[box type=”bio”] Learning Point of the Article: [/box]
Delta wiring technique for mallet finger fractures is safe and reliable method as compared to other methods as delta wiring method does not involve any trans articular pins.
Case Report | Volume 10 | Issue 1 | JOCR January – February 2020 | Page 98-101 | Bipul K Garg, Gaurav B Waghmare, Shravan Singh, Kishor B Jadhav. DOI: 10.13107/jocr.2020.v10.i01.1656
Authors: Bipul K Garg[1], Gaurav B Waghmare[1], Shravan Singh[1], Kishor B Jadhav[1]
[1]Department of Orthopaedic Surgery, Sir J. J. Group of Hospitals and Grant Medical College, Mumbai, Maharashtra, India.
Address of Correspondence:
Dr. Bipul K Garg,
Department of Orthopaedic Surgery, Sir J. J. Group of Hospitals and Grant Medical College, Mumbai, Maharashtra, India.
E-mail: garg.bipul@gmail.com
Abstract
Introduction: Extension-block pinning is a popular surgical treatment method for mallet fractures but is associated with several pitfalls. Transfixation Kirschner wires used in the extension-block pinning technique may cause iatrogenic nail bed injury, bone fragment rotation, chondral damage, or osteoarthritis. The objective of this study was to determine the result of the delta wiring technique in a case of mallet finger with fracture fragment involving more than one-third of the distal phalanx articular surface. This is the first reported case of mallet fracture treated with delta wiring in literature.
Case Report: A 30-year-old male patient admitted in our institute with complaints of severe pain in the right index finger with inability to extend the distal interphalangeal joint (DIP) for 5 days. There was a history of fall from the bike before this complaint. Radiographs revealed a bony mallet fracture involving more than one-third of the articular surface of distal phalanx. The patient was taken up for delta wiring fixation of the fracture. Radiographic bony union was seen at 7 weeks. At the final follow-up at 1 year, DIP had 75° of flexion and had extension deficit of 5°. According to Crawford’s criteria, the patient had good results with a VAS score of 1 with no pain.
Conclusion: Delta wiring technique is a new and safe treatment modality for bony mallet fracture with fracture fragment involving more than one-third of the distal phalanx articular surface as satisfactory clinical and radiological outcomes obtained in our case.
Keywords: Bony mallet finger, extension-block pinning, delta wiring, transfixation pin.
Introduction
A mallet fracture involves damage to the terminal extensor mechanism caused by bony avulsion of the distal phalanx base. Such fractures typically result from forced flexion of the extended distal interphalangeal joint (DIP) [1]. Although several treatment options have been reported, from conservative to surgical management, the optimal treatment continues to be a subject of debate [2]. However, surgery is usually advocated when the dorsal fragment involves more than one-third of the articular surface or when there is volar subluxation [3]. The main surgical options are Kirschner wire fixation [4], tension band wiring [5], microscrews [6], pull-out wire fixation [7], hook plate [8], small external fixator [2], or extension-block fixation [3,9]. The extension-block pinning technique reported by Ishiguro et al. [9] is among the most popular treatment methods for mallet fractures but is associated with several potential problems. Transfixation Kirschner wires used to fix the DIP joint may cause iatrogenic nail bed injury, bone fragment rotation, chondral damage, or osteoarthritis. Furthermore, the need for prolonged immobilization may cause flexion contracture of the DIP joint. Procedure described in this case is simple and minimally invasive technique reported by Kim [10], for the management of mallet fractures, which can permit early joint motion and give strong compression force on the fracture fragment continuously. Delta wiring technique had not been studied extensively in literature, and to our knowledge, this is the first reported case in literature.
