[box type=”bio”] Learning Point of the Article: [/box]
The very rare case of nail breakage after humerus fracture treatment can be adressed with a one stage procedure, even after a long standing non-union of the fracture.
Case Report | Volume 10 | Issue 1 | JOCR January – February 2020 | Page 89-92 | Giovanni Ziveri, Carlo Felice De Biase. DOI: 10.13107/jocr.2020.v10.i01.1652
Authors: Giovanni Ziveri[1], Carlo Felice De Biase[1]
[1]Department of Traumatology and Shoulder Surgery, “Città di Parma” Hospital, Piazzale Athos Maestri 5, Parma, Italy.
Address of Correspondence:
Dr. Giovanni Ziveri,
Casa di curaCittà di Parma, Piazzale Athos Maestri 5, Parma, Italy.
E-mail: gioctor@gmail.com
Abstract
Introduction: The rate of nonunion of operatively treated fractures of humeral shaft is low. Increased incidence of nonunion is associated with different conditions such as open fractures, bone loss, or fracture gapping. Nonunions after prior intramedullary nailing can be difficult to address, even more with hardware failure. We present the case of a humeral nail breakage 11 years after implantation, secondary to nonunion.
Case Report: A 33-year-old man referred to our hospital with oligotrophic nonunion of the middle humeral diaphysis and nail breakage after 11 years from the first fracture. We decided then to schedule a one-stage surgical procedure of nail removal and new osteosynthesis with autogenous iliac crest bone graft.
Conclusions: The patient presented good clinical evolution, without functional limitation or pain. Bone graft union was radiologically confirmed at final follow-up. To the best of our knowledge, this is the first case of non-traumatic nail breakage in a humeral shaft nonunion after such a long period of time. In this case, we found that a one-stage surgical procedure with nail removal and locking compression plate fixation associated with tricortical autogenous iliac crest bone grafting after long-standing humeral shaft nonunion is favorable.
Keywords: Humerus, nail, breakage, nonunion, treatment.
Introduction
Fractures of the humeral shaft account for 3–5% of all fractures and approximately 30% of those of the humerus [1, 2] While there may be some consensus on the nature of operative treatment, in general, the choice of the fixation device (plate vs. nail) is still debated [3]. The rate of nonunion is reported to range from 3% to 5% of all operatively treated fractures while after non-operative treatment is higher and described as up to 23% in literature [4, 5, 6, 7, 8].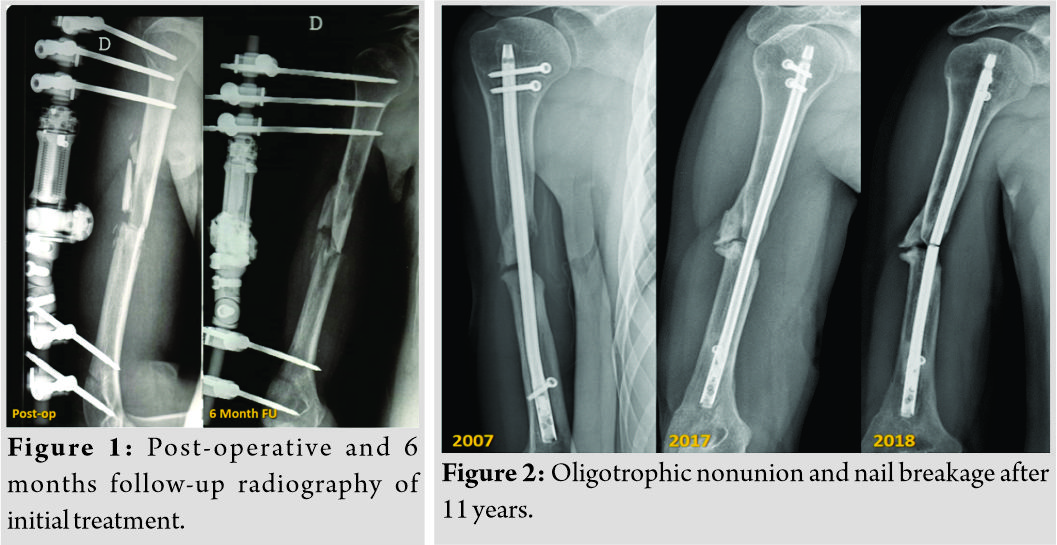
Increased incidence of nonunion is associated with open fractures, high-impact injuries, bone loss or fracture gapping, soft tissue interposition, unstable fracture patterns, segmental fractures, impaired blood supply, infection, and initial treatment with traction or a hanging cast [2]. The patient factors such as obesity, osteoporosis, alcoholism, malnutrition, and non-compliance also are influential [2, 9, 10]. Humeral nonunions after prior intramedullary (IM) nailing can be difficult to address due to possible bone loss around a loose nail, which complicates the reconstructive procedure and lead to poorer operative results compared to prior non-operative treatment or plate fixation [11].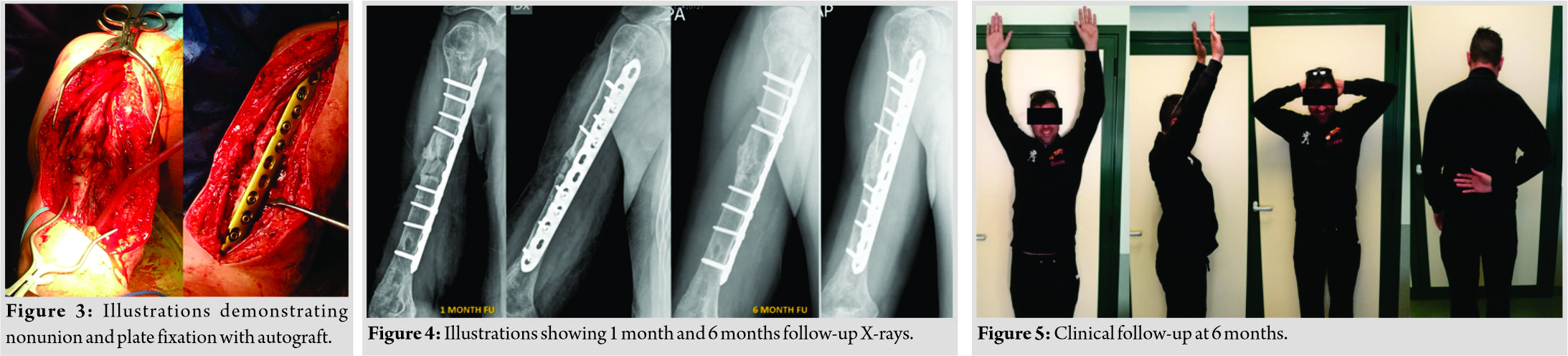
Different treatment techniques have been described for the specific reconstructive problems including open reduction and plating with the removal of the nail, exchange IM nailing, Ilizarov external fixation, and the application of a wave plate [5,11, 12, 13, 14, 15].
Herein, we present the case of a 33-year-old male with nail breakage 11 years after implantation, secondary to nonunion of the humeral shaft. To the best of our knowledge, it is the first case reported in literature.
Case Report
