[box type=”bio”] Learning Point of the Article: [/box]
Raise awareness of BPOP and to help the surgeons to distinguish them from more common differentials.
Case Report | Volume 10 | Issue 1 | JOCR January – February 2020 | Page 45-50 | Supreet N Bajwa, Rajeev Reddy, Yash S Wagh, Manish Agarwal, Ameya Katariya. DOI: 10.13107/jocr.2020.v10.i01.1630
Authors: Supreet N Bajwa[1], Rajeev Reddy[1], Yash S Wagh[1], Manish Agarwal[1], Ameya Katariya[1]
1]Department of Orthopaedics, P.D. Hinduja National Hospital, Mumbai, Maharashtra, India.
Address of Correspondence:
Dr. Supreet N Bajwa,
Department of Orthopaedics, P.D. Hinduja National Hospital, Mumbai, Maharashtra, India.
E-mail: supreetbajwa90@gmail.com
Abstract
Introduction: Bizarre parosteal osteochondromatous proliferationis a distinct entity which requires proper radiological and pathological distinction for correct surgical management.
Case Report: We present a series of four cases which were misdiagnosed by the treating surgeons, reporting radiologists and pathologists due to clinical and investigatory consistencies with other benign or malignant orthopedic tumors. Due to common diagnostic errors of these uncommon tumors, the patients had recurrence and required multiple invasive procedures which could have been avoided with high index of suspicion.
Conclusion: Dueto high local recurrence rates and a lack of adjuvant therapy options, this lesion will continue to pose a challenge for orthopedic surgeons and more awareness ofthis lesion will help identify and understand that a wide excision, with no compromise related to the margins, is required for this benign-appearing lesion.
Keywords: Bizarre parosteal osteochondromatous proliferation, Nora Lesion, Osteochondromatosis.
Introduction
Bizarre parosteal osteochondromatous proliferation (BPOP), also called Nora’s Lesion, was described in 1983 by Nora et al.[1] as a rare benign but locally aggressive lesion usually misdiagnosed on initial presentation and commonly mistreated. Less than 200 cases have been published in literature to date, thereby diminishing the knowledge of this tumor in routine orthopedic practice. The lesion is characterized typically by a well-marginated exophytic outgrowth from the periosteal surface with an intact cortex without medullary changes and consisting of bone, cartilage, and fibrous tissue [2].Original literature suggests it to be found most commonly in tubular bones of hands and feet with phalanges, metacarpals, and metatarsals being more involved [3]. However, these tumors are also reported in long bones [4] as also seen in our case series (three out of four cases). These lesions are commonly found in the second and third decades of life with no sex predilection [5].BPOP may be wrongly considered too benign or malignant due to the frequent misdiagnosis by orthopedicians, radiologists, and pathologists as well due to the variable presentation of the lesion. Grossly, typical BPOP may resemble an osteochondroma but with high frequency of recurrence, fast-growing, and distinct histopathological appearance with marked proliferative activity, bizarre binucleated chondrocytes (mimicking chondrosarcoma but without cellular atypia), and also showing fibrous myxoid spindle cell stroma and basal bony trabeculae with high osteoblastic activity and uneven calcification. Atypical radiological presentation may resemble myositis ossificans or juxtacortical osteosarcoma. In this case series of four cases, we discuss the various presentations of this distinct lesion (with cases of cortical destruction) with various radiological presentations of BPOP which on recurrence can be considered a malignant entity.
