[box type=”bio”] Learning Point of the Article: [/box]
Management of Pediatric cervical hemivertebra with neurodeficit.
Case Report | Volume 10 | Issue 4 | JOCR July 2020 | Page 13-16 | Aniket M. Gupta, Jayprakash V. Modi, Pratik H. Israni, Deepak Agrawal, Shrey K. Desai, Nirav Mungalpara. DOI: 10.13107/jocr.2020.v10.i04.1780
Authors: Aniket M. Gupta[1], Jayprakash V. Modi[1], Pratik H. Israni[1], Deepak Agrawal[1], Shrey K. Desai[1], Nirav Mungalpara[1]
[1]Department of Orthopedics, Civil Hospital Ahmedabad, Asarwa, Ahmedabad, Gujarat, India.
Address of Correspondence:
Dr. Aniket M. Gupta,
Department of Orthopedic Surgery, Civil Hospital, Ahmedabad, Gujarat, India.
E-mail: Guptaaniket30794@gmail.com
Abstract
Introduction: Hemi vertebrae are very rarely seen at a cervical level which results in kyphotic deformity without coronal tilt. Vertebral formation defects have been the basis of congenital kyphoscoliosis deformity in the pediatric age group. Cervical spine kyphosis more than 10° along with kinking of cord at a single level results in neurodeficits which require urgent management on the lines of decompression, realignment, and bony fusion to prevent recurrence and failure and to achieve superior outcomes. However, in pediatric age group, spine surgeons face a lot challenges with respect to surgical anatomy, body landmarks, and bone anchors.
Case Report: A 3-year-old male patient presented to the outpatient department with complain of progressive bilateral upper and lower limb weakness and progressive deformity of the cervical spine which increased in the past 2 months. The patient earlier used to walk with support. However, for 2 months, there was progressive decrease in motor function. The clinical course, radiologic features, pathology, and treatment outcome of the patient were documented. C3 hemivertebrectomy and stabilization from C2 to C4 with fibular strut grafting and anterior cervical plating were done under neuromonitoring guidance. The neurologic symptoms of the patient were markedly improved after surgery.
Conclusion: We have reported the first case of the management of pediatric cervical spine hemivertebrae with neurodeficit in a 3-year-old child, with anterior hemivertebrectomy, strut grafting, and plating which improved the patient neurologically and functionally.
Keywords: Hemivertebrae, Pediatric cervical deformity, Pediatric deformity, Cervical kyphosis, Congenital cervical kyphosis, Congenital kyphotic deformity.
Introduction
Cervical hemivertebrae are a very rare clinical entity, to our knowledge, there are only two cases reports published regarding the management; however, in both of them, the age at presentation with the deformity was at adolescent age [1]. Cervical hemivertebrae with neurodeficit in young child have never been reported. Etiology for pediatric cervical deformity can be either traumatic or congenital. Traumatic spinal injuries are usually missed in the pediatric age group and are later presented with late complications. However, the bony anatomy is clear with respect to vertebral body, pedicles, lateral mass, etc., in a traumatic cause. However, congenital cervical deformity leading to kyphosis is a rare clinical condition with dysplastic pedicles, hemivertebrae [2]. Congenital cervical spine kyphotic deformity has been underreported due to rarity of the cases with few case reports and small case series. It is very difficult to find literature on cervical kyphosis with posterior hemivertebra leading to compression of spinal cord causing neurology worsening and myelomalacic changes. Congenital subaxial cervical spine instability in very young or small-for-age children is uncommon and typically arises from trauma or skeletal dysplasia. Various operative techniques have been used to achieve stabilization in pediatric patients with evidence of instability, including only anterior, only posterior, and combined approaches [1]. The studies conducted on cervical kyphosis management mainly suggest that anterior approach is safer though combination of anterior and posterior approach provides better stability and better correction of deformity [3]. Combined approach, however, results in more mortality, post-operative neurology worsening, complications, and revision surgeries [3]. Hence, many surgeons [4, 5, 6] prefer anterior approach only as they are familiar with the procedure and also allow removal of compression on the spinal cord with the correction of the deformity. Our case report is on a 3-year-old male patient presenting with progressive kyphosis with C3 posterior hemivertebra with neurology worsening for which anterior fixation was done.