Case Report
A 30-year-old male admitted in our institute with complaints of severe pain in the right index finger with inability to extend the DIP joint for 5 days. There was a history of fall from the bike before this complaint. Radiographs revealed a bony mallet fracture at the distal phalanx, with fracture fragment involving more than one-third of distal phalanx articular surface. The patient was then planned for delta wiring fixation of the fracture. The procedure was performed using an image intensifier under digital block anesthesia without a tourniquet.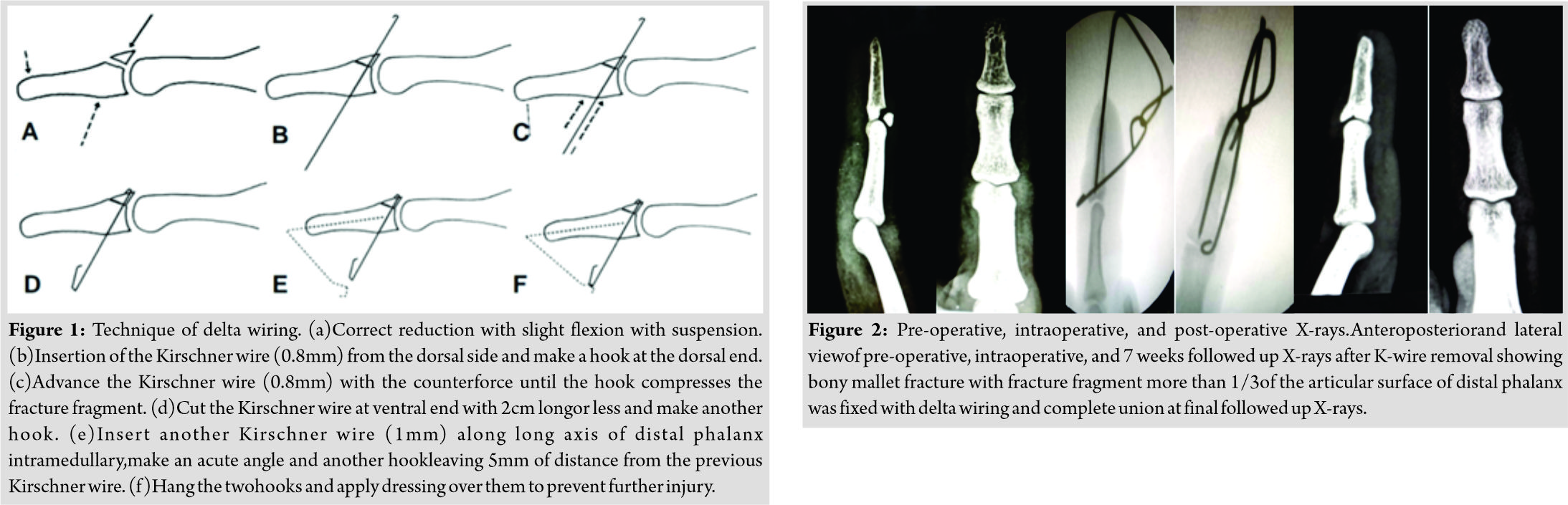 Appropriate reduction is confirmed on lateral X-ray with slight flexion with suspension. Insert a Kirschner wire 0.8 mm through the bony fracture fragment attached with extensor tendon from the dorsal side and make a hook on dorsal end of Kirschner wire and advance the Kirschner wire through the distal phalanx with counter force. Cut the Kirschner wire saving 2 cm length at plantar end which is now come out from the skin of plantar side penetrated through the fracture fragment, distal phalanx and make another hook. Insert another Kirschner wire 1 mm along the long axis of distal phalanx intrameduallry.
Appropriate reduction is confirmed on lateral X-ray with slight flexion with suspension. Insert a Kirschner wire 0.8 mm through the bony fracture fragment attached with extensor tendon from the dorsal side and make a hook on dorsal end of Kirschner wire and advance the Kirschner wire through the distal phalanx with counter force. Cut the Kirschner wire saving 2 cm length at plantar end which is now come out from the skin of plantar side penetrated through the fracture fragment, distal phalanx and make another hook. Insert another Kirschner wire 1 mm along the long axis of distal phalanx intrameduallry.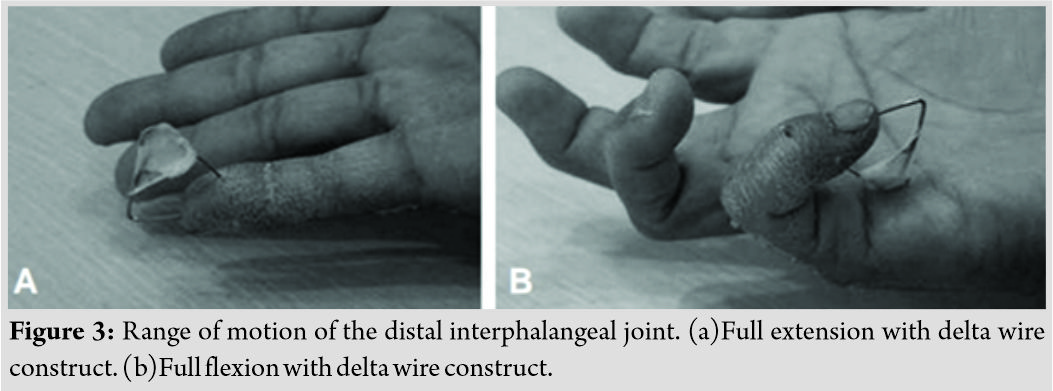 Make an acute angle and another hook leaving 5mm of distance from the previous Kirschner wire. Hang the two hooks and apply dressing over them to prevent further injury (Fig.1a-f), allowing the DIP joint to have free movement. The patient’s was discharged on the day of surgery and requested to return for weekly review. After clinical and radiological confirmation of union around 7 weeks, the Kirschner wires were removed. For removal, the first step is to untie the hook, then axial intramedullary wire pulled out easily, then the first wire was just push back slight dorsally, and the hook was cut, then from plantar side the first wire pulled out. Lateral and posteroanterior plain radiographs were taken pre-operative, intraoperative, and weekly postoperatively (Fig. 2). Active range of motion exercises was initiated immediately after the operation (Fig.3aand b). Fracture union was defined as the X-ray presence of bridging trabeculae and a radiolucent line at the fracture gap and the clinical absence of tenderness at the fracture site. The active range of motion and extension lag of the DIP joint were