Case Report
Case 1
A 34-year-old female was referred to our hospital after undergoing an excision of a distal lateral fibular swelling in another hospital which was reported to be an osteochondroma (Fig. 1a). The patient had a local recurrence with the mass recurring at the same site within 10 months of initial presentation(Fig. 1b). She gave no history of trauma preceding the initial swelling.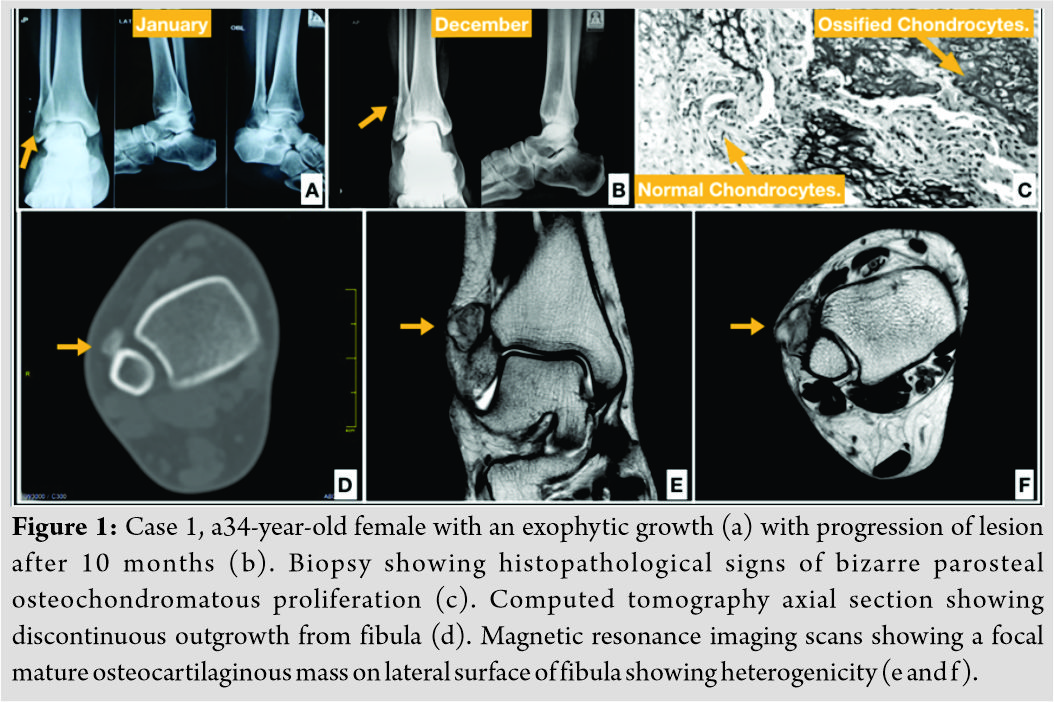 The rapid growth caused pain localized to the lateral side of the leg. On examination, she had a linear longitudinal well-healed surgical scar with a firm palpable mass present on distal anterolateral aspect of the fibula. Her ankle range of motion was full with no limitations on weight-bearing and no neurovascular deficit. Radiograph showed an ossified mass extending from the anterolateral cortex of the fibula. Computed tomography (CT) scan (Fig. 1d) revealed an ossified mass without any corticomedullary continuity, thereby raising suspicion on the primary diagnosis of osteochondroma and magnetic resonance imaging (MRI) was done which revealed a focal mature osteocartilaginous mass arising from the lateral cortex of the fibula which was isointense on T1 with hyperintensity on the surface on T2 scans and a deep heterogeneous areas (Fig. 1e and f). The mass was rebiopsied at our hospital revealing proliferative and irregular osteocartilaginous interface with bizarre nuclei of the chondrocytes suggestive of BPOP (Fig. 1c). All pre-operative investigations were normal. The patient underwent a wide hemicortical excision of the involved fibular cortex with iliac crest bone grafting done to fill the void followed by plating. The final histopathological mass measured 3.1cm×2.2 cm×2 cm (Fig. 2a and b).
The rapid growth caused pain localized to the lateral side of the leg. On examination, she had a linear longitudinal well-healed surgical scar with a firm palpable mass present on distal anterolateral aspect of the fibula. Her ankle range of motion was full with no limitations on weight-bearing and no neurovascular deficit. Radiograph showed an ossified mass extending from the anterolateral cortex of the fibula. Computed tomography (CT) scan (Fig. 1d) revealed an ossified mass without any corticomedullary continuity, thereby raising suspicion on the primary diagnosis of osteochondroma and magnetic resonance imaging (MRI) was done which revealed a focal mature osteocartilaginous mass arising from the lateral cortex of the fibula which was isointense on T1 with hyperintensity on the surface on T2 scans and a deep heterogeneous areas (Fig. 1e and f). The mass was rebiopsied at our hospital revealing proliferative and irregular osteocartilaginous interface with bizarre nuclei of the chondrocytes suggestive of BPOP (Fig. 1c). All pre-operative investigations were normal. The patient underwent a wide hemicortical excision of the involved fibular cortex with iliac crest bone grafting done to fill the void followed by plating. The final histopathological mass measured 3.1cm×2.2 cm×2 cm (Fig. 2a and b). 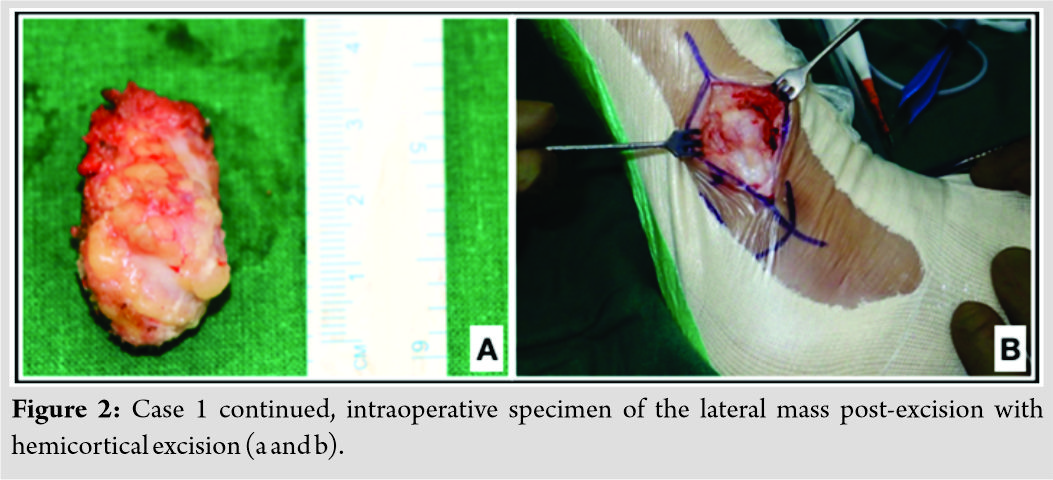 No complications were seen postoperatively with the patient being recurrence and pain free at the last follow-up of 6 years (Fig. 3).