Case Report
A 3-year-old male patient presented to the outpatient department with complain of progressive bilateral upper and lower limb weakness and progressive deformity of the cervical spine which increased in the past 2 months. The patient earlier used to walk with support. However, for 2 months, there was progressive decrease in motor function. At the time of presentation, there was flickering movement in the hands with absent movement in rest of the limbs.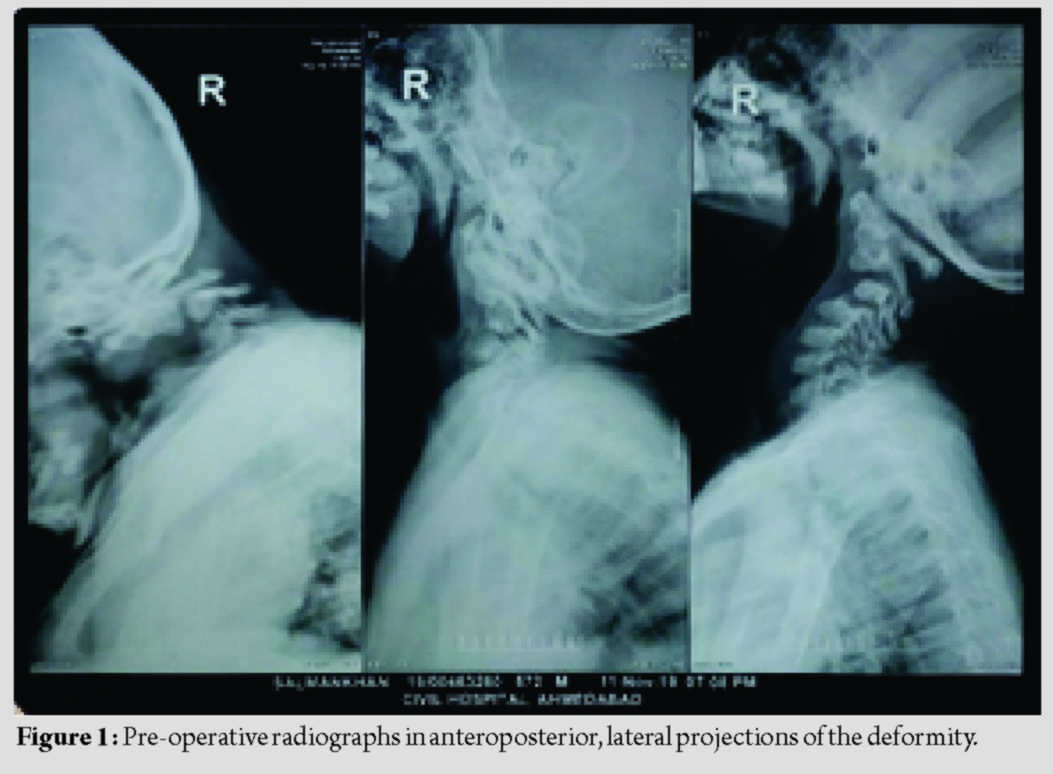
The patient had no history of recent trauma, rest of birth, family, and developmental history was insignificant. Other siblings of the patient did not have any significant medical history. Various other screening tests to identify syndromic picture were carried out and all were negative. The patient’s