A 33-year-old man referred to our hospital with oligotrophic nonunion of the middle humeral diaphysis and nail breakage. He had a history of Gustilo type I open fracture 12 years before (May 2006), secondary to a motorcycle accident, with a multifragmentary pattern (Arbeitsgemeinschaft für Osteosynthesefragen/Orthopedic Trauma Association type 12B3). He had been initially treated with debridement, wound closure, and positioning of a uniplanar external fixator. After 6 months of clinical and radiological follow-up, there were no signs of healing and persistent pain at fracture site (Fig. 1). It was then decided to convert the external fixator into a roamed retrograde IM nail. The patient was followed up clinically and radiologically until 2017 and had returned to his normal life without complaining of any pain during everyday life and working activity. Unfortunately, unlike the good clinical outcome, the follow-up X-rays showed an oligotrophic nonunion of the midshaft of the humerus with, at least, 1 cm of bone loss. A year later(May 2018), the patient came to our attention because, after a mere twisting movement, he heard a snap and, subsequently, pain and loss of function to the right arm. With plain radiographs, a nail breakage was assessed (Fig. 2). He complained of moderate pain and functional disability of the involved limb and was then admitted to our hospital. Full blood count, sedimentation rate, and C-reactive protein level were preoperatively investigated for infection and were negative. We decided then to schedule a one-stage surgical procedure of nail removal and new osteosynthesis with autogenous iliac crest bone graft. After regional nerve block and general anesthesia, the patient is seated in a lazy beach chair position, with the head of the bed elevated approximately 30°. This position allows good surgical exposure of the humerus and eases access to the iliac crest. In addition, a padded bump is placed under the ipsilateral hip to ease in the access of the iliac crest by increasing the crests’ prominence. The humeral nonunion was exposed through an extended anterolateral approach. A straight incision at the lateral border of the biceps muscle was made, and, after cutting the fascia, the biceps muscle was retracted medially, bringing the brachialis muscle into view. The brachialis muscle was split longitudinally throughout its lateral third and transected down to the bone. Through deltopectoral surgical exposure, the two proximal screws were removed. Distally, the radial nerve was identified, surrounded with a vessel loop and the distal screw was then removed. The nonunion zone was debrided by removing all fibrous tissue, interposed muscle, and necrotic bone followed by decortication, until bleeding bone was observed to provide a viable bed for the bone graft and to stimulate callus formation. The debridement left almost 2 cm bone gap and exposed the broken nail which was removed. A tricortical bone graft is obtained from the iliac crest according to previously described technique [16]. The iliac crest graft was trimmed to enable it to snugly telescope into the fracture fragments (the harvested bone graft was then packed into the defect) and then, a 4.5mm limited contact dynamic compression plate was placed on the anterior face of the humerus (Fig. 3). Dynamic examination of the synthesis under fluoroscopy has been used as an intraoperative method to assess the stability of the construct. Wound closure was provided. Three sets of intraoperative cultures were done with negative results. Post-operative X-rays showed good alignment of the nonunion and refilling of the bone defect. The patient was allowed early rehabilitation with free shoulder and elbow motion to avoid joint stiffness. He was followed up radiologically at regular time intervals of 4 weeks and clinically with Constant shoulder score (CS), subjective shoulder value (SSV), and visual analog scale (VAS). Visits were scheduled until bone graft union was radiologically confirmed at final follow-up (Fig. 4). At this point, good clinical function was achieved with SSV of 80%, VAS 0, and CS of 76 (Fig. 5).