No complications were seen postoperatively with the patient being recurrence and pain free at the last follow-up of 6 years (Fig. 3).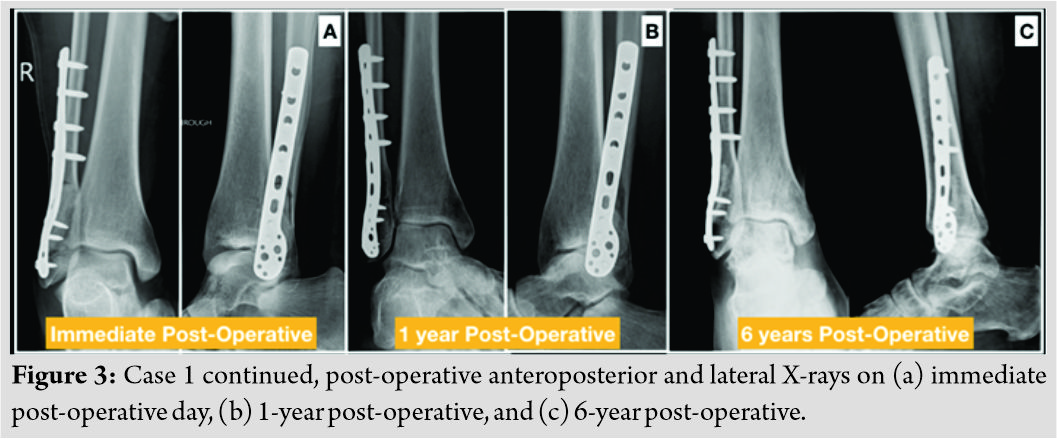
Case 2
A 21-year-old male presented with a recurrent swelling of the left little finger for 4 months. He had undergone an excision biopsy at the same site 18 months ago in another institute. The biopsy slide reported outside as osteoma was reviewed and found to be BPOP. The patient gave no history of pain or trauma preceding the swelling. On examination (Fig. 4d), a firm, immobile, non-tender discreet swelling was felt on the anterolateral aspect of proximal phalanx of the left little finger. The overlying skin was free and showed scar of the previous surgery. There was no limitation of finger movement. All pre-operative investigations were normal. X-rays showed two bony projections in the proximal phalanx of the left little finger (Fig. 4a). The distal projection seemed to arise from the periosteum while the proximal lesion appeared separate from it. No periosteal or cortical thickening was seen with differential of periosteal osteogenic sarcoma(OGS)and BPOP in mind.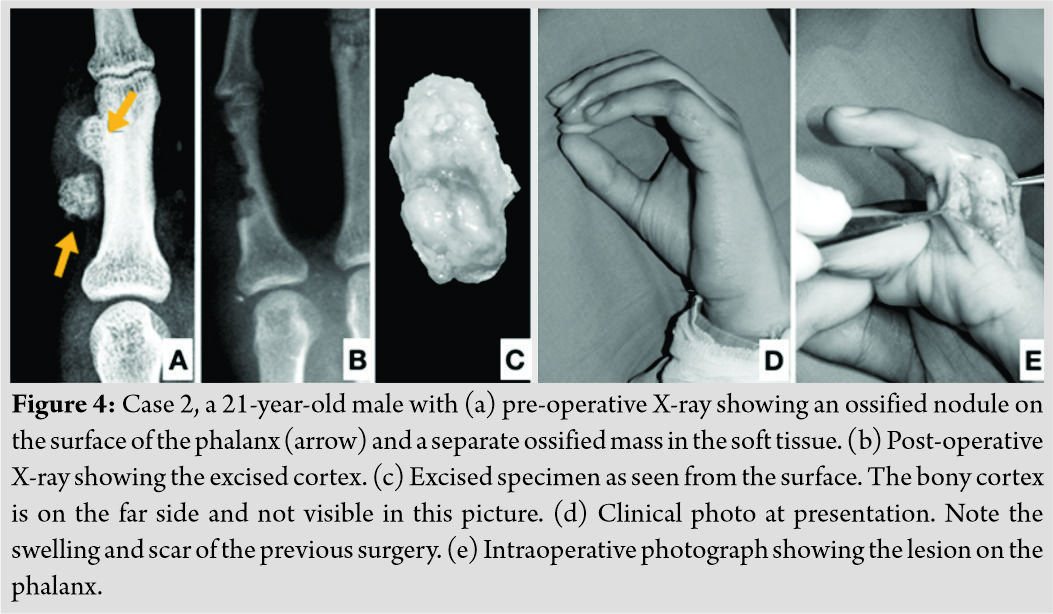
The patient was operated with wide excision of the involved cortex with no apparent corticomedullary continuity with the mass (Fig. 4b, c and e). The interphalangeal joint was not found to be involved. Post-operative stay was uneventful with the patient regaining full range of motion of finger at all joints with no pain or recurrence at subsequent follow-ups.
