[box type=”bio”] Learning Point of the Article: [/box]
Non-union and implant failure are recognized features of AFFs and may necessitate revision surgery to achieve a successful union. Exchange k-nailing and augmented plating technique can be performed successfully along with bone grafting for treating diaphyseal AFF non-union.
Case Report | Volume 10 | Issue 3 | JOCR May – June 2020 | Page 5-9 | Vivek M. Sodhai, Chetan V. Pradhan, Ashok K. Shyam1. DOI: 10.13107/jocr.2020.v10.i03.1724
Authors: Vivek M. Sodhai[1], Chetan V. Pradhan[1], Ashok K. Shyam[1],[2]
[1]Department of Trauma, Sancheti Institute for Orthopaedics and Rehabilitation, Pune, Maharashtra. India,
[2]Indian Orthopaedic Research Group, Thane, Maharashtra, India.
Address of Correspondence:
Dr. Vivek M. Sodhai,
Department of Trauma, Sancheti Institute for Orthopaedics and Rehabilitation,16, Shivaji Nagar, Pune – 411005, Maharashtra, India.
E-mail: vivek.sodhai89@gmail.com
Abstract
Introduction: Atypical femoral fractures (AFFs) have an unpredictable healing process leading to higher complication rates. The literature describes various treatment modalities of non-unions in AFF. We aimed to report a case of non-union with AFF and successful union with exchange K-nailing and augmented plating techniques.
Case Report: A 75-year-old lady with 5 years of bisphosphonate intake sustained an AFF at the mid-diaphyseal level after a trivial injury which was fixed with closed intramedullary nailing. Nine months after fixation, she developed refracture at the fracture site with segmental breakage of the nail suggesting non-union. This was managed by the removal of fibrous structures at the fracture site, removal of a broken nail, exchange K-nailing, augmented plating, and iliac crest bone grafting. The fracture healed at 15 months from the injury and achieved good functional outcome at a short-term follow-up of 1 year.
Conclusion: Our case report highlights the challenges of treating diaphyseal AFF and the combined benefit of exchange nailing and augmented plating with bone grafting in treating AFFs with non-union.
Keywords: Atypical femoral fractures, non-union, implant failure, exchange nailing, augmented plating.
Introduction
There is no exact pathogenic mechanism regarding the development of atypical femoral fractures (AFFs) [1]; however, studies suggest osteoporosis, prolonged bisphosphonates (BP) treatment, excessive anterolateral femoral curvature, and increased cortical thickening as independent risk factors for AFFs [2]. Diagnostic criteria for AFFs were given by the Task Force of the American Society for Bone and Mineral Research (ASBMR) in 2010 and updated in 2013 [3], includes major and minor criteria. Patients with AFFs have a higher incidence of delayed fracture healing as compared to typical femoral fractures at subtrochanteric or diaphyseal levels [4], which can be attributed to decreased bone turnover secondary to prolonged BP treatment [5]. Due to this unpredictable fracture healing, cases of non-union and implant failures in AFFs are being reported frequently. Lovy et al. reported the use of bone marrow aspirate concentrate and demineralized bone matrix injections at fracture sites to avoid delayed union and non-union [6]. Yeh et al. demonstrated the use of teriparatide medications in patients with subtrochanteric AFFs for fracture healing, hip function recovery, and pain relief [7]. However, there is no standardization of treatment in cases with non-union and implant failures. Nail dynamization, exchange nailing, blade plating, and locking compression plating supplemented with bone grafting have been tried as revision surgeries in AFFs [8]. In our case, we used the technique of exchange K-nail, augmented plating, and bone grafting as described by Sancheti et al. [9] in cases of aseptic femoral diaphyseal non-union and achieved successful union with excellent functional outcomes without any complications. Informed consent was obtained from the patient regarding the inclusion in the study and the need for a case report.