Discussion
To the best of our knowledge, this is the first case of nail breakage in a humeral shaft nonunion after a long period of time. A shaft nonunion in long bone fractures after IM nailing is usually a rare complication, especially since the introduction of locking nails. However, it has been indicated that the treatment of diaphyseal nonunions after failed locked nailing of the humerus is not analogous to similar problems observed in the tibia or femur [17]. While in the lower limb, body weight and smaller torsional forces contribute to dynamic loading, the humerus is subject to more rotatory forces and minor axial loading [18]. Still, rotational instability combined with gap distraction at the fracture site contributes to the majority of humeral shaft nonunions after IM nailing [19].
In our opinion, this rotational force to which the arm has been subjected for such a long period of time (11 years) in association with nonunion of the fracture could have led to hardware breakage in this patient. Any nail, in fact, can resist a specific number of cycles and the lack of healing at a certain time might cause an implant failure. This complication is rare and reported in literature for implants in proximal femoral fractures [20]. Most of the fractures that presented this complication were initially classified as unstable and were presented as nonunion at the fracture site at the last follow-up previous to the implant breakage [21].
Humeral nonunions after prior IM nailing can be difficult to address, even more with nail breakage. Conventionally, removal of the IM device followed by open compression plating has been advocated and has shown high healing rates [11]. Lin et al. presented a large study of 86 patients with humeral shaft nonunions managed by the removal of previous implants, open reduction, and internal fixation with dynamic compression plating, supplemented with cancellous bone grafts. Of these patients, 38 were primarily treated with IM nailing. All nonunions healed within an average of 18 weeks [22]. McKee et al.[11] reported the treatment results of nail removal and plating (9 patients) and exchange nailing (10 patients). Union was achieved in all patients with plating and bone grafting but in only 4 of 10 patients with exchange nailing. Exchange nailing alone appears to be ineffective, as Flinkkila et al. [17] found a similar low healing rate of nonunions in 6 of 13 patients. Better results have been reported when exchange nailing is combined with decortication, fibrous tissue removal, and bone grafting. Lin et al. [23] reported on 23 patients treated by open exchange locked nailing with bone grafting, with additional compression wiring in 19 of those patients. All but one nonunion healed.
Conclusion
In this case, we found that the outcomes after locking compression plate (LCP) fixation associated with tricortical autogenous iliac crest bone grafting for long-standing humeral shaft nonunion are favorable. LCP fixation can achieve a high degree of cortex-to-cortex stability with compression of the bone segments and correction of the malalignment. In addition, an autogenous graft with intimate contact with both fragments may facilitate neovascularization and migration of osteogenic cells, which can foster an environment conducive to bone healing. The range of motion of the patient’s shoulder recovered to its pre-injury level. Therefore, we can suggest that this technique could be employed for treating humeral shaft nonunion associated with nail breakage even after such a long period of time.
Clinical Message
Non-traumatic breakage of the IM nail is an uncommon complication. The implant failure usually occurs when the fracture does not achieve the consolidation. It is usually observed after lower limb fracture treatment and never described so far for humerus nailing. The very rare case of nail breakage after humerus fracture treatment can be addressed with a one-stage procedure, even after a long-standing nonunion of the fracture (11 years in this patient).
References
1. Brinker MR, O’Connor DP. The incidence of fractures and dislocations referred for orthopaedic services in a capitated population. J Bone Joint Surg Am 2004;86:290-7.
2. Ward EF, Savoie FH 3rd, Hughes JL Jr. Fractures of the diaphyseal humerus. In: Browner BD, Jupiter JB, Levine AM, Trafton PG, editors. Skeletal Trauma: Fractures, Dislocations, Ligamentous Injuries. 2nd ed., Vol. 2. Philadelphia, PA: WB Saunders; 1998. p. 1523-47.
