[box type=”bio”] Learning Point of the Article: [/box]
A trial of conservative management should be tried before any intervention; angiography and selective arterial embolization of the geniculate arteries can be an effective treatment in appropriately selected patients.
Case Report | Volume 10 | Issue 1 | JOCR January – February 2020 | Page 22-25| Prabhudev P Purudappa, Om P Sharma, Munis Ashraf, Senthil N Sambandam. DOI: 10.13107/jocr.2019.v10i01.1622
Authors: Prabhudev P Purudappa[1], Om P Sharma[2], Munis Ashraf[3], Senthil N Sambandam[4]
[1]Department of Orthopaedic Surgery, VA Medical Center, Boston Orthopedics 6C150 S Huntington Avenue Boston, Massachusetts 02130, United States.
[2]Department of Orthopaedic Surgery, Essentia Health St. Mary’s-Detroit Lakes Clinic 1027 Washington Ave, Detroit Lakes, Minnesota 56501, United States
[3]Department of Orthopaedic Surgery, Yenepoya Medical College Hospital, Mangalore, India., 4Department of Orthopaedic Surgery, Louis A Johnson VA Medical Center Clarksburg, West Virginia 26301, United States.
Address of Correspondence:
Dr. Munis Ashraf,
Department of Orthopaedic Surgery, Yenepoya Medical College Hospitals, Mangalore, India.
E-mail: munis6gmail.com
Abstract
Introduction: Spontaneous recurrent hemarthrosis of the knee following a total knee arthroplasty is a rare complication with varying time of onset from 2 months to 18 years. It needs a prompt diagnosis and treatment to prevent complications of stiffness, chronic pain, and limited function. We present a case of spontaneous recurrent hemarthrosis presenting at 3 months following a total knee arthroplasty with a follow-up to 1 year.
Case Report: A 66-year-old male presented at 3 months following a right total knee arthroplasty with a history of increased pain and swelling of the knee joint. Initially, he was treated with anti-inflammatories when the pain and swelling recurred, an aspiration demonstrated hemarthrosis of the knee. Further evaluation demonstrated no infection, a femoral angiography demonstrated prominence of medial superior and inferior geniculate arteries with a tumor blush appearance. Therapeutic embolization of both the arteries resulted in complete resolution of the symptoms in 1 month with return of full knee function. At the end of 1-year follow-up, the patient had return of full knee function with no pain and no recurrence.
Conclusion: An algorithmic approach is helpful in identifying the etiology of spontaneous recurrent hemarthrosis of knee and a course of conservative treatment should always be the first line of treatment. Angiography and selective arterial embolization of the geniculate arteries can be an effective treatment in the management of recurrent spontaneous hemarthrosis.
Keywords: Spontaneous hemarthrosis, knee arthroplasty, embolization.
Introduction
Recurrent spontaneous hemarthrosis post total knee replacement is a rare complication with an incidence ranging from 0.1% to 1.6% [1,2,3,4,5]. The time of onset has been reported to be an average of 2 years from the surgery, but it can vary from 2 months to 18 years [1,3,5,6]. The etiology of this condition has not been well understood, it can be due to various conditions such as direct vessel injury to the popliteal artery, geniculate arteries [7,8], arteriovenous fistula, and pseudoaneurysms [9]. Impingement of the proliferative synovium between the articulating components is the most common cause of recurrent proliferative hemarthrosis [9] after excluding the coagulopathies. It is important to diagnose this condition promptly and treat appropriately to prevent complications of stiffness, chronic pain, and limited function. We report a case of spontaneous recurrent hemarthrosis following a total knee arthroplasty at 3 months postoperatively which was successfully treated with selective arterial embolization.