Case Report
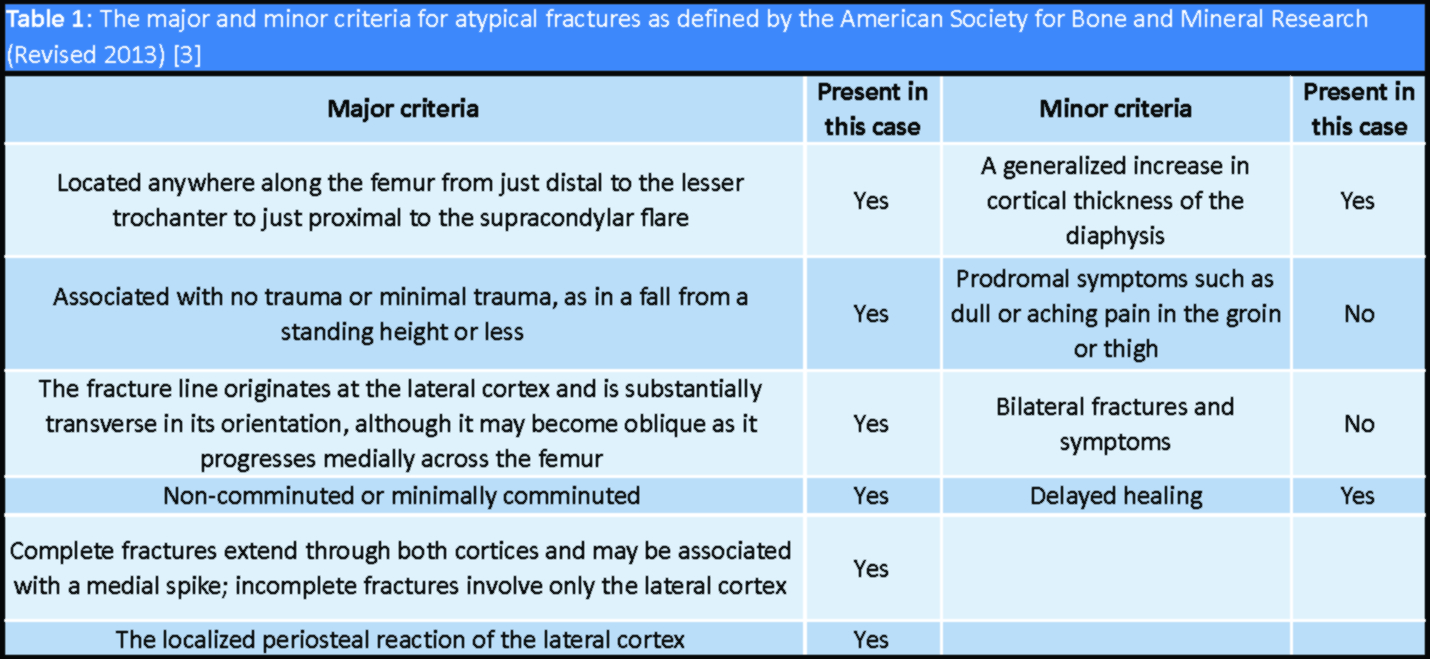
A 75-year-old lady presented to our emergency room after a trivial fall and severe pain in her right thigh and inability to walk. There was a history of BP intake for the treatment of osteoporosis for 5 years duration. There was no history of prodromal thigh pain. Radiographs of the right femur showed a complete fracture of the right femur shaft at the isthmus with the transverse lateral cortex, medial spike, and increased cortical thickening suggestive of atypical nature of this fracture (Fig. 1). As per the criteria given by the Task Force of ASBMR, the patient had all major and minor criteria except that the patient had no prodromal symptoms and bilateral association (Table 1).
These signs led to a diagnosis of Atypical fracture of the femoral shaft. The radiograph of the contralateral femur showed no signs of an incomplete fracture. Subsequently, BP was stopped and the patient underwent closed intramedullary nailing with post-operative radiograph showing acceptable reduction and stable fixation (Fig. 2). Postoperatively, the patient was started on active exercises and non-weight-bearing with a walker on day 1, and subsequently, the patient was discharged on day 3.