neck angiography was normal. Hoffman sign was negative. All the reflexes and sensation were normal. The patient’s cognitive ability was within normal range.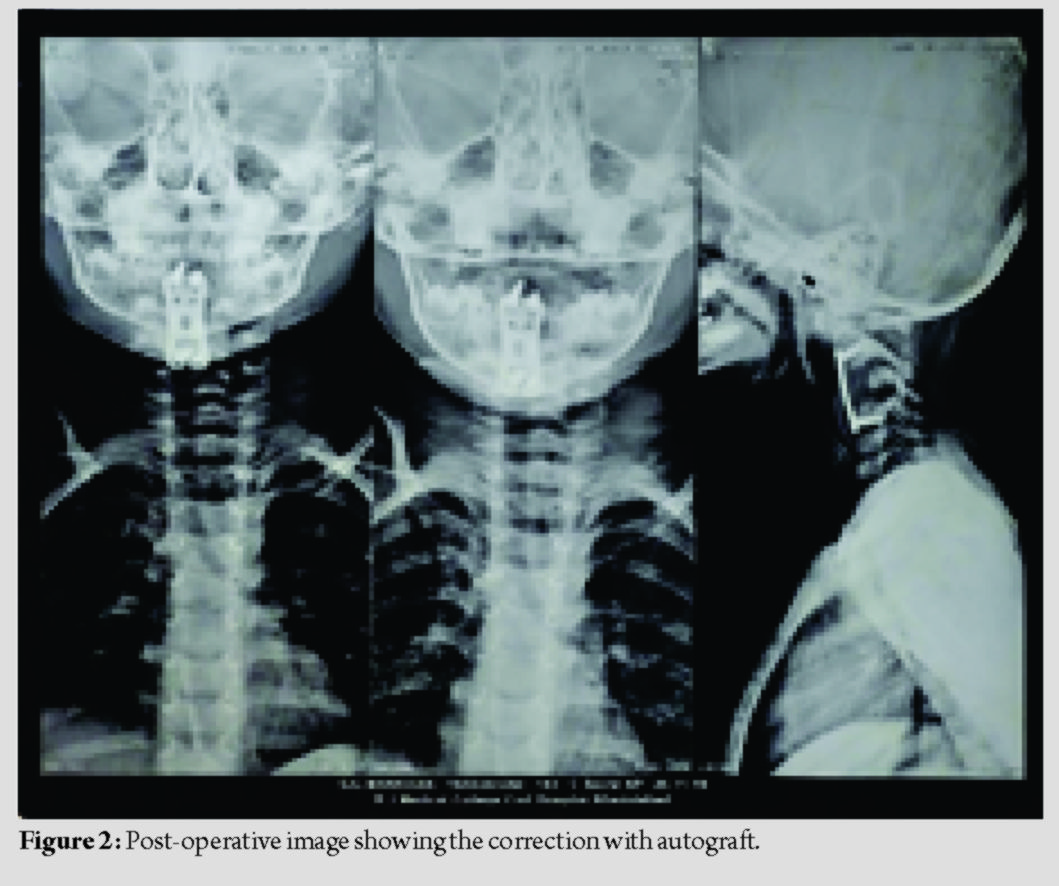
Cervical X-rays with lateral projection (Fig. 1) were done which showed C3 hemivertebrae resulting in significant kyphosis of the cervical spine posterior facet subluxation with increased interspinous widening. Mean sagittal Cobb’s angle was 35° which corrected to 5° postoperatively (Fig. 2). MRI was done which showed significant compression at C3 level with canal diameter of 4.7 mm with myelomalacia (Fig. 3) which were hyperintense on T2-weighted images and hypointense on T1. Dynamic and static (Fig. 4) 3D computed tomography (CT) scan were done preoperatively to understand the bony anatomy, flexibility of the kyphosis, and course of vertebral artery and to plan the bony anchors and instrumentation.