Case Report
A 66-year-old male underwent a right total knee arthroplasty for end-stage tricompartmental osteoarthritis in July 2018. His immediate post-operative recovery was uneventful. He was progressing well at 2 and 6 weeks follow-up with minimal pain and minimal swelling in the knee. He was able to perform activities of daily living with minimal difficulty. At 3-month post-surgery, he complained of moderately increased pain and swelling of the right knee after minor twisting type of injury to the knee. He was treated with tab. naproxen 500mg twice daily, which gave him good pain relief for about 2 weeks. He was also evaluated to rule out prosthetic joint infection, and his erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) were within normal limits. He was seen at 2 weeks at which time, the patient reported that his pain and swelling have improved, and he was able to function better. He came back to the clinic next day with sudden increase in pain and swelling, limited range of motion, and difficulty with walking. No history of any fever or chills reported. Clinical examination demonstrated moderate-sized knee effusion, local warmth, no erythema, and a range of motion of 10–100°. He was again treated symptomatically with ice application, naproxen for pain. His pain and swelling gradually improved and he was able to return to some of his activities. He returned to the clinic again after about 3 weeks with increasing pain and swelling of his right knee and no history of fever or chills. His knee examination demonstrated a large tense effusion, local warmth, severe tenderness to palpation, and limited range of motion of 10–70°. His knee aspiration produced 30 cc of frank blood and his ESR and CRP were 4mm/h and 3.9mg/L, respectively. The cultures came back negative. He was not on any anticoagulation medication except for 2 weeks immediate post-operative for deep vein thrombosis prophylaxis. He was also not known to have any bleeding disorders. His pain and swelling improved temporarily after the aspiration but returned within a week.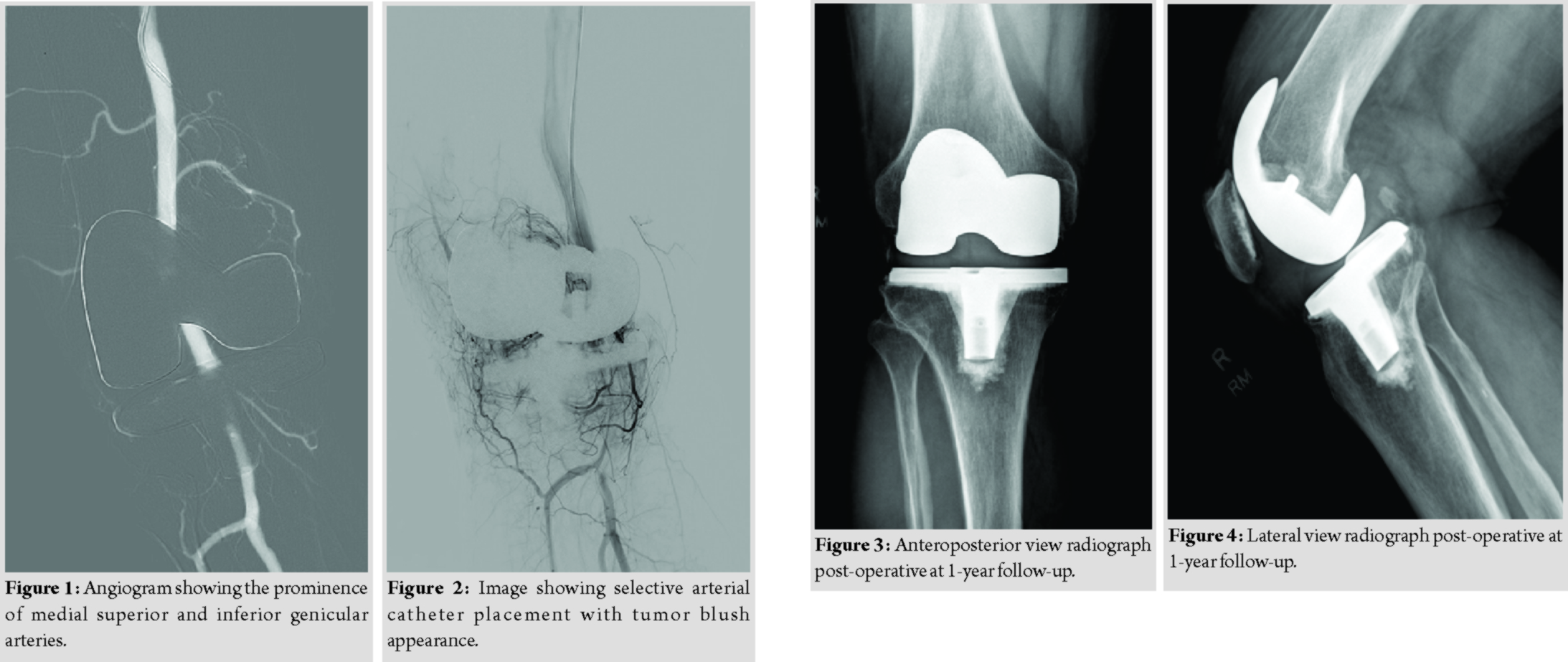
In consultation with vascular surgeons and interventional radiology, he underwent a computed tomography angiogram to evaluate for any vascular abnormalities, leading to hemarthrosis of the knee. This demonstrated prominence of medial superior and inferior geniculate vessels in the right knee, but a detailed evaluation was limited due to artifacts form the knee implant. No extravasation was identified. He then underwent a right femoral angiography through the left femoral approach which again demonstrated prominent medial superior and inferior geniculate arteries (Fig. 1). A 5 Fr angiography catheter was placed in the right medial superior geniculate artery and a 3 Fr. Microcatheter was placed coaxially throughthe 5 Fr catheter more distally into the medial superior geniculate artery for super selective angiography, which showed synovial hypervascularity and blush. This geniculate artery was subsequently embolized with one-fourth vial of microspheres (500 µ in size). The 5 Fr angiography catheter was then placed in the right medial inferior geniculate artery and a 3 Fr microcatheter was placed coaxially via the 5 Fr catheter more distally into the medial inferior geniculate artery for superselective angiography, which showed synovial hypervascularity and tumor blush (Fig. 2). This geniculate artery was subsequently embolized with one-fifth vial of microspheres (500 micron in size). Post-embolization right femoral angiography showed these geniculate arteries to be occluded. The patient was discharged home on the same day and was recommended to return to activities as tolerated. He was seen in the orthopedic clinic at 1 month from the procedure at which time, the patient reported complete resolution of the swelling and pain in his right knee. He was back to all his activities with no limitations. The patient continues to be asymptomatic and no recurrence of the hemarthrosis at 12-month follow-up (Fig. 3and 4).