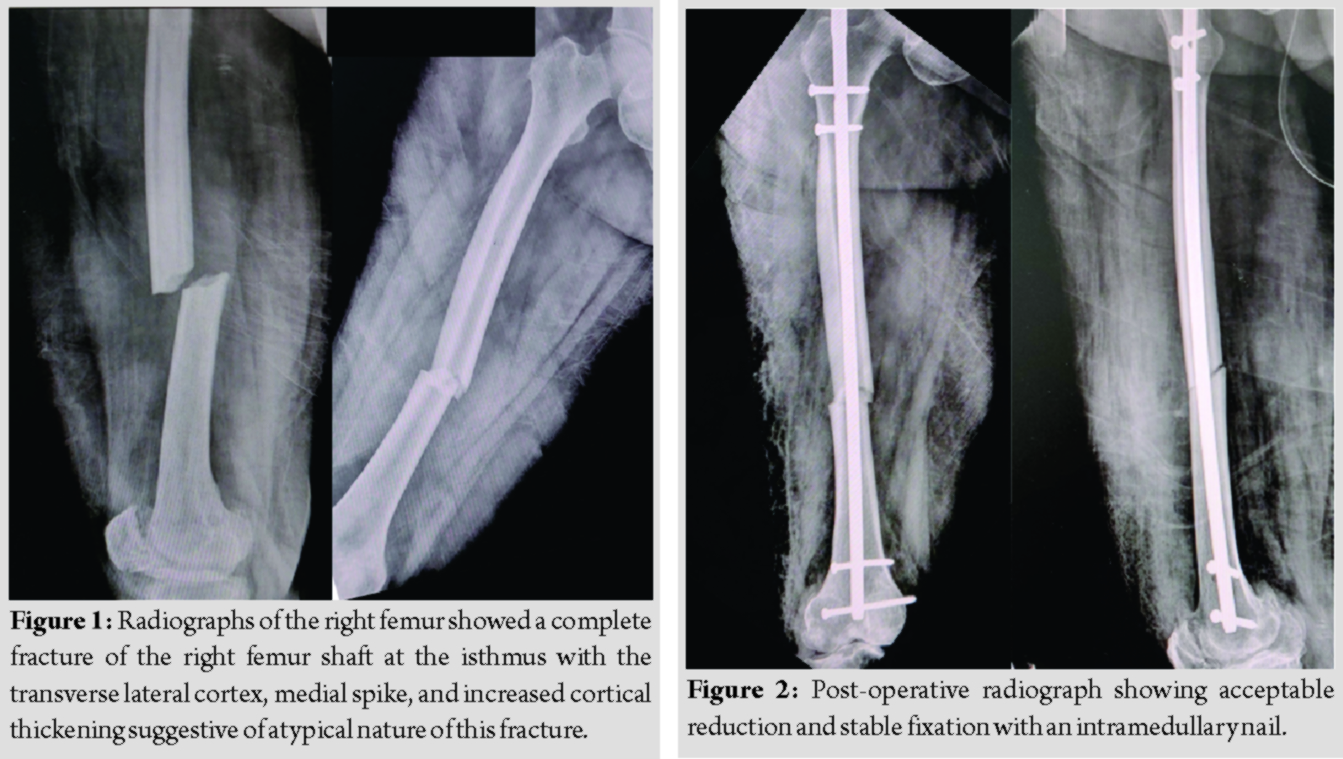
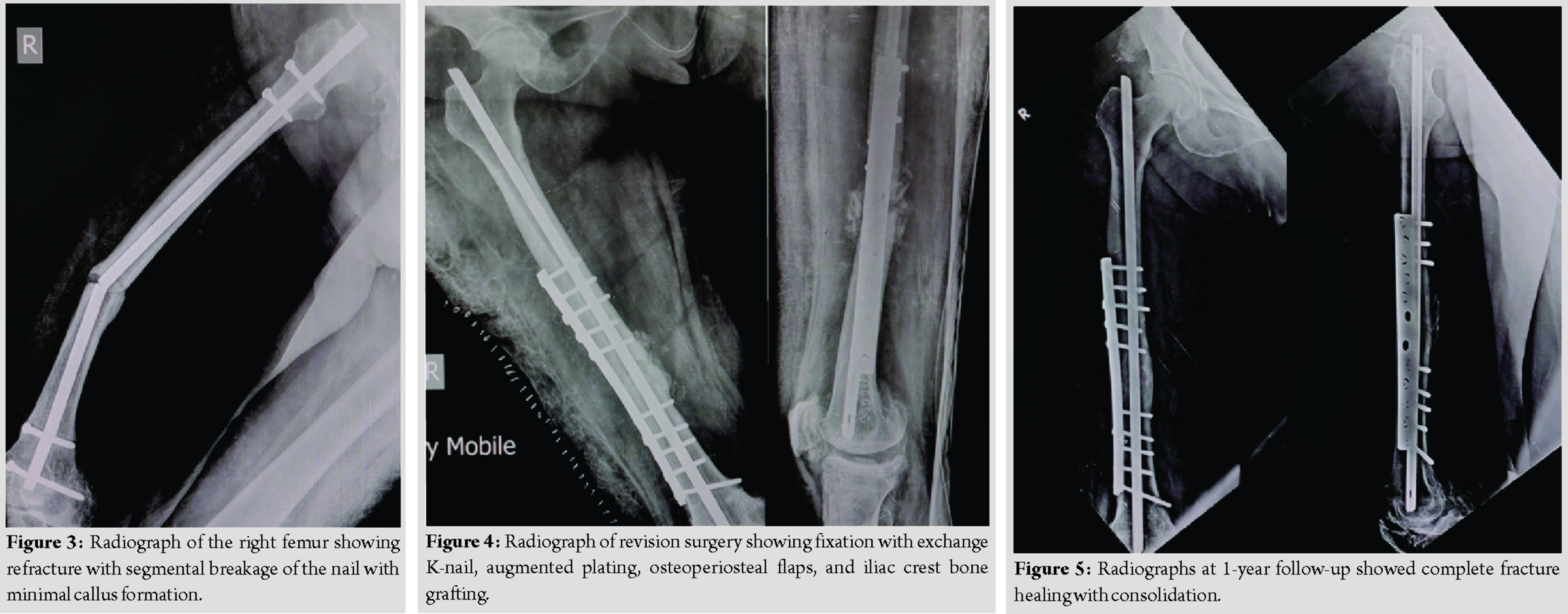
The radiographs at 3months showed evidence of callus formation, and the patient was advised weight-bearing walking. Subsequent radiographs at follow-ups showed slow healing of the fracture with minimal callus formation. At 9 months, the patient again presented to the emergency room with thigh pain after getting up from sitting position. Clinical examination showed varus deformity of the right thigh with radiographs showing refracture with segmental breakage of the nail at the level of fracture and distal bolts with minimal callus formation (Fig. 3).This led to the impression that the AFF in the diaphyseal region did not unite in 9 months. Subsequently, the patient was treated with exposure of the fracture site, removal of the nail, and fibrous union. The sclerotic bone ends were removed until there was punctuate bleeding from the bone ends. The fixation was performed with K-nail and augmented plating, as shown by Sancheti et al. [9] and was supplemented with osteoperiosteal flaps and iliac crest bone grafting (ICBG) (Fig. 4).Postoperatively, the patient was started on active exercises and non-weight-bearing walking with walker support on day 2and was discharged from the hospital on day 5. The patient was followed up regularly at 1-month intervals. The radiographs at 3 months showed good callus formation and the patient was advised to complete weight-bearing. The fracture healed successfully at 6 months and the patient started walking without support. At 1-year follow-up, the patient had full hip and knee range of motion and radiographs showed complete fracture healing with consolidation (Fig. 5).
