[box type=”bio”] Learning Point of the Article: [/box]
Bone graft substitute β-tricalcium phosphate was implanted through a small fenestration in the greater trochanter using a special funnel, and the funnel was particularly useful for proximal femoral cystic lesions.
Case Report | Volume 10 | Issue 3 | JOCR May – June 2020 | Page 23-26 | Akio Sakamoto, Takeshi Okamoto, Shuichi Matsuda. DOI: 10.13107/jocr.2020.v10.i03.1732
Authors: Akio Sakamoto[1], Takeshi Okamoto[1], Shuichi Matsuda[1]
[1]Department of Orthopaedic Surgery, Graduate School of Medicine, Kyoto University, Kyoto, Japan.
Address of Correspondence:
Dr. Akio Sakamoto,
Department of Orthopaedic Surgery, Graduate School of Medicine, Kyoto University, Shogoin, Kawahara-cho 54, Sakyo-ku, Kyoto 606-8507, Japan.
E-mail: akiosaka@kuhp.kyoto-u.ac.jp
Abstract
Introduction: Bone grafts are widely performed to fill bone cavities and accelerate bone ingrowth. Advances in minimally invasive surgical techniques to treat bone tumors provide the impetus for minimally invasive bone graft procedures. A special funnel with an inner plunger has been manufactured specifically for the delivery of bone graft substitutes.
Technique: Secondary bone cysts in two patients with fibrous dysplasia (a 42-year-old male and a 36-year-old female) were treated with the bone graft substitute β-tricalcium phosphateby implantation through a small fenestration in the greater trochanter using a special funnel. Bone consolidation has been observed at about 6 months after the surgery.
Conclusions: Secondary bone cysts in two patients with fibrous dysplasiaare presented as representative cases for this method. The funnel was particularly useful for proximal femoral cystic lesions, as a solitary bone cyst; it facilitated a minimally invasive surgical procedure without the need for curettage. Small fenestrations reduce the likelihood of surgery-related fractures. Long-term follow-up is necessary to confirm the method and is capable of curing secondary bone cysts in patients with fibrous dysplasia.
Keywords: Beta-tricalcium phosphate, bone cysts, bone graft, fibrous dysplasia, funnel.
Introduction
The cavity created after curettage of bone tumors is often filled with bone autograft[1] or an osteosynthetic material, such as β-tricalcium phosphate (β-TCP) [2]. During minimally invasive procedures when β-TCP is implanted, it is necessary to avoid the spread of β-TCP to the subcutaneous tissue because it can cause a host inflammatory response [3]. A specially designed funnel with an inner plunger has now been manufactured to better target the delivery of β-TCP (HOYA Corporation, PENTAX New Ceramics Division, Tokyo, Japan). A solitary bone cyst is a cystic lesion filled with fluid, characterized by a thinned cortex, which primarily appears during childhood and adolescence. The surgical strategies for solitary bone cysts include percutaneous reconstruction with bone grafts or bone substitutes [4]. Bone cysts can occur in adults as a consequence of disease or trauma, such as a fracture [5]. In adults, these bone cysts are referred to as secondary bone cysts. Fibrous dysplasia is a benign fibro-osseous lesion, characterized histologically by bland-looking fibroblasts and an irregularly shaped bone [6]. The incidence of secondary bone cysts in fibrous dysplasia is unknown, because of an absence of reports. In contrast, secondary aneurysmal bone cysts which are filled with blood can occur in fibrous dysplasia as preexisting bone lesions [7, 8]. Among the various cases for which bone grafts are indicated, proximal femoral cystic lesions appear most suited to β-TCP implantation using a procedure that is minimally invasive, as it eliminates the need for curettage. In this report of cases with secondary bone cysts in fibrous dysplasia, the merits of using a special funnel during a minimally invasive surgery are highlighted.
