13 Type III fractures were managed with open reduction and internal fixation, but this management failed with need of conversion to a total hip arthroplasty. With poorer functional outcomes as compared to type I and II fractures and high risk of avascular necrosis, arthroplasty may be a better option in place of fixation in type III fractures. However, authors of this study do feel that every effort should be made to preserve the joint in a younger patient, whereas arthroplasty would be a more viable option in the elderly.There is currently very little evidence in the use of total hip replacement (THR) for the treatment of Pipkin fractures in young individuals. However, we do also recognize that there is already extensive evidence showing good outcomes in THR for end-stage hip disease of non-traumatic causes for young patients [20, 21], spurring recommendations for primary THR in the management of type III fractures [22].
Conclusion
Femoral head fracture-dislocations have extremely variable outcomes and we recommend careful classification and pre-operative planning before attempting surgical fixation. Optimal time of reduction and surgical approach all play an important role in final outcomes and reducing risk of complication. In particular for the Pipkin Type III femoral head fracture, careful assessment of reducibility throughradiographs and CT images may be paramount to prevent an iatrogenic femoral neck fracture and subsequent avascular necrosis of the femoral head. We hope this case report contributes to further understanding of such fractures.
Clinical Message
Femoral head fractures require careful classification and pre-operative planning. Astute assessment of radiographs is required pre-reduction, post-reduction, preoperatively, and postoperatively. Although rare, replacement arthroplasty should be considered for Pipkin Type III femoral head fractures due to high risk of avascular necrosis.
References
1. Birkett J. Description of a dislocation of the head of the femur, complicated with its fracture; with remarks. Med Chir Trans 1869;52:133-8.
2. Pipkin G. Treatment of grade 4 fracture-dislocation of the hip. J Bone Joint Surg Am 1957;39-A(5):1027-42 passim.
3. Marsh JL, Slongo TF, Agel J, Broderick JS, Creevey W, DeCoster TA, et al. Fracture and dislocation classification compendium 2007: Orthopaedic trauma association classification, database and outcomes committee. J Orthop Trauma 2007;21Suppl 10:S1-133.
4. Giannoudis PV, Kontakis G, Christoforakis Z, Akula M, Tosounidis T, Koutras C. Management, complications and clinical results of femoral head fractures. Injury 2009;40:1245-51.
5. Epstein HC, Wiss DA, Cozen L. Posterior fracture dislocation of the hip with fractures of the femoral head. Clin Orthop Relat Res 1985;201:9-17.
6. Masse A, Aprato A, Alluto C, Favuto M, Ganz R. Surgical hip dislocation is a reliable approach for treatment of femoral head fractures. Clin Orthop Relat Res 2015;473:3744-51.
7. Clegg TE, Roberts CS, Greene JW, Prather BA. Hip dislocations epidemiology, treatment, and outcomes. Injury 2010;41:329-34.
8. Thompson VP, Epstein HC. Traumatic dislocation of the hip; a survey of two hundred and four cases covering a period of twenty-one years. J Bone Joint Surg Am 1951;33-A(3):746-78 passim.
9. Tonetti J, Ruatti S, Lafontan V, Loubignac F, Chiron P, Sari-Ali H, et al. Is femoral head fracture-dislocation management improvable: A retrospective study in 110 cases. Orthop Traumatol Surg Res 2010;96:623-31.
10. Epstein HC. Posterior fracture-dislocations of the hip; long-term follow-up. J Bone Joint Surg Am 1974;56:1103-27.
11. Roeder LF Jr., DeLee JC. Femoral head fractures associated with posterior hip dislocation. Clin Orthop Relat Res 1980;147:121-30.
12. Park KH, Kim JW, Oh CW, Kim JW, Oh JK, Kyung HS. A treatment strategy to avoid iatrogenic Pipkin Type 3 femoral head fracture-dislocations. Arch Orthop Trauma Surg 2016;136:1107-13.
13. Marchetti ME, Steinberg GG, Coumas JM. Intermediate-term experience of Pipkin fracture-dislocations of the hip. J Orthop Trauma 1996;10:455-61.
14. Stannard JP, Harris HW, Volgas DA, Alonso JE. Functional outcome of patients with femoral head fractures associated with hip dislocations. Clin Orthop Relat Res 2000;377:44-56.
15. Swiontkowski MF, Thorpe M, Seiler JG, Hansen ST. Operative management of displaced femoral head fractures: Case-matched comparison of anterior versus posterior approaches for Pipkin I and Pipkin II fractures. J Orthop Trauma 1992;6:437-42.
16. Ganz R, Gill TJ, Gautier E, Ganz K, Krügel N, Berlemann U. Surgical dislocation of the adult hip a technique with full access to the femoral head and acetabulum without the risk of avascular necrosis. J Bone Joint Surg Br 2001;83:1119-24.
17. Henle P, Kloen P, Siebenrock KA. Femoral head injuries: Which treatment strategy can be recommended? Injury 2007;38:478-88.
18. Keel MJ, Bastian JD, Büchler L, Siebenrock KA. Surgical dislocation of the hip for a locked traumatic posterior dislocation with associated femoral neck and acetabular fractures. J Bone Joint Surg Br 2010;92:442-6.
19. Scolaro JA, Marecek G, Firoozabadi R, Krieg JC, Routt ML. Management and radiographic outcomes of femoral head fractures. J Orthop Traumatol 2017;18:235-41.
20. Swarup I, Shields M, Mayer EN, Hendow CJ, Burket JC, Figgie MP. Outcomes after total hip arthroplasty in young patients with osteonecrosis of the hip. Hip Int 2017;27:286-92.
21. Rajaee SS, Theriault RV, Pevear ME, Smith EL. National trends in primary total hip arthroplasty in extremely young patients: A focus on bearing surface usage from 2009 to 2012. J Arthroplasty 2016;31Suppl 9:63-8.
22. Tosounidis T, Aderinto J, Giannoudis PV. Pipkin Type-III fractures of the femoral head: Fix it or replace it? Injury 2017;48:2375-8.
 |
 |
 |
 |
| Dr. Mak Wai Keong | Dr. Hamid Rahmatullah Bin Abd Razak | Dr. Wong Merng Koon | Dr. Chew Chee Ping |
| How to Cite This Article: Keong M W, Razak H R B A, Koon W M, Ping C C. Case Report of a Rare Pipkin Type III Femoral Head Fracture. Journal of Orthopaedic Case Reports 2019 Sep-Oct; 9(5): 11-15. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com