Discussion
Recurrent spontaneous hemarthrosis can severely limit the function of the knee following a total knee arthroplasty. It should be promptly diagnosed, and a course of conservative treatment should always be tried before any surgical procedures. Saksena et al. [9] recommended an algorithmic approach in the evaluation of hemarthrosis of the knee. All the anticoagulation medications should be stopped, and the patient should be evaluated for any coagulopathies. Rest, ice, aspiration, and immobilization should be done following a large hemarthrosis. Prosthetic joint infection should always be ruled out with inflammatory markers and cultures of the aspirate [9, 10]. When the conservative treatment method fails, and the patient has recurrent hemarthrosis, angiography has been used as a first-line procedure to help with the diagnosis and then proceed with treatment [9]. This technique has been successfully used in the treatment of pseudoaneurysms and arteriovenous fistulas previously [11,12].
Many authors have been using selective arterial embolization of the geniculate arteries to diminish the blood flow into hypertrophic synovium, thereby treating the recurrent hemarthrosis. Weidner et al. [10] reported successful resolution of recurrent hemarthrosis in 12 of 13 patients treated with geniculate arterial embolization. One clinical failure likely represented misdiagnosed prosthetic joint infection. Two patients had transient cutaneous ischemia following embolization which resolved spontaneously. In their study, the average time interval between arthroplasty and onset of hemarthrosis was 47 months. Bagla et al. [6] treated fivepatients with selective geniculate arterial embolization; angiography demonstrated synovial hypervascularity with geniculate artery tumor blush appearance in all patients. There was a complete resolution of the symptoms and effusion at an average time of 2.6 weeks with no recurrences during the follow-up. The angiographic examination in our patient also demonstrated typical synovial hypervascularity with the geniculate artery tumor blush appearance. It was successfully treated with microsphere embolization of the geniculate artery.
Spontaneous recurrent hemarthrosis after a total knee arthroplasty is more often reported as a late complication. Weidner et al. [10] had three out of 13 patients which presented within the 1styear of post-operative period. Kindsfater and Scott [3] in their series of 30 patients, the average interval from implantation to recurrent hemarthrosis was 24.2 months (range from 2 weeks to 144 months). Our patient presented at 3 months from the time of total knee replacement surgery. Guevara et al. [13] reported on 10 patients who underwent geniculate artery embolization, hemarthrosis resolved in six patients. Four patients required repeat embolization, of which two patients had resolution of the hemarthrosis. Three of the four patients who required repeat embolization had serious medical comorbidities such as blood dyscrasias or on therapeutic anticoagulation. Their study showed that the geniculate artery embolization had limited clinical success and higher repeat embolization rates in patient with serious comorbidities. Dhondt et al. [14] included the eight patients with the spontaneous hemarthrosis in their study, five of them were treated with selective embolization, and three of which were successful after the first attempt. One patient had resolution after two attempts and another one needed open surgery after two failed attempts.