Case 3
A 31-year-old male presented to the hospital with slow-growing swelling in the left proximal tibia for 7–8 years. The patient gave a history of fall 1–2 months before presentation and was unable to bear weight on the affected limb. On examination, a large mass was palpable arising from the proximal tibia extending posteriorly, laterally, and superiorly across the knee joint. Popliteal pulsation could not be felt, but dorsalis pedis was palpable and the patient had no neurological deficit. The patient had a fixed flexion deformity of 60° with no further range of motion possible at the knee joint. The X-ray showed large calcific lesion arising from the upper end of tibia and likely from fibula (Fig. 5a and b). The calcification was chunky and irregular in nature and appeared to be a secondary sarcomatous change in a case of long existing osteochondroma. The MRI suggested of an irregular osteochondromatous lesion extending toward the posterior neuromuscular bundle but not invading it (Fig. 5c and d). All pre-operative investigations were normal and a decision was taken to widely resect this tumor and implant a proximal tibia replacement megaprosthesis to allow limb salvage. A gross 13 cm long proximal tibial segment was resected and sent for intraoperative histological analysis. The tumor was lobulated with a cartilaginous cap and measured 10 cm×9cm×6 cm (Fig. 5e and f). 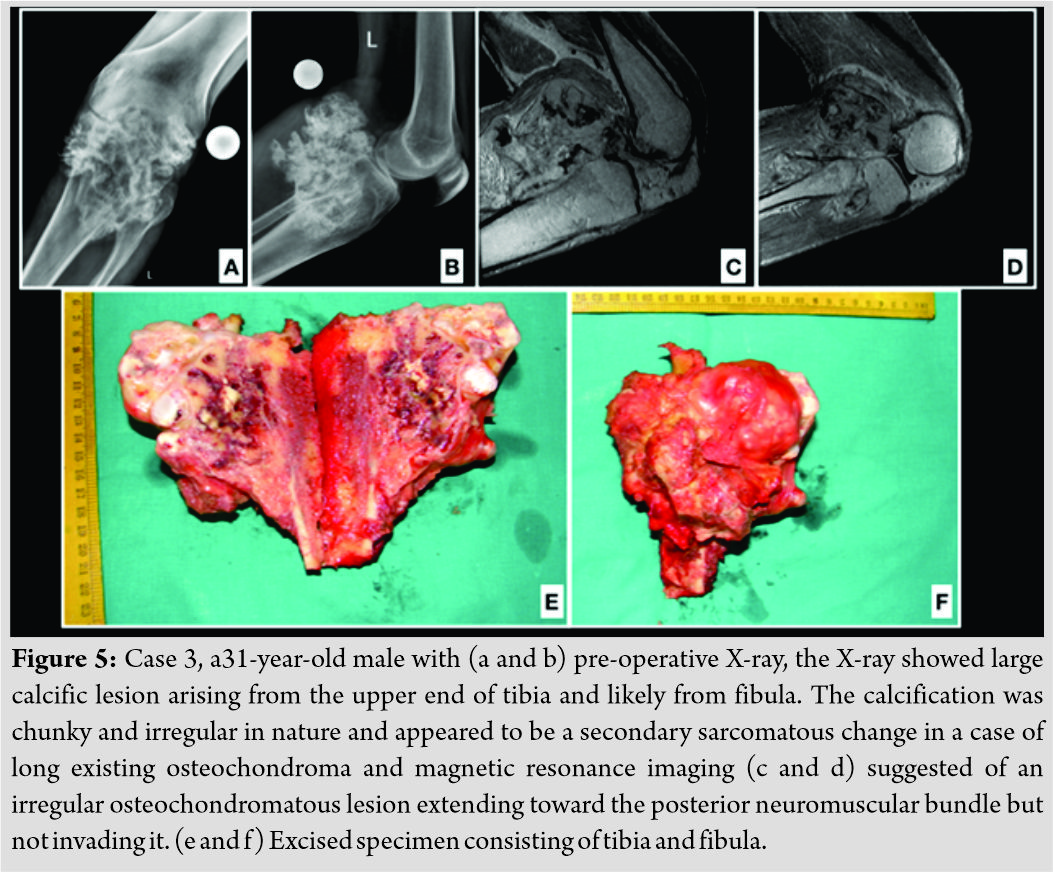 The tumor had eroded the posterior cortical margins. Also resected was a 4cm stump of proximal fibula which showed involvement intraoperatively. The histopathology revealed irregular mass of bony trabeculae with island of hyaline cartilage with extensive enchondral ossification. The newly ossified bone showed characteristic blue coloration in the intratrabecular space with no atypical cellular proliferation, thus confirming the diagnosis of BPOP. On regular post-operative follow-up, the patient recovered good quadriceps and hamstrings strength with knee range also recovering between 0 and 90°. No signs of recurrence were seen on a 7-year follow-up (Fig. 6.)