3. Bhandari M, Devereaux PJ, McKee MD, Schemitsch EH. Compression plating versus intramedullary nailing of humeral shaft fracturesa meta-analysis. Acta Orthop2006;77:279-84.
4. Rommens PM, Kuechle R, Bord T, Lewens T, Engelmann R, Blum J, et al. Humeral nailing revisited. Injury 2008;39:1319-28.
5. Kontakis GM, Papadokostakis GM, Alpantaki K, Chlouverakis G, Hadjipavlou AG, Giannoudis PV, et al. Intramedullary nailing for non-union of the humeral diaphysis: A review. Injury 2006;37:953-60.
6. Denard A Jr., Richards JE, Obremskey WT, Tucker MC, Floyd M, Herzog GA, et al. Outcome of nonoperative vs operative treatment of humeral shaft fractures: A retrospective study of 213 patients. Orthopedics 2010;33:33-8.
7. Rutgers M, Ring D. Treatment of diaphyseal fractures of the humerus using a functional brace. J Orthop Trauma 2006;20:597-601.
8. Toivanen JA, Nieminen J, Laine HJ, Honkonen SE, Järvinen MJ. Functional treatment of closed humeral shaft fractures. Int Orthop2005;29:10-3.
9. Rosen H. The treatment of nonunions and pseudarthroses of the humeral shaft. Orthop Clin North Am 1990;21:725-42.
10. Jupiter JB, von Deck M. Ununited humeral diaphyses. J Shoulder Elbow Surg 1998;7:644-53.
11. McKee MD, Miranda MA, Riemer BL, Blasier RB, Redmond BJ, Sims SH, et al. Management of humeral nonunion after the failure of locking intramedullary nails. J Orthop Trauma 1996;10:492-9.
12. Catagni MA, Guerreschi F, Probe RA. Treatment of humeral nonunions with the ilizarov technique. Bull Hosp Jt Dis Orthop Inst 1991;51:74-83.
13. Ring D, Jupiter JB, Quintero J, Sanders RA, Marti RK. Atrophic ununited diaphyseal fractures of the humerus with a bony defect: Treatment by wave-plate osteosynthesis. J Bone Joint Surg Br 2000;82:867-71.
14. Patel VR, Menon DK, Pool RD, Simonis RB. Nonunion of the humerus after failure of surgical treatment. Management using the ilizarov circular fixator. J Bone Joint Surg Br 2000;82:977-83.
15. Gerber A, Marti R, Jupiter J. Surgical management of diaphyseal humeral nonunion after intramedullary nailing: Wave-plate fixation and autologous bone grafting without nail removal. J Shoulder Elbow Surg 2003;12:309-13.
16. Giannoudis PV, Karadimas EJ, Kanakaris NK. Anterior iliac crest bone graft harvesting. In: Giannoudis P, editor. Practical Procedures in Orthopedic Surgery. London: Springer; 2011.
17. Flinkkilä T, Ristiniemi J, Hämäläinen M. Nonunion after intramedullary nailing of humeral shaft fractures. J Trauma 2001;50:540-4.
18. Blum J, Machemer H, Baumgart F, Schlegel U, Wahl D, Rommens PM, et al. Biomechanical comparison of bending and torsional properties in retrograde intramedullary nailing of humeral shaft fractures. J Orthop Trauma 1999;13:344-50.
19. Baltov A, Mihail R, Dian E. Complications after interlocking intramedullary nailing of humeral shaft fractures. Injury 2014;45 Suppl 1:S9-15.
20. Alvarez DB, Aparicio JP, Fernández EL, Múgica IG, Batalla DN, Jiménez JP, et al. Implant breakage, a rare complication with the gamma nail. A review of 843 fractures of the proximal femur treated with a gamma nail. Acta OrthopBelg2004;70:435-43.
21. Marcos CS. Salvage for nail breakage in femoral intramedullary nailing. Injury 2015;46:729-33.
22. Lin CL, Fang CK, Chiu FY, Chen CM, Chen TH. Revision with dynamic compression plate and cancellous bone graft for aseptic nonunion after surgical treatment of humeral shaft fracture. J Trauma 2009;67:1393-6.
23. Lin J, Chiang H, Hou SM. Open exchange locked nailing in humeral nonunions after intramedullary nailing. Clin OrthopRelat Res 2003;411:260-8.
 |
 |
| Dr. Giovanni Ziveri | Dr. Carlo Felice De Biase |
| How to Cite This Article: Ziveri G, De Biase CF. A Case Report of Humeral Nail Breakage after 11 Years Secondary to Shaft Nonunion: Treatment with Autogenous Iliac Crest Bone Graft and Compression Plate. Journal of Orthopaedic Case Reports 2020 Jan-Feb;10(1): 89-92. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com