Technique
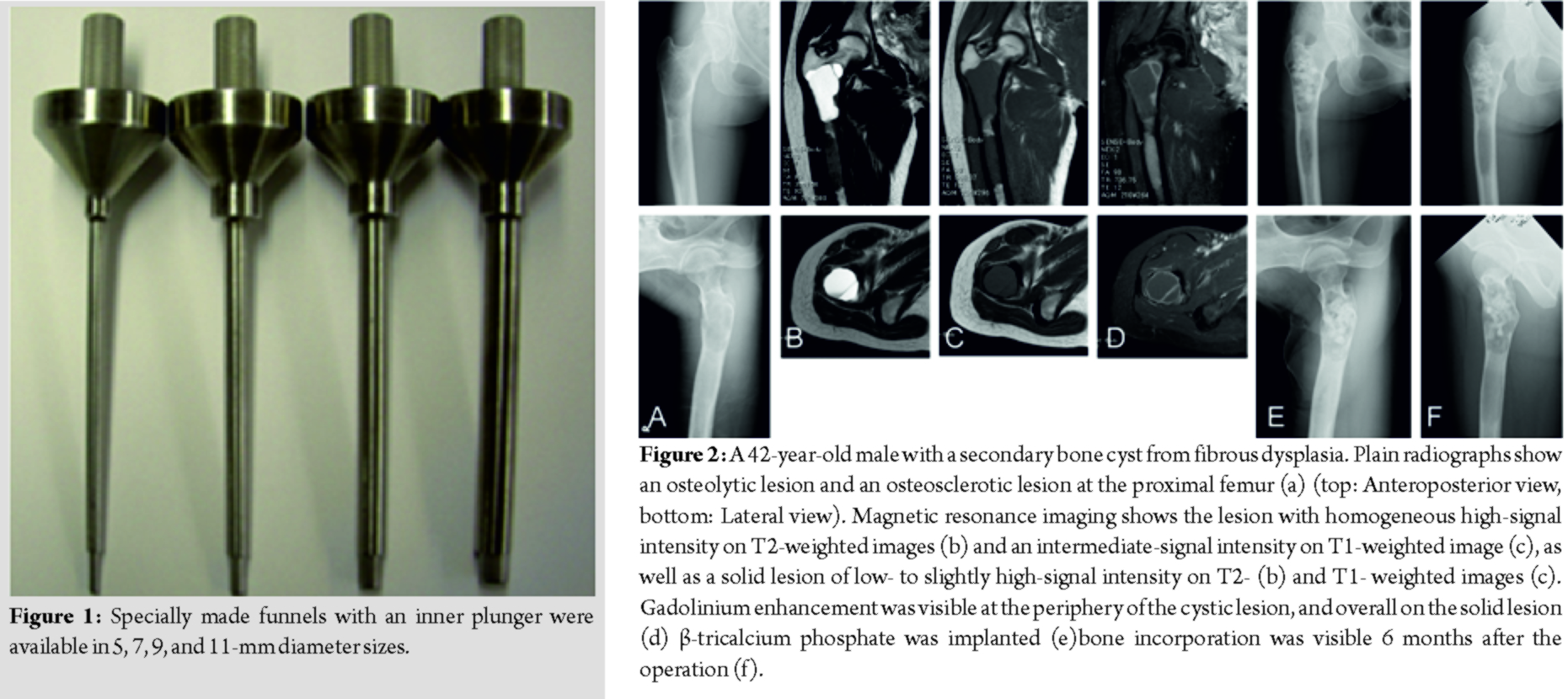
Specially manufactured funnels with an inner plunger were available in 5, 7, 9, and 11 mm diameter sizes (Fig. 1). The device has been registered for clinical usage to the Pharmaceuticals and Medical Devices Agency in Japan (#13B1X173101010). Surgery was performed in both cases under general anesthesia. The cortex of the greater trochanter adjacent to the lesion was approached from the lateral side, splitting the tensor fasciae latae. Fenestration of the cortex was performed with a surgical drill or reamer until reaching the same diameter as the funnel. β-TCP in the form of particles, cubes, and columnar shapes was implanted through the funnel.