The tumor had eroded the posterior cortical margins. Also resected was a 4cm stump of proximal fibula which showed involvement intraoperatively. The histopathology revealed irregular mass of bony trabeculae with island of hyaline cartilage with extensive enchondral ossification. The newly ossified bone showed characteristic blue coloration in the intratrabecular space with no atypical cellular proliferation, thus confirming the diagnosis of BPOP. On regular post-operative follow-up, the patient recovered good quadriceps and hamstrings strength with knee range also recovering between 0 and 90°. No signs of recurrence were seen on a 7-year follow-up (Fig. 6.)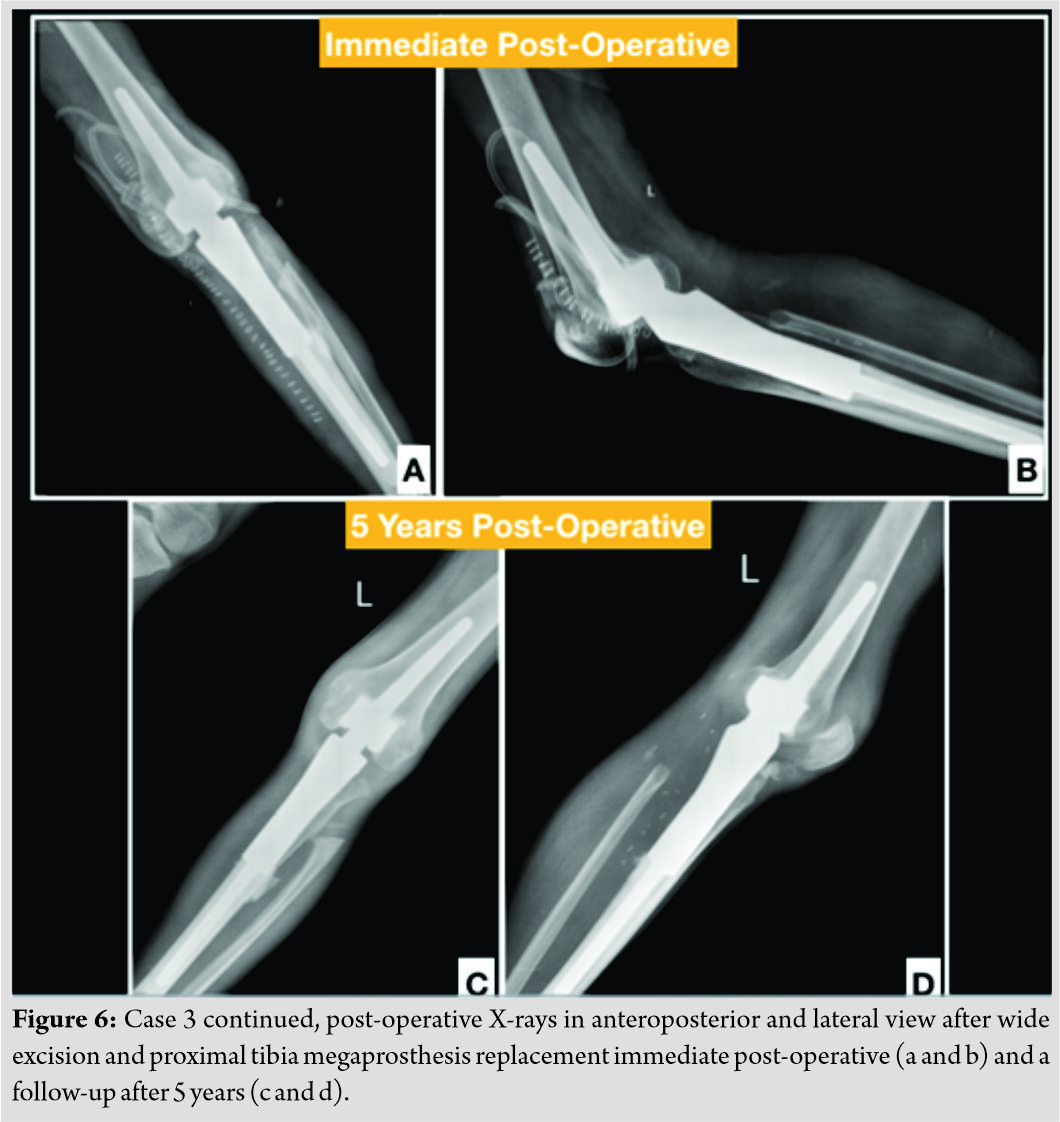
Case 4
A 26-year-old male came to the hospital with swelling of his right lateral end clavicle region for the past 6 years with an increase in size over the past 6 months. There was no history of trauma or surgery. On examination, the swelling was 6cm×7 cm, bony hard in consistency, non-tender, and localized over the lateral end of clavicle, anteriorly and posteriorly. No neurovascular deficit was associated with the mass. On X-ray (Fig. 7a and b), there was a large, irregular osseous mass arising from distal end of clavicle extending anteriorly, posteriorly, and inferiorly. Acromion and acromioclavicular shoulder joint were spared. CT scan confirmed the mass to be adherent to the periosteum with scalloping of the involved cortex. However, no corticomedullary continuity was seen. MRI suggested a mass arising from the inferior aspect of distal end of clavicle measuring 9.4cm×8.2 cm in axial and 7.7 cm in superoinferior dimensions. The mass extended superiorly, inferiorly, and posteriorly causing inferomedial displacement of infraclavicular portion of brachial plexus and axillary vessels without involving them. We suspected an osteochondroma with secondary chondromatous change with a differential of BPOP in mind. The patient underwent a planned excision of lateral end of clavicle with wide margins (Fig. 7c). Histopathology confirmed the tumor to be BPOP. Postoperatively, no recurrence was seen with the patient having full function of the limb (Fig. 7d).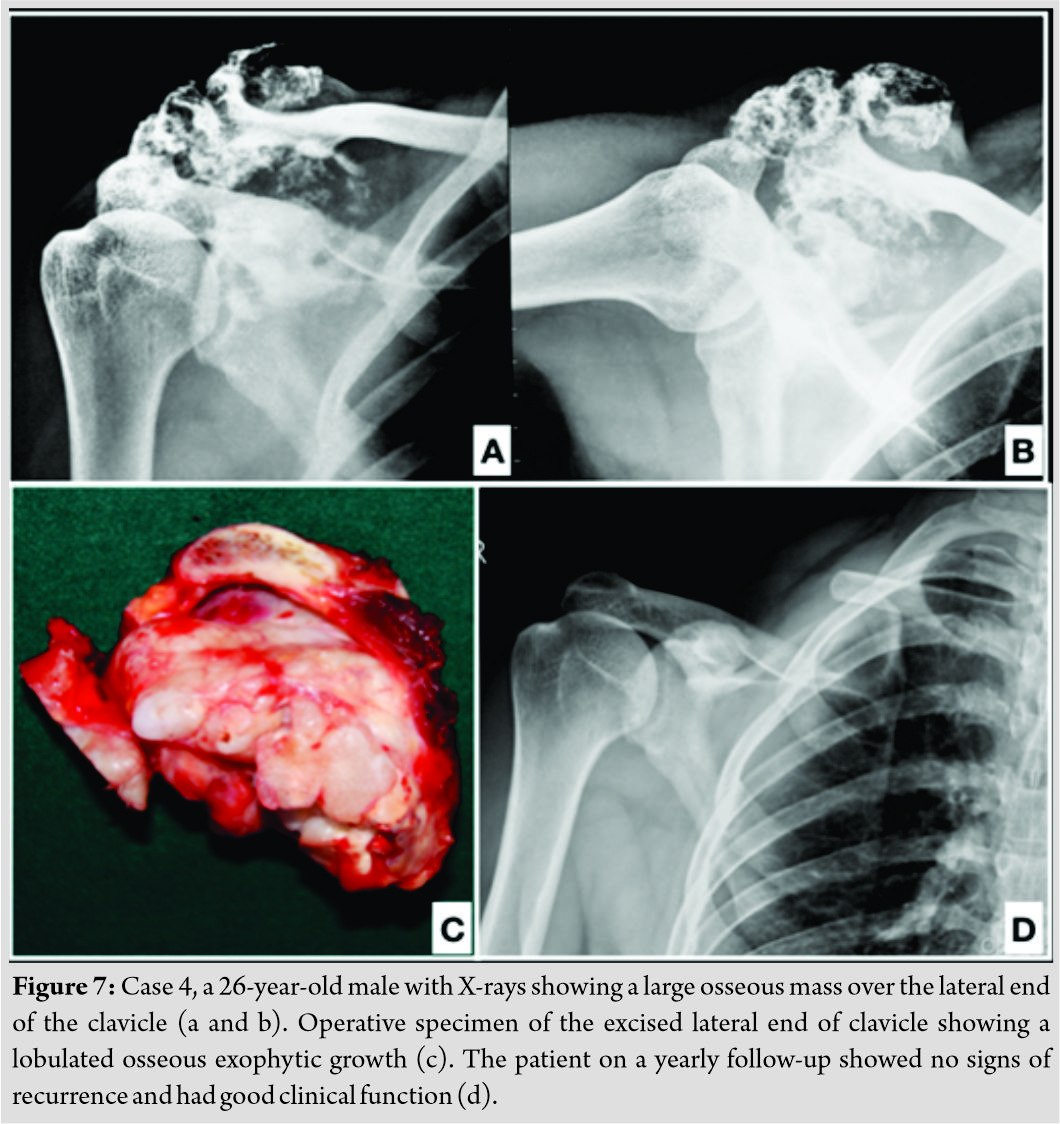
Case 5(lost to follow-up)
A 36-year-old female came with recurrent swelling of base of the 4th metatarsal for which she had undergone curettage at a local hospital (Fig. 8). The lesion was suspected to be an osteochondroma but recurred within 6 months of excision. Slides were reviewed by our histopathology department and the case was confirmed to be BPOP on histology. The patient, however, refused to undergo wide excision and was lost to follow up.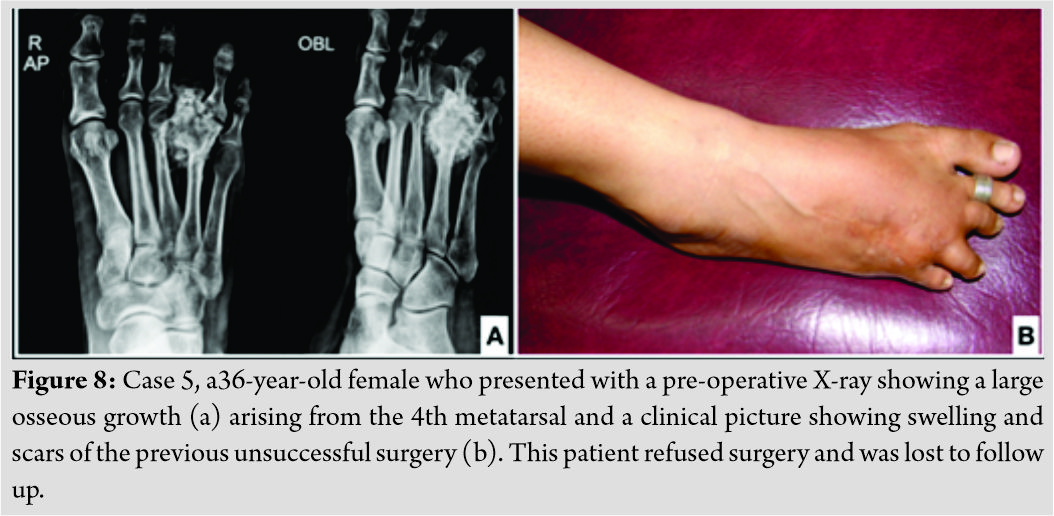