Discussion
At present, the standard of care for treatment of complete AFF is the immediate discontinuation of BP, assessment of contralateral femur for any signs of incomplete AFF, internal fixation preferably using an intramedullary device, and supplementation with calcium and vitamin D [3, 10, 11]. Surgically treated complete AFFs exhibit delayed but reliable fracture healing [12]. Delayed but reliable fracture healing is a recognized feature of complete AFFs treated surgically [12]. Egol et al. reported a mean healing time of 8.3 months (7.1 months in the anatomically reduced group and 10.8 months in non-anatomically reduced group), indicating delayed healing in these fractures. They reported one case of non-union with cephalomedullary nailing which was revised to compression plating using blade plate and bone grafting [12]. This delay may be due to suppressed bone turnover secondary to prolonged BP therapy [5]. Studies have shown that the initial phase of callus formation is unaffected by BPs, while the remodeling phase with cortical bone healing is primarily affected by BP therapy, and this action is caused by suppression of coupled action of osteoblasts and osteoclasts [13]. The literature gives variable surgical success in complete AFFs with several studies showing variable healing rates of 85% in a recent review by Koh et al. [14] and 54% by Weil et al. [8]. Lim et al. reported an association of the post-fixation gap at the fracture site at the lateral or anterior cortex with delayed union or non-union [15]. Saleh et al. recommended the use of autologous bone marrow grafting during primary fixation to increase healing rates [16]; however, no studies have reported the efficacy of this procedure. The literature reports various treatment options for delayed union and non-union incomplete AFFs with no standardization of the treatment. Weil et al. reported secondary procedures such as dynamization of the nail, exchange nailing, or revision with surface fixation in patients with complete AFFs [8]. Giannotti et al. reported a case of atrophic non-union in a patient previously treated with an intramedullary nail, which united successfully within 3 months with revision of intramedullary nail and supplementation with strontium ranelate [17]. Bonifacio et al. reported a case of AFF in the subtrochanteric region with non-union and breakage of the intramedullary nail. The patient was treated with exchange nailing with cephalomedullary nail and ICBG, leading to fracture healing in 3 months [11]. Lee et al. reported the use of low-intensity pulsed ultrasound(LIPUS) in treating six AFFs, leading to earlier healing. Two of the cases were AFFs with non-union [18]. Lovy et al. reported faster union with bone marrow aspirate concentrate and demineralized bone matrix injections after intramedullary nailing of AFFs [6]. Pispati et al. showed asuccessful union with subcutaneous teriparatide 20 mcg for 18 months in subtrochanteric AFF with delayed healing [19]. Sancheti et al. reported 100% union exchange K-nail and augmented plating in aseptic femoral diaphyseal non-union in the study of 70 patients and concluded that exchange K-nailing and augmented plating supplemented by bone grafting area good method for achieving union in diaphyseal femoral non-union [9]. They used the combined effect of torsional stability with the plate and axial as well as bending stability with nail [20]. In our case, we followed a similar technique of removal of any fibrous structures between fracture ends, extracting the segmentally broken nail, exchange K-nailing, and augmented dynamic compression plating. To supplement this mechanical stability, osteoperiosteal flaps were raised and ICBG was added to initiate the biology. To the best of our knowledge, this is the first report of exchange K-nailing and augmented plating in the femur diaphyseal non-union of AFF. Due to the lack of literature supporting the use of medical therapy for early healing in revision surgeries of AFFs, we avoided using recombinant parathyroid hormone-like teriparatide or strontium ranelate in our case. Further studies with larger sample size are required to validate these results.
Conclusion
Non-union and implant failure are a recognized feature of AFFs and may necessitate revision surgery to achieve a successful union. Our case achieved a successful union using the combined benefit of exchange K-nailing and augmented plating along with bone grafting for diaphyseal AFF with non-union without any complication.
Clinical Message
Non-union and implant failure are recognized features of AFFs and may necessitate revision surgery to achieve a successful union. Exchange K-nailing and augmented plating techniques can be performed successfully along with bone grafting for treating diaphyseal AFF non-union.
References
1. Grady MK, Watson JT, Cannada LK. Treatment of femoral fracture nonunion after long-term bisphosphonate use. Orthopedics 2012;35:e991-5.
2. Lim SJ, Yeo I, Yoon PW, Yoo JJ, Rhyu KH, Han SB, et al. Incidence, risk factors, and fracture healing of atypical femoral fractures: A multicenter case-control study. Osteoporos Int 2018;29:2427-35.
3. Shane E, Burr D, Abrahamsen B, Adler RA, Brown TD, Cheung AM, et al. Atypical subtrochanteric and diaphyseal femoral fractures: Second report of a task force of the American society for bone and mineral research. J Bone Miner Res 2014;29:1-23.
4. Carvahlo NN, Voss LA, Almeida MO, Salgado CL, Bandeira F. Atypical femoral fractures during prolonged use of bisphosphonates: Short-term responses to strontium ranelate and teriparatide. J Clin Endocrinol Metab 2011;96:2675-80.