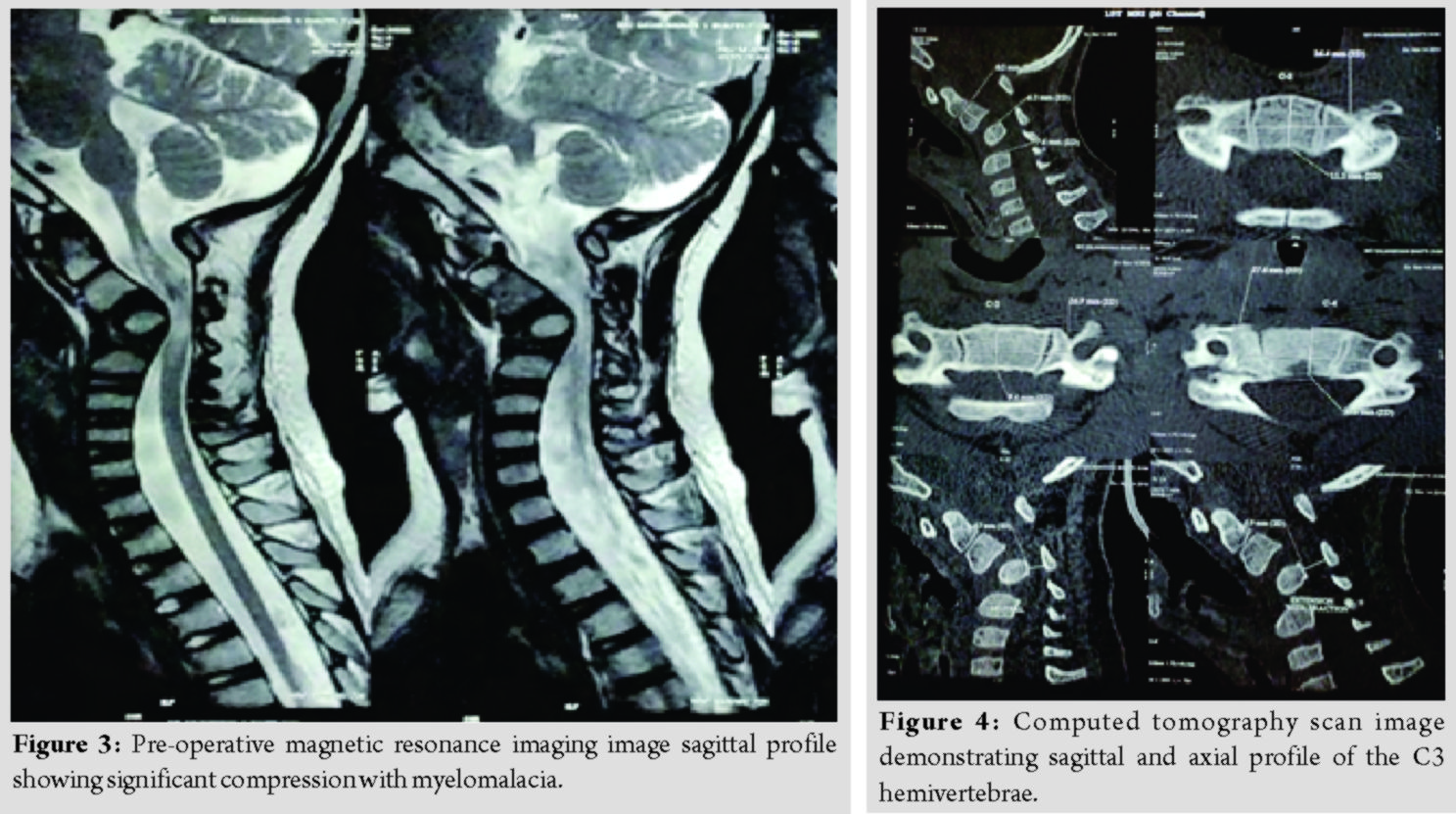
The patient was operated for corpectomy with anterior cervical plate fixation and a fibular strut graft from the left leg was used (Fig. 2, 5). The patient was stable postoperatively and using SOMI brace, bedside mobilization was started. The patient had improved neurologically with motor power from 0/5 to 4/5 in both upper and lower limbs. Physiotherapy with handgrip strengthening exercises was started.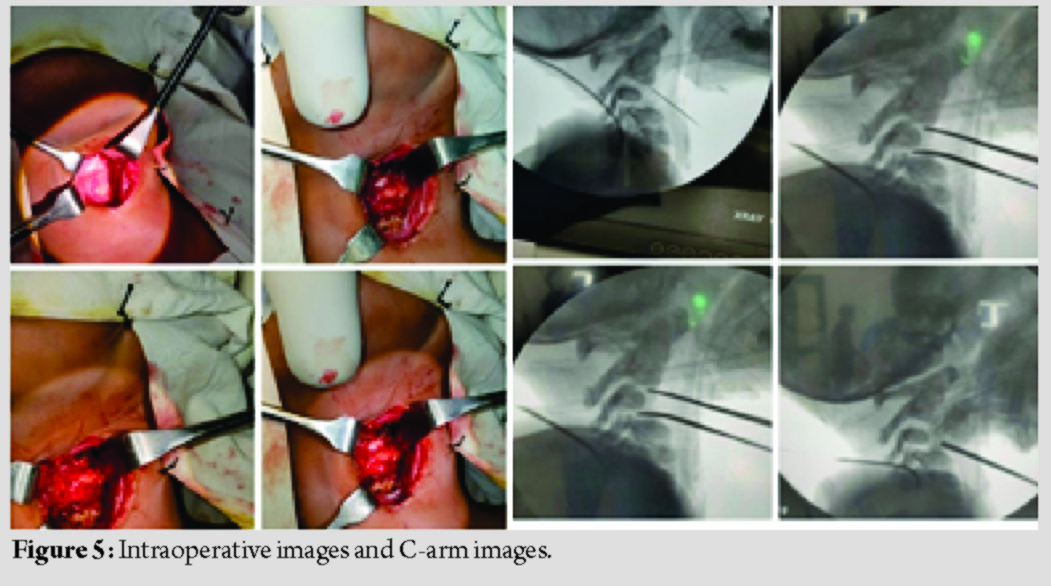
Discussion
Stabilization with implants in the infantile spine is challenging due to the diminutive size of the bony anatomy and cartilaginous end plates and the lack of spinal instrumentation designed specifically for its fixation.
