[box type=”bio”] Learning Point of the Article: [/box]
Excellent functional outcome can be achieved for patellar tendon reconstruction without using implants for fixation provided adequate length and thickness of the allograft is used.
Case Report | Volume 10 | Issue 5 | JOCR August 2020 | Page 29-30 | Sharath Kittanakere Ramanath, Rahul Hemant Shah, Sandesh Patil, Shreyas Umesh. DOI: 10.13107/jocr.2020.v10.i05.1824
Authors: Sharath Kittanakere Ramanath[1], Rahul Hemant Shah[2], Sandesh Patil[1], Shreyas Umesh[1]
[1]Department of Orthopaedics, Ramaiah Medical College and Hospitals, Bengaluru, Karnataka, India.
[2]Department of Orthopaedics, Bharatratna Dr. Babasaheb Ambedkar Hospital, Mumbai, Maharashtra, India.
Address of Correspondence:
Dr. Rahul Hemant Shah,
Department of Orthopaedics, Bharatratna Dr. Babasaheb Ambedkar Hospital, Mumbai, Maharashtra, India.
E-mail: rahul54shah@gmail.com
Abstract
Introduction: Neglected patellar tendon ruptures are uncommon. They are challenging due to the proximal migration of patella and soft-tissue contractures. They are usually managed with autografts or allografts with or without synthetic augmentation, and fixation is done using metallic implants.
Case Report: A 59-year-old farmer presented with an inability to straighten his knee for 6 months after sustaining a cut lacerated wound with a sickle. He was diagnosed with a patellar tendon rupture. Tendoachilles’ allograft reconstruction was done by creating transosseous tunnels in the patella and tibial tuberosity with a figure of 8 configurations of the final construct. Synthetic augmentation and metallic implants were not used. Excellent clinical and radiological results were achieved at 3 years’ follow-up.
Conclusion: Chronic patellar tendon ruptures can be managed using allograft without the need for synthetic augmentation or fixation with implants. This gives excellent clinical and radiological results.
Keywords: Patella tendon rupture, Patella alta, Knee, Neglected, Novel technique.
Introduction
Knee extensor mechanism includes quadriceps tendon, patella, patellar tendon, medial and lateral patellar retinaculum, medial and lateral patellofemoral ligaments, Hoffa’s fat pad, and prepatellar bursa [1]. Its functions are knee extension and patellofemoral joint stabilization. Structural damage affects patellofemoral joint stability, leading to early-onset patellofemoral arthritis [2]. The most common etiology for patellar tendon rupture is trauma, with males under 40 years of age being most commonly affected [3]. Unilateral ruptures mainly occur due to trauma. Bilateral ruptures usually occur in association with rheumatoid arthritis, systemic lupus erythematosus, chronic renal failure, and primary hyperparathyroidism [4]. The incidence of patellar tendon rupture is 0.68/100,000 individuals with neglected ruptures being even more uncommon [5]. Acute injuries can be managed by end-to-end suturing. This is not possible with neglected ruptures due to soft-tissue contractures and proximal patellar migration. They require reconstruction or augmentation surgeries. Here, we describe a technique of reconstruction of a neglected patellar tendon rupture by passing a tendoachilles’ allograft through tunnels drilled in the patella and tibial tuberosity. We achieved excellent clinical and radiological results without using synthetic augmentation or implants.
Case Report
A 59-year-old farmer presented with an inability to straighten his right knee for 6 months after sustaining a deep cut lacerated wound to the anterior aspect of the right knee 6 months back. The wound was cleaned and sutured without further interventions.