Case Report
Case 1
A 42-year-old male reported occasional pain in his left hip when he walked. A bilateral assessment indicated a full range of motion at the hip joints. Plain radiographs showed an osteolytic area at the femoral neck and distally adjacent osteosclerosis (Fig. 2a). Magnetic resonance imaging (MRI)revealed an osteolytic lesion with homogeneous high-signal intensity and intermediate-signal intensity in the T2- and T1-weighted images, respectively. The homogeneous signal intensity, as well as the peripheral enhancement by gadolinium, suggested that the lesion was of a cystic nature and contained serous fluid (Fig. 2b-d). Also based on MRI, in the osteosclerotic area there was a heterogeneous low-to slightly high-signal intensity on T2- and T1-weighted images, with gadolinium enhancement (Fig. 2b-d).Accordingly, the osteosclerotic lesion was diagnosed as fibrous dysplasia. The cystic lesion in the bone was a secondary bone cyst. The reported pain was judged to be caused byan impending fracture at the lesion site. The implantation of β-TCP was performed through a small 7-mm fenestration in the lateral greater trochanter. Intraoperative findings confirmed that the lesion was cystic, and that the intra-cystic content was serous, but did not contain blood. A needle biopsy from the osseous lesion was performed. Columnar-shaped β-TCP and β-TCP particles were implanted using the special funnel (7mm diameter). The histology showed irregular shaped trabeculae composed of woven bone lacking osteoblastic rimming, embedded in a cellular fibrous stroma of bland-looking spindle- or stellate-shaped cells. The histology of the fibrotic bone lesion confirmed the diagnosis of fibrous dysplasia. For 1 month postoperatively, weight bearing was allowed with a single crutch. The implanted β-TCP was gradually incorporated (Fig. 2e and f). There was no recurrence of hip pain 6 months postoperatively.
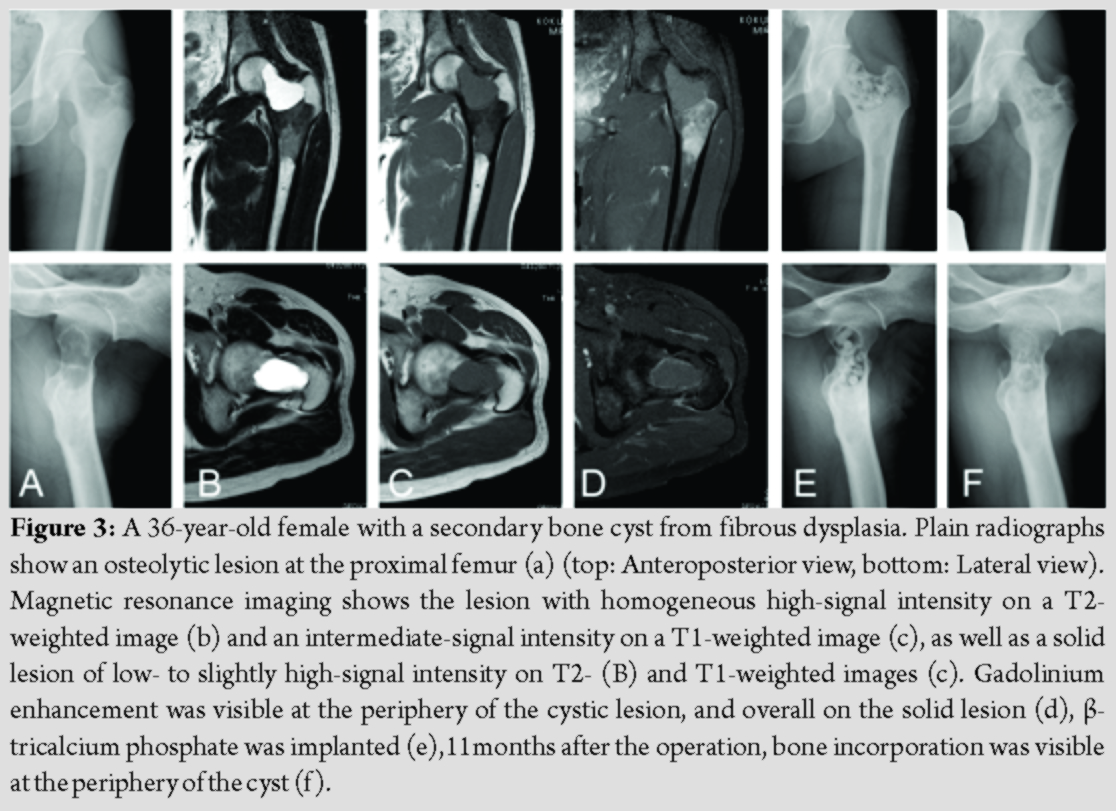
Case 2
A36-year-old female reported occasional pain in the right proximal thigh. At the initial examination, she did not have pain. Plain radiographs showed an osteolytic lesion at the proximal femur (Fig. 3a). MRI demonstrated an osteolytic lesion with homogeneous high-signal intensity and low-signal intensity in the T2- and T1-weighted images, respectively. Gadolinium enhancement was only seen at the periphery (Fig. 3b-3d). An MRI in the osteosclerotic area demonstrated homogeneous low- to slightly high-signal intensity on T2- and T1-weighted images (Fig. 3b-3d).The diagnosis was a secondary bone cyst in fibrous dysplasia. There is a higher gender-associated risk of developing osteoporosis which could increase the possibility of a future fracture. During the operation, the cortex of the lateral greater trochanter was fenestrated to enable a 7-mm funnel to be used for the implantation of β-TCP into the cystic lesion (Fig. 3e). Columnar-shaped β-TCP and β-TCP particles were implanted using the special funnel. A needle biopsy was also performed. Histologically, the lesion was composed of irregular-shaped trabeculae composed of woven bone lacking osteoblastic rimming, embedded in a fibrous stroma containing fibroblast-like spindle or oval cells. The features were compatible with fibrous dysplasia. Full weight bearing without the use of a crutch was allowed. The implanted β-TCP was gradually incorporated into host bone (Fig. 3f).