5. Negri AL, Rodolfo F. Healing of subtrochanteric atypical fractures after strontium ranelate treatment. Clin Case Miner Bone Metabol 2012;9:166-9.
6. Lovy AJ, Kim JS, Di Capua J, Somani S, Shim S, Keswani A, et al. Intramedullary nail fixation of atypical femur fractures with bone marrow aspirate concentrate leads to faster union: A case-control study. J Orthop Trauma 2017;31:358-62.
7. Yeh WL, Su CY, Chang CW, Chen CH, Fu TS, Chen LH, et al. Surgical outcome of atypical subtrochanteric and femoral fracture related to bisphosphonates use in osteoporotic patients with or without teriparatide treatment. BMC Musculoskelet Disord 2017;18:527.
8. Weil YA, Rivkin G, Safran O, Liebergall M, Foldes AJ. The outcome of surgically treated femur fractures associated with long-term bisphosphonate use. J Trauma 2011;71:186-90.
9. Sancheti KH, Pradhan C, Patil A, Puram C, Bharti P, Sancheti P, et al. Effectiveness of exchange K-nail and augmented plating in aseptic femoral diaphyseal non-union. Injury 2017;48 Suppl 2:S61-5.
10. Sodhai V, Pradhan C, Shyam A. Intramedullary nailing: Definitive as well as prophylactic fixation method in a case of bilateral atypical femoral fractures-a case report. J Orthop Case Rep 2019;9:61-4.
11. Bonifacio L, Syson P. Construct failure in an atypical femoral fracture treated with intramedullary nailing: A case report. Malays Orthop J 2014;8:82-4.
12. Egol K, Park JH, Rosenberg ZS, Peck V, Tejwani N. Healing delayed but generally reliable after bisphosphonate-associated complete femur fractures treated with IM nails. Clin Orthop Relat Res 2014;472:2728-34.
13. McDonald M, Schindeler A, Little D. Bisphosphonate treatment and fracture repair. Bonekey Osteovision 2007;4:236-51.
14. Koh A, Guerado E, Giannoudis PV. Atypical femoral fractures related to bisphosphonate treatment: Issues and controversies related to their surgical management. Bone Joint J 2017;99-B:295-302.
15. Lim HS, Kim CK, Park YS, Moon YW, Lim SJ, Kim SM. Factors associated with increased healing time in complete femoral fractures after long-term bisphosphonate therapy. J Bone Joint Surg Am 2016;98:1978-87.
16. Saleh A, Hegde VV, Potty AG, Lane JM. Bisphosphonate therapy and atypical fractures. Orthop Clin North Am 2013;44:137-51.
17. Giannotti S, Bottai V, Dell’Osso G, De Paola G, Ghilardi M, Guido G. Pseudoarthrosis in atypical femoral fracture: Case report. Osteoporos Int 2013;24:2895-5.
18. Lee SY, Niikura T, Iwakura T, Fukui T, Kuroda R. Clinical experience with the use of low-intensity pulsed ultrasound (LIPUS) in the treatment of atypical femoral fractures. J Orthop Trauma 2017;31:S2.
19. Pispati A, Pandey V, Patel R. Oral bisphosphonate induced recurrent osteonecrosis of jaw with atypical femoral fracture and subsequent mandible fracture in the same patient: A case report. J Orthop Case Rep 2018;8:85-8.
20. Park K, Kim K, Choi YS. Comparison of mechanical rigidity between plate augmentation leaving the nail in situ and interlocking nail using cadaveric fracture model of the femur. Int Orthop 2011;35:581-5.
 |
 |
 |
| Dr. Vivek M. Sodhai | Dr. Chetan V. Pradhan | Dr. Ashok K. Shyam |
| How to Cite This Article: Sodhai VM, Pradhan CV, Shyam AK. Exchange K-nailing, Augmented Plating Technique for Atypical Femur Diaphyseal Non-union, and Implant Failure – A Case Report. Journal of Orthopaedic Case Reports 2020 May-June;10(3): 5-9. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com