measured with a goniometer. Full flexion was considered as achieved when the angle of the injured side reached that of the opposite side at follow-up. Functional outcomes were evaluated using Crawford’s criteria (Table 1). At 1 year, the DIP had flexion of 75° and had extension deficit of 5°. According to Crawford’s criteria, the patient had good result. The patient does not have pain at the final follow-up with a VAS score of 1.There were no complications, such as comminution of the fracture fragment, nail deformity, volar subluxation, or dislocation of the DIP joint osteoarthritis.
Make an acute angle and another hook leaving 5mm of distance from the previous Kirschner wire. Hang the two hooks and apply dressing over them to prevent further injury (Fig.1a-f), allowing the DIP joint to have free movement. The patient’s was discharged on the day of surgery and requested to return for weekly review. After clinical and radiological confirmation of union around 7 weeks, the Kirschner wires were removed. For removal, the first step is to untie the hook, then axial intramedullary wire pulled out easily, then the first wire was just push back slight dorsally, and the hook was cut, then from plantar side the first wire pulled out. Lateral and posteroanterior plain radiographs were taken pre-operative, intraoperative, and weekly postoperatively (Fig. 2). Active range of motion exercises was initiated immediately after the operation (Fig.3aand b). Fracture union was defined as the X-ray presence of bridging trabeculae and a radiolucent line at the fracture gap and the clinical absence of tenderness at the fracture site. The active range of motion and extension lag of the DIP joint were measured with a goniometer. Full flexion was considered as achieved when the angle of the injured side reached that of the opposite side at follow-up. Functional outcomes were evaluated using Crawford’s criteria (Table 1). At 1 year, the DIP had flexion of 75° and had extension deficit of 5°. According to Crawford’s criteria, the patient had good result. The patient does not have pain at the final follow-up with a VAS score of 1.There were no complications, such as comminution of the fracture fragment, nail deformity, volar subluxation, or dislocation of the DIP joint osteoarthritis.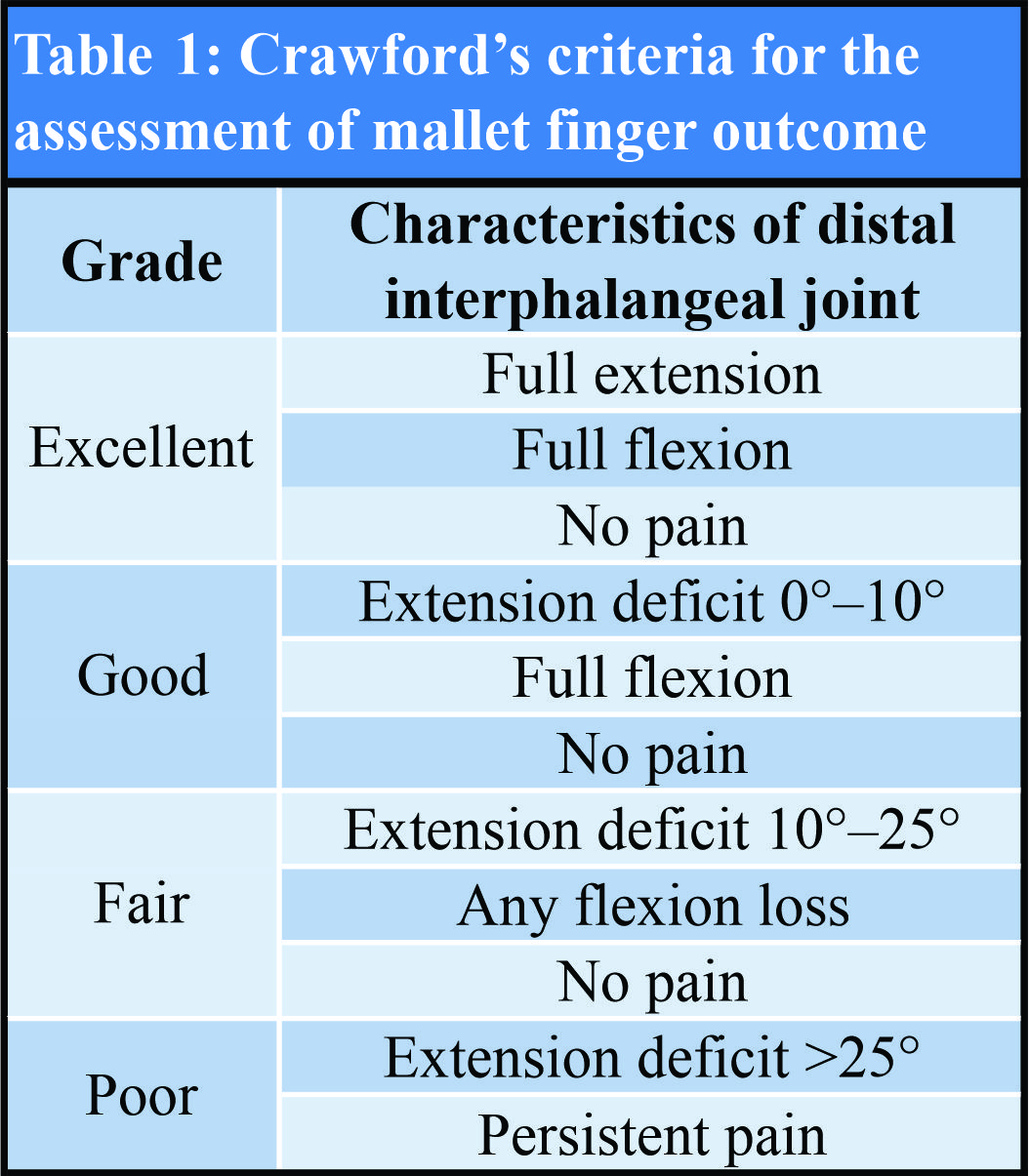
Discussion
There is no optimal treatment for mallet finger injuries; there is a range of potential treatments that are considered appropriate [11]. Ishiguro et al. [9] first described extension-block pinning as a simple and reliable method, and it has since become one of the most popular methods of treating mallet finger, with later modifications [10]. Most of these techniques involve the use of Kirschner wire fixation across the DIP, despite awareness that it is difficult to insert a temporary transfixation pin through the DIP. Potential disadvantages associated with repeated attempts during insertion include articular cartilage damage that can