Challenges that spine surgeons face while managing these cases:
Lack of literature to recommend the management principles along with lack of guidelines with respect to classification systems. Pediatric bone with strong cortical bone with weak cancellous part suggests unpredictable hold for the instrumentations. Lack of biomechanical studies to provide clarity for the use of instrumentation. Implants and instrumentations issue – lack of standardization as profile, dimensions, locking, constrained or semi constrained, and screw pitch biomechanical studies are lacking. Long-term studies for currently available instrumentation systems are sparse. Instrumenting upper cervical spine, particularly axis vertebrae, requires elaborate planning as far as radiography is concerned. 3D CT scan is always useful in pre-operative planning – to plan the length of screw size, bony anchors, and measuring the C2 body dimensions such as pedicle size and length of pedicle screw on the CT console. We measure the approximate length of the strut graft to be placed as well on the console. For bone grafts, autograft strut remains the gold standard for graft material through which a spinal fusion may be achieved. Allograft has its own benefits like avoidance of donor site morbidity and can be used as a structural support or as pieces in a metallic cage. These are being used around the globe with success along with its associated complications [7]. Posterior stabilization presents with similar set of challenges in pediatric age group along with predictable anomalous course of vertebral artery as reported with a hemivertebrae in cervical spine. The body of C2 fuses with the odontoid process by 3–6 years of age. In subaxial cervical spine, the neural arches fuse with body by age 2–3 years, and the body fuses with the neural arches between 3 and 6 years of age, based on this understanding senior author decided to avoid posterior stabilization with a closely monitoring of the child [8]. Halo vest traction and immobilization are also a mode of treatment to correct the deformity but are less preferred considering an average time of application for 3 months, pin loosening, pin tract infection, risk of skull penetration specially in young children of age <3 years, epidural abscess, and failure of treatment like pseudoarthrosis [9, 10].
Conclusion
In a pediatric patient of severe cervical kyphosis with neurology worsening, anterior cervical fixation is a safe and effective surgery with low rates of complications and better patient compliance. However, this cannot be generalized to the entire population since of the small level of the study and needs further validation from larger studies.
Clinical Message
In a pediatric patient with congenital cervical kyphosis with neurology worsening, we recommend correction of the deformity while relieving the compression on the cord using fibular strut graft and anterior cervical plating.
References
1. Daivajna S, Jones A, Hossein Mehdian SM. Surgical management of severe cervical kyphosis with myelopathy in osteogenesis imperfecta: a case report. Spine (Phila Pa 1976). 2005;30(7):E191-E194. doi:10.1097/01.brs.0000157471.44284.a2
2. He Z, Liu Y, Xue F, Xiao H, Yuan W, Chen D. Surgical management of congenital cervical kyphosis. Orthopedics 2012;35:e1396-401.
3. Han K, Lu C, Li J, Xiong G, Wang B, Lv G, et al. Surgical treatment of cervical kyphosis. Eur Spine J 2011;20:523‐36.
4. Ferch RD, Shad A, Cadoux-Hudson TA, Teddy PJ. Anterior correction of cervical kyphotic deformity: Effects on myelopathy, neck pain, and sagittal alignment. J Neurosurg 2004;100:13-9.
5. Gülmen V, Zileli M. Surgical treatment of postlaminectomy cervical kyphosis. Turk Neurosurg 2000;10:28-35.
6. Herman JM, Sonntag VK. Cervical corpectomy and plate fixation for postlaminectomy kyphosis. J Neurosurg 1994;80:963-70.
7. Betz RR, Lavelle WF, Samdani AF. Bone grafting options in children. Spine (Phila Pa 1976) 2010;35:1648-54.
8. Lustrin ES, Karakas SP, Ortiz AO, Cinnamon J, Castillo M, Vaheesan K, et al. Pediatric cervical spine: Normal anatomy, variants, and trauma. Radiographics 2003;23:539-60.
9. Arkader A, Hosalkar HS, Drummond DS, Dormans JP. Analysis of halo-orthoses application in children less than three years old. J Child Orthop 2007;1:337-44.
10. Garfin SR, Botte MJ, Waters RL, Nickel VL. Complications in the use of the halo fixation device. J Bone Joint Surg Am 1986;68:320-5.
 |
 |
 |
 |
 |
| Dr. Aniket M. Gupta | Dr. Jayprakash V. Modi | Dr. Pratik H. Israni | Dr. Deepak Agrawal | Dr. Shrey K. Desai |
| How to Cite This Article: Gupta AM, Modi JV, Israni PH, Agrawal D, Desai SK, Mungalpara N. Pediatric cervical Hemivertebrae – A Rare Case Presentation in a 3-Year-Old Child. Journal of Orthopaedic Case Reports 2020 July;10(4): 13-16. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com