The patient had bipedal right extensor lag gait. A transverse scar of 1 cm × 8 cm was present inferior to the patella. Depression was noted between the inferior pole of patella and tibial tuberosity. The patient was unable to extend the knee but had active flexion up to 120° (Fig. 1). Pre-operative radiographs showed an Insall-Salvati ratio of 1.78 with no radiological evidence of fracture or avulsion (Fig. 2). Since he was a farmer, we decided to spare the hamstring muscles so that squatting would not be affected. Blood investigations revealed a hemoglobin of 15.2 g/dl with no signs of infection.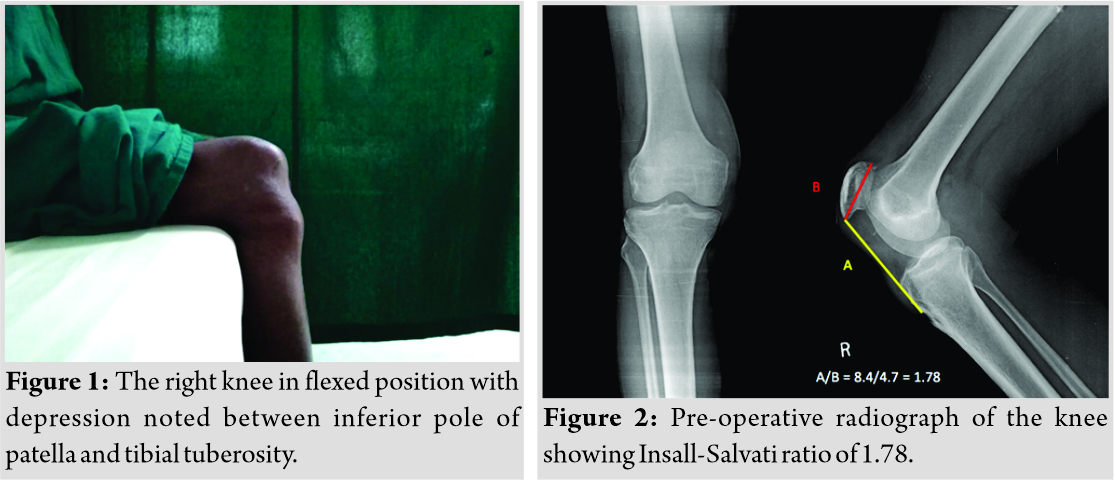
The patient was positioned supine with spinal anesthesia. Tourniquet was avoided as it would have hindered with intraoperative patellar length assessment due to quadriceps tethering. A vertical midline incision was taken from the center of the patella to tibial tuberosity. Patellar tendon was found to be lacerated and retracted. Adhesions around the patella and quadriceps tendon were released. Tendoachilles’ allograft of length 23 cm was procured from a tissue bank adhering to strict protocols. The graft was acquired 1 h before the surgery after informing the previous day. It was thawed, then cleaned with normal saline and 5% povidone-iodine solution. Distal bony attachment was excised. The graft was cut along its length to give a thickness of 5 mm. A tunnel was created in patella and tibial tuberosity with a 5 mm reamer (Fig. 3). One end of the graft was stitched with polyethylene terephthalate 2–0 and anchored on a Beath pin. The pin with the graft was first passed from lateral to the medial side of the tibial tuberosity and then from lateral to medial end of the patella, the ends of which were sutured with a thick non-absorbable suture. We noted the tendon to be in the excess length of 1.5 cm which was resected. Suturing and tightening were done with knee in extension. The knot was formed on the lateral side of the tibial end (Fig. 4). 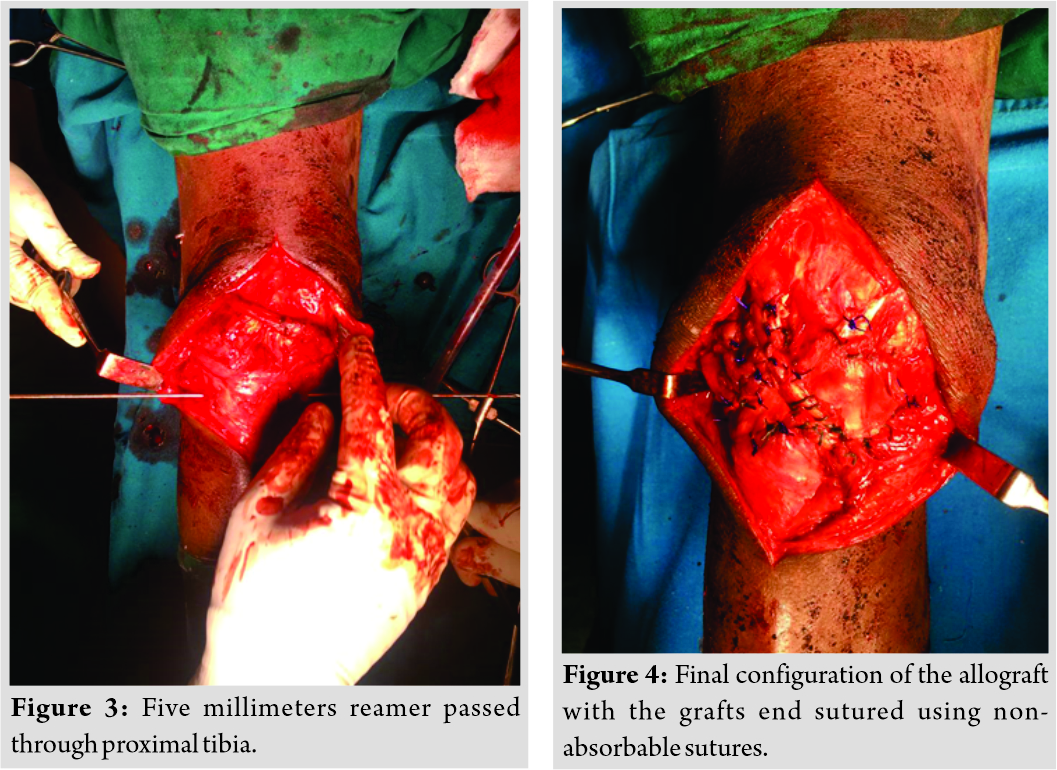 This gave the final structure a figure of 8 configurations (Fig. 5). The stability of the reconstructed tendon was checked under flexion and extension. Patella slid inferiorly during flexion and superiorly during extension. No extensor lag or maltracking was noted. Knee was maintained in extension for 2 weeks with an above-knee slab (Fig. 6). Sutures were removed after 2 weeks. The slab was converted into the cast and maintained for 4 weeks in extension. After 4 weeks, the patient was started on gentle knee mobilization along with quadriceps and hamstring strengthening exercises. The patient had no extensor lag, and he was walking full-weight-bearing with a normal gait at 4 months after surgery. At 3 years follow-up, the patient had full range of painless motion with no signs of infection or activity limitation with normalized Insall-Salvati ratio (Fig. 7).
This gave the final structure a figure of 8 configurations (Fig. 5). The stability of the reconstructed tendon was checked under flexion and extension. Patella slid inferiorly during flexion and superiorly during extension. No extensor lag or maltracking was noted. Knee was maintained in extension for 2 weeks with an above-knee slab (Fig. 6). Sutures were removed after 2 weeks. The slab was converted into the cast and maintained for 4 weeks in extension. After 4 weeks, the patient was started on gentle knee mobilization along with quadriceps and hamstring strengthening exercises. The patient had no extensor lag, and he was walking full-weight-bearing with a normal gait at 4 months after surgery. At 3 years follow-up, the patient had full range of painless motion with no signs of infection or activity limitation with normalized Insall-Salvati ratio (Fig. 7).