lead to the secondary osteoarthritis, especially if more than one attempt during pin insertion is needed [3] and iatrogenic nail bed injury. However, the delta wiring technique [10] did not require that a transfixation pin is inserted through the joint, which should reasonably be expected to decrease the risk of secondary arthritis. Miura [2] described a modified version of the extension-block fixation method that was designed to achieve accurate reduction and stable fixation by controlling dorsal rotation of the fragment with an external fixator. Twelve acute mallet fractures were treated with this method and not only were all united after an average of 5±1 weeks but also there were no arthritic changes after an average follow-up of 4 months. However, that design required a bulky fixator and a DIP splint for an average of 6 weeks. It also required a second surgical procedure to remove the fixator. Miranda et al. [12] described a simple technique to improve intraoperative bony mallet reduction and avoid complications such as articular cartilage damage, nail bed damage, and dorsal skin necrosis. They used a blunt needle as a joystick to reduce the bony fragment of a stab incision. After reduction was achieved, a dorsal splint was applied holding the DIP joint in 15°–30° extension. They achieved and maintained satisfactory reduction and reported their technique as a less invasive management option for bony mallet fractures. Criticism of this technique focused on the difficulty of maintaining the reduction of the unstable fragment with the dorsal splint alone due to the strong extensor tendon pulling force on the bony fragment [13]. Karslıoğluet al. [14] emphasized that rotation of the mallet fragment can prevent appropriate fracture reduction and may result in extension lag, incongruity of the articular surface, premature osteoarthritis, or stiffness. They described a percutaneous derotation technique utilizing needle tip reduction during surgery for Type II b and III c patients according to the Wehbe and Schneider classification [15]. They found that derotation of Type II (25% rotation) and III (50% rotation) mallet fractures with closed reduction was simple and could prevent surgical failure [14]. Closed reduction by extension-block Kirschner wire fixation and also by delta wiring is a relative contraindication in bony mallet fractures older than 5 weeks. Reduction may not be achieved due to scar tissue that prevents closed reduction in these fractures [9]. Open reduction to restore the congruity of the articular surface is indicated in such cases [11]. Pegoli et al. [3] used percutaneous curettage with an Ishiguro extension-block Kirschner wire technique to treat mallet fracture cases older than 5 weeks. Further, research will be essential to assess the efficacy of this approach with fracture fragments that involve <1/3 of the articular surface. Finally, the follow-up period is also too short to observe long-term adverse outcomes.