Discussion
BPOP is a rare benign but locally aggressive lesions characteristically arising from the cortex of the underlying bone without invading the involved cortex. BPOP was originally described by Nora et al., in 1983, in small bones of hands and feet [1], but all long bones can be involved as described by Meneses et al., in 1983, and further updated in 1993 [6]. Nora distinguished these lesions from reactive periosteal lesions described by Spjut and Dorfman, in 1981 [7]. Dorfman also suggested BPOP to be a part of reactive lesion seen in different phases of maturation – florid reactive periostitis, BPOP, and finally turrets exostosis. However, an inconsistent history of trauma as an inciting event also supported by the absence of trauma in four out of five of our cases disputes this theory. Zambrano et al. [8] also disputed this theory and considered BPOP to be a neoplastic entity. Subsequently, Nilsson et al. [9] and Endo et al. [10] found and suggested t(1;17) (q32;q21) as a separate translocation unique to BPOP. None of our patients had undergone cytogenetic study; thus, no comment can be made on such an association. Furthermore, if BPOP is a reactive entity, another explanation is warranted for the remarkable recurrence rate in each study. In 2001, Horiguchi et al. [5] identified a process in BPOP similar to normal enchondral ossification growth plate showing a reactive process after injury. This process was the expression of basic fibroblastic growth factor in all chondrocytes. BPOP most commonly mimic an osteochondroma due to their bony matrix capped with cartilage. However, several radiological and histological differences are apparent. In BPOP, there is a marked proliferation of cartilage cap with an irregular bone cartilage interface. Three components characterize BPOP: Cartilage cap with highly cellular bizarre binucleate chondrocytes without any cellular or cytological atypia [6]; callus-like maturation of bone cartilage junction [1]; andabundant benign-appearing osteocytes with spindle cells in bony trabeculae [1, 6]. The bony trabeculae have a characteristic blue coloration with hematoxylin and eosin stain with loose arrangement of spindle cells. The osteochondromas in contrast have a parallel chondrocyte arrangement which is more streamlined in lacunar spaces [11]. The typical radiological finding of BPOP is a heterogeneous well-marginated ossified mass arising from the cortical surface of