The observations from literature review are that spontaneous recurrent hemarthrosis of knee is most often reported as a late complication; treatment modalities which have been tried are conservative management, selective arterial embolization, and open ligation of feeder vessel; recurrence of effusion following conservative management and selective embolization has been reported.
Conclusion
This case report emphasizes the importance of early diagnosis of recurrent hemarthrosis following total knee arthroplasty to prevent significant consequences. An algorithmic approach is helpful in identifying the etiology of hemarthrosis; a course of conservative treatment should always be the first line of treatment. Angiography should be used as one of the early diagnostic procedures when the conservative treatment fails, and selective arterial embolization of the geniculate arteries can be an effective treatment in the management of recurrent spontaneous hemarthrosis. The procedure may be less effective in patients with serious comorbidities such as blood dyscrasias and therapeutic anticoagulation.
Clinical Message
A high index of suspicion in cases with spontaneous knee effusion is imperative for the early diagnosis of spontaneous hemarthrosis. A trial of conservative management should be tried before any intervention. Angiography and selective arterial embolization of the geniculate arteries can be an effective treatment in appropriately selected patients
References
1. OhderaT, TokunagaM, HiroshimaS, YoshimotoE, MatsudaS. Recurrent hemarthrosis after knee joint arthroplasty: Etiology and treatment.J Arthroplasty2004;19:157-61.
2. SuzukiM, KakizakiJ, TsukeokaT, TsuneizumiY, MiyagiJ, MoriyaH. A case of spontaneous hemoarthrosis after a total knee arthroplasty.Mod Rheumatol2006;16:248-50.
3. KindsfaterK, ScottR. Recurrent hemarthrosis after total knee arthroplasty.J Arthroplasty1995;10 Suppl:S52-5.
4. OishiCS, ElliottML, ColwellCW Jr. Recurrent hemarthrosis following a total knee arthroplasty.J Arthroplasty1995;10 Suppl:S56-8.
5. WorlandRL, JessupDE. Recurrent hemarthrosis after total knee arthroplasty.J Arthroplasty1996;11:977-8.
6. BaglaS, RhollKS, vanBreda A, SterlingKM, vanBreda A. Geniculate artery embolization in the management of spontaneous recurrent hemarthrosis of the knee: Case series.J VascIntervRadiol2013;24:439-42.
7. RandJA. Vascular complications of total knee arthroplasty. Report of three cases.J Arthroplasty1987;2:89-93.
8. HolmbergA, MilbrinkJ, BergqvistD. Arterial complications after knee arthroplasty: 4 cases and a review of the literature.Acta OrthopScand1996;67:75-8.
9. SaksenaJ, PlattsAD, DowdGS. Recurrent haemarthrosis following total knee replacement.Knee2010;17:7-14.
10. WeidnerZD, HamiltonWG, SmirniotopoulosJ, BaglaS. Recurrent hemarthrosis following knee arthroplasty treated with arterial embolization.J Arthroplasty2015;30:2004-7.
11. HaddadFS, PrendergastCM, DorrellJH, PlattsAD. Arteriovenous fistula after fibular osteotomy leading to recurrent haemarthroses in a total knee replacement.J Bone Joint Surg Br1996;78:458-60.
12. IbrahimM, BoothRE Jr., ClarkTW. Embolization of traumatic pseudoaneurysms after total knee arthroplasty.J Arthroplasty2004;19:123-8.
13. GuevaraCJ, LeeKA, BarrackR, DarcyMD. Technically successful geniculate artery embolization does not equate clinical success for treatment of recurrent knee hemarthrosis after knee surgery.J VascIntervRadiol2016;27:383-7.
14. DhondtE, VanhoenackerFM, D’Archambeau O, SnoeckxA, DefreyneL. Angiographic findings and therapeutic embolization of late hemarthrosis after total joint arthroplasty.Skeletal Radiol2009;38:31-6.
 |
 |
 |
 |
| Dr. Prabhudev P Purudappa | Dr. Om P Sharma | Dr. Munis Ashraf | Dr. Senthil N Sambandam |
| How to Cite This Article: Purudappa PP, Sharma O P, Ashraf M, Sambandam S N. Spontaneous Recurrent Hemarthrosis Post Total Knee Arthroplasty Treated with Selective Embolization – A Case Report and Review of Literature. Journal of Orthopaedic Case Reports 2020 Jan-Feb;10(1): 22-25. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com