Conclusion
Our technique reduces the risks of iatrogenic chondral injury, joint degeneration, nail bed injury, as well as fracture displacement due to continuous compression on the fracture fragment. Delta wiring technique may, therefore, be a useful alternative method for the treatment of mallet fractures, benefiting from being less invasive and easy to perform.
Clinical Message
Decision-making for the management of delta fractures can be challenging. Multiple techniques have been described in literature, but each and every technique has many pitfalls such as secondary osteoarthritis and chondral damage. Delta wiring technique did not have those complications as in this technique no need of transarticular pins.
References
1. Doyle J. Extensor tendons: Acute injuries. In: Green DP, Hotchkiss RN, Pederson WC, editors. Operative Hand Surgery. 4th ed. Philadelphia, PA: Churchill Livingstone; 1999. p. 1950-70.
2. MiuraT. Extension block pinning using a small external fixator for mallet finger fractures.J Hand Surg Am2013;38:2348-52.
3. PegoliL, TohS, AraiK, FukudaA, NishikawaS, VallejoIG. The ishiguro extension block technique for the treatment of mallet finger fracture: Indications and clinical results.J Hand Surg Br2003;28:15-7.
4. LubahnJD. Mallet finger fractures: A comparison of open and closed technique.J Hand Surg Am1989;14:394-6.
5. DamronTA, EngberWD. Surgical treatment of mallet finger fractures by tension band technique.Clin OrthopRelat Res1994;300:133-40.
6. KronlageSC, FaustD. Open reduction and screw fixation of mallet fractures.J Hand Surg Br2004;29:135-8.
7. ZhangX, MengH, ShaoX, WenS, ZhuH, MiX. Pull-out wire fixation for acute mallet finger fractures with k-wire stabilization of the distal interphalangeal joint.J Hand Surg Am2010;35:1864-9.
8. TeohLC, LeeJY. Mallet fractures: A novel approach to internal fixation using a hook plate.J Hand Surg Eur Vol2007;32:24-30.
9. IshiguroT, ItohY, YabeY, HashizumeN. Extension block with kirschner wire for fracture dislocation of the distal interphalangeal joint.Tech Hand Up Extrem Surg1997;1:95-102.
10. Kim JH, Kim JH, Lee S, Kim DG. “Delta (delta) wire technique” for bony mallet finger: Surgical technique. J Korean Orthop Res Soc 2013;16:13-6.
11. LinJS, SamoraJB. Surgical and nonsurgical management of mallet finger: A systematic review.J Hand Surg Am2018;43:146-63.
12. MirandaBH, MurugesanL, GrobbelaarAO, JemecB. PBNR: Percutaneous blunt needle reduction of bony mallet injuries.Tech Hand Up Extrem Surg2015;19:81-3.
13. KarsliogluB, TekinAC, TasatanE. Percutaneous blunt needle reduction (PBNR) needs stable fixation.Tech Hand Up Extrem Surg2018;22:35-6.
14. KarslıoğluB, UzunM, TetikC, TasatanE, TekinAC, BuyukkurtCD. Derotation of the mallet piece: A crucial point in mallet fracture surgery.Hand Surg Rehabil2018;Volume 37, Issue 4, July 2018, Pages 202-205:S2468-1229.
15. WehbéMA, SchneiderLH. Mallet fractures.J Bone Joint Surg Am1984;66:658-69.
 |
 |
 |
 |
| Dr. Bipul K Garg | Dr. Gaurav B Waghmare | Dr. Shravan Singh | Dr. Kishor B Jadhav |
| How to Cite This Article: Garg BK, Waghmare GB, Singh S, Jadhav KB. Mallet Finger Fracture Treated with Delta Wiring Technique: A Case Report of a New Fixation Technique. Journal of Orthopaedic Case Reports 2020 Jan-Feb;10(1): 98-101. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com