the bone without periosteal reaction or flaring of underlying cortex which is contrary to the corticomedullary continuity seen in cases of osteochondroma. However, in atypical cases, as shown by Rybak et al. [12], corticomedullary continuity on imaging was proven to be BPOP on pathology, thus questioning the role of imaging alone in identifying BPOP. Although none of our patients showed any corticomedullary continuity, we do not believe that radiology alone is sufficient to diagnose BPOP and that a comprehensive radiological study with cross-sectional imaging (MRI with low-intensity signals on T1 and high-moderate signal intensity on T2) of the lesion with histological confirmation is confirmatory. BPOP must also be differentiated from myositis ossificans (mature ossification without cartilaginous cap), parosteal OGS (invades local tissue and shows fibrous atypia), periosteal chondroma (exhibits saucerization of the underlying cortex), or reactive periostitis (similar histology to BPOP without the cartilaginous proliferation). As per our cases, the typical radiological diagnostic features to raise a possibility of BPOP should be: An ossified mass arising out of the cortex without any corticomedullary continuity on CT scan; an MRI should suggest a focal mature osteocartilaginous mass arising from the cortex which is isointense on T1 images with hyperintensity on the surface of T2 scans with deep heterogeneous areas (as classically seen on 1E and 1F). Such imaging findings must be biopsied for confirmation and histopathology must show the following features: Proliferative and irregular osteocartilaginous interface with bizarre nuclei of the chondrocytes; irregular mass of bony trabeculae with island of hyaline cartilage with extensive enchondral ossification; and newly ossified bone showed characteristic blue coloration in the intratrabecular space with no atypical cellular proliferation. Treatment of BPOP requires wide excision of the involved cortex along with the tumor with intraoperative frozen section confirming negative margins to prevent recurrence. Reconstruction depends on the extent of tumor spread as extensive spread may require a complete resection (as shown in our case 3 and 4) and reconstruction with a megaprosthesis (case 3). No compromise should be made on the margins of the tumor due to a high recurrence rate (as high as 51% reported by Nora et al. [1] and a second recurrence of 22% within 2 years of excision). Resection must include complete resection of pseudocapsule, periosteum, and decortication of underling host bone.