Discussion
Bone grafts are commonly performed to fill bone cavities. After the curettage of a bone tumor, the cavity created is often filled with bone autograft or synthetic bone material, including β-TCP[2]. With advances in minimally invasive treatments, including endoscopic procedures, a minimally invasive procedure would be most appropriate in many circumstances. Previously, a 3.5-mm drill sleeve has been used in bone grafts with autologous cancellous bone to treat a talar bone cyst [9]. This report describes the use of a novel, specially made funnel with an inner plunger used to deliver a bone graft substitute. Among all the various indications for bone grafting, the use of a funnel to deliver osteosynthetic material to the proximal femoral neck to treat trochanteric lesions is most beneficial because a curettage or tumor resection becomes unnecessary. The use of the funnel device simplified the implantation of β-TCP and reduced surgical time. In the current cases, β-TCP was chosen as a filler for the cavity. After the curettage in benign bone tumors, the cavity is often filled with bone autograft/allograft, polymethylmethacrylate bone cement or β-TCP. Bone autograft/allograft and β-TCP can be remodeled to normal bone. Bone autograft is insufficient in quantity when the lesion is large. In the current report, secondary bone cysts in fibrous dysplasias are presented as representative cases for this method. In a previous report, when fibrous dysplasia patients have pain, a limp or radiological evidence of microfracture, surgical treatment is necessary. Of the 53 patients who were initially treated non-operatively, 45 (85%) remained asymptomatic [10]. The application of this method to secondary bone cysts in fibrous dysplasias might prevent further surgical treatment. However, long-term follow-up is necessary to confirm the method and is capable of curing these secondary bone cysts in patients with fibrous dysplasia. The funnel was particularly useful for proximal femoral cystic lesions, as a solitary bone cyst. Solitary bone cysts in long bones are mostly located in the metaphysis, adjacent to the epiphyseal plate in children and adolescents [11]. The development of lesions may be related to skeletal growth. The pathogenesis of solitary bone cysts in the long bones has been assumed to be a blockage of the circulation due to venous obstruction [12]. Secondary solitary bone cysts arise from healed or healing fractures and have been reported in theliterature[13]; their occurrence after a fracture provides plausible evidence in support of the “trauma-hemorrhage” theory for explaining their presence [5]. The differential diagnosis of solitary bone cysts among cystic lesions is an aneurysmal bone cyst, characterized by an expansive cystic lesion containing blood. Aneurysmal bone cysts are benign, intraosseous, and solitary lesions that consist of large thin-walled cavities that are usually filled with blood [7]. The proposed pathogenesis includes arteriovenous shunts, bleeding due to trauma, and bleeding from a prior bone lesion [14]. Various pre-existing bone lesions, including fibrous dysplasia, giant cell tumors, chondroblastomas, and non-ossifying fibromas, have beenreported [8, 15]. In the current cases, the absence of blood excluded the diagnosis of an aneurysmal bone cyst. However, it is possible that a bone cyst in a patient with fibrous dysplasia might be a remnant condition of a secondary aneurysmal bone cyst.
Conclusion
A specially made funnel for delivering bone substitute material is currently available. A minimally invasive procedure in which curettage or tumor resection is unnecessary for the implantation of β-TCP into a secondary bone cyst in fibrous dysplasia is reported. Utilizing the funnel has merit given it facilitates the well-controlled and targeted delivery of β-TCP to a lesion during the implantation procedure and reduces the time taken to perform each operation.