Conclusion
BPOP is a diagnostic challenge and is commonly misdiagnosed on radiology and histopathology. In all of our cases, both radiologists and pathologists have misdiagnosed BPOP, thereby advocating a high index of suspicion with typical and atypical presentations. We strongly recommend a wide (enbloc) excision and removal of the involved cortex, periosteum, and pseudocapsule with negative disease-free margins to be determined intraoperatively. This recommendation is based on a regular follow-up of all our cases (upto 7 years) with no recurrences. Proper pre-operative planning for the execution of reconstruction of bone and ligaments is must to provide normal limb and joint function.
Clinical Message
BPOP is a distinct entity commonly misdiagnosed by radiologists, pathologists, and orthopedicians alike. Keeping a high index of suspicion in a recurring osteochondroma and observing the basic diagnostic sequence of imaging, namely, X-ray, CT scan, and MRI would help in avoiding morbidity associated with recurrences.
References
1. Nora FE, Dahlin DC, Beabout JW. Bizarre parostealosteochondromatousproliferations of the hands and feet. Am J Surg Pathol1983;7:245-50.
2. Dhondt E, Oudenhoven L, Khan S, Kroon HM, Hogendoorn PC, Nieborg A, et al. Nora’s lesion, a distinct radiological entity? Skeletal Radiol2006;35:497-502.
3. Torreggiani WC, Munk PL, Al-Ismail K, O’Connell JX, Nicolaou S, Lee MJ, et al. MR imaging features of bizarre parostealosteochondromatous proliferation of bone (Nora’s lesion). Eur J Radiol2001;40:224-31.
4. Abramovici L, Steiner GC. Bizarre parostealosteochondromatousproliferation (Nora’s lesion): A retrospective study of 12 cases, 2 arising in long bones. Hum Pathol2002;33:1205-10.
5. Horiguchi H, Sakane M, Matsui M, Wadano Y. Bizarre parostealosteochondromatous proliferation (Nora’s lesion) of the foot. Pathol Int 2001;51:816-23.
6. Meneses MF, Unni KK, Swee RG. Bizarre parostealosteochondromatous proliferation of bone (Nora’s lesion). Am J Surg Pathol1993;17:691-7.
7. Spjut HJ, Dorfman HD. Florid reactive periostitis of the tubular bones of the hands and feet. A benign lesion which may simulate osteosarcoma. Am J Surg Pathol1981;5:423-33.
8. Zambrano E, Nosé V, Perez-Atayde AR, Gebhardt M, Hresko MT, Kleinman P, et al. Distinct chromosomal rearrangements in subungual (Dupuytren) exostosis and bizarre parostealosteochondromatous proliferation (Nora lesion). Am J Surg Pathol2004;28:1033-9.
9. Nilsson M, Domanski HA, Mertens F, Mandahl N. Molecular cytogenetic characterization of recurrent translocation breakpoints in bizarre parostealosteochondromatous proliferation (Nora’s lesion). Hum Pathol2004;35:1063-9.
10. Endo M, Hasegawa T, Tashiro T, Yamaguchi U, Morimoto Y, Nakatani F, et al. Bizarre parostealosteochondromatous proliferation with a t(1;17) translocation. Virchows Arch 2005;447:99-102.
11. Dahlin DC, Unni KK. Bone Tumors: General Aspects and Data on 8,547 Cases. 4th ed. United States: Charles C Thomas Publisher; 1986.
12. Rybak LD, Abramovici L, Kenan S, Posner MA, Bonar F, Steiner GC. Cortico-medullary continuity in bizarre parostealosteochondromatous proliferation mimicking osteochondroma on imaging. Skeletal Radiol2007;36:829-34.
 |
 |
 |
 |
 |
| Dr. Supreet N Bajwa | Dr. Rajeev Reddy | Dr. Yash S Wagh | Dr. Manish Agarwal | Dr. Ameya Katariya |
| How to Cite This Article: Bajwa S N, Reddy R, Wagh Y S, Agarwal M, Katariya A. Bizarre Parosteal Osteochondromatous Proliferation– A Case Series of Typical and Atypical Presentations. Journal of Orthopaedic Case Reports 2020 Jan-Feb;10(1): 45-50. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com