Clinical Message
Bone grafts are frequently performed to fill bone cavities and accelerate bone ingrowth. Secondary bone cysts in two patients with fibrous dysplasia (a 42-year-old male and a 36-year-old female) were treated with the bone graft substitute β-TCP by implantation through a small fenestration in the greater trochanter using a special funnel. The funnel is particularly useful for proximal femoral cystic lesions; it facilitates a minimally invasive bone procedure without the need for curettage. Small fenestrations reduce the likelihood of surgery-related fractures.
References
1. O’Donnell RJ, Springfield DS, Motwani HK, Ready JE, Gebhardt MC, Mankin HJ. Recurrence of giant-cell tumors of the long bones after curettage and packing with cement. J Bone Joint Surg Am. 1994;76:1827-33.
2. Sakamoto A. Reconstruction with β-tricalcium phosphate for giant cell tumor of bone around the knee. J Knee Surg. 2016;30:75-7.
3. Lin K, Yuan W, Wang L, Lu J, Chen L, Wang Z, et al. Evaluation of host inflammatory responses of β-tricalcium phosphate bioceramics caused by calcium pyrophosphate impurity using a subcutaneous model. J Biomed Mater Res B Appl Biomater. 2011;99:350-8.
4. Yildirim C, Akmaz I, Sahin O, Keklikci K. Simple calcaneal bone cysts: a pilot study comparing open versus endoscopic curettage and grafting. J Bone Joint Surg Br. 2011;93:1626-31.
5. Rosario MS, Yamamoto N, Hayashi K, Takeuchi A, Kimura H, Miwa S, et al. An unusual case of proximal humeral simple bone cyst in an adult from secondary cystic change. World J Surg Oncol. 2017;15:102.
6. Shin SJ, Lee SJ, Kim SK. Frequency of GNAS R201H substitution mutation in polyostotic fibrous dysplasia: pyrosequencing analysis in tissue samples with or without decalcification. Sci Rep. 2017;7:2836.
7. Sasaki H, Nagano S, Shimada H, Yokouchi M, Setoguchi T, Ishidou Y, et al. Diagnosing and discriminating between primary and secondary aneurysmal bone cysts. Oncol Lett. 2017;13:2290-6.
8. Anderson N, DiBella C, Pianta M, Slavin J, Choong P. Aggressive aneurysmal bone cyst in association with polyostotic fibrous dysplasia: a case report. Int J Surg Case Rep. 2015;12:52-6.
9. Lui TH. Endoscopic curettage and bone grafting of huge talar bone cyst with preservation of cartilaginous surfaces: surgical planning. Foot Ankle Surg. 2014;20:248-52.
10. Han I, Choi ES, Kim HS. Monostotic fibrous dysplasia of the proximal femur: natural history and predisposing factors for disease progression. Bone Joint J. 2014;96-B:673-6.
11. Sakamoto A, Matsuda S, Yoshida T, Iwamoto Y. Clinical outcome following surgical intervention for a solitary bone cyst: emphasis on treatment by curettage and steroid injection. J Orthop Sci. 2010;15:553-9.
12. Cohen J. Intramedullary nailing for the treatment of unicameral bone cysts. J Bone Joint Surg Am. 2001;83-A:1279-80.
13. Moore TE, King AR, Travis RC, Allen BC. Post-traumatic cysts and cyst-like lesions of bone. Skeletal Radiol. 1989;18:93-7.
14. Gibbs CP Jr., Hefele MC, Peabody TD, Montag AG, Aithal V, Simon MA. Aneurysmal bone cyst of the extremities. Factors related to local recurrence after curettage with a high-speed burr. J Bone Joint Surg Am. 1999;81:1671-8.
15. Sakamoto A, Ishii T, Oda Y, Iwamoto Y. Nonossifying fibroma presenting as an aneurysmal bone cyst: a case report. J Med Case Rep. 2012;6:407.
 |
 |
 |
| Dr. Akio Sakamoto | Dr. Takeshi Okamoto | Dr. Shuichi Matsuda |
| How to Cite This Article: Sakamoto A, Okamoto T, Matsuda S. A minimally invasive novel technique using a new device to treat proximal femoral cystic lesions. Journal of Orthopaedic Case Reports 2020 May-June;10(3): 23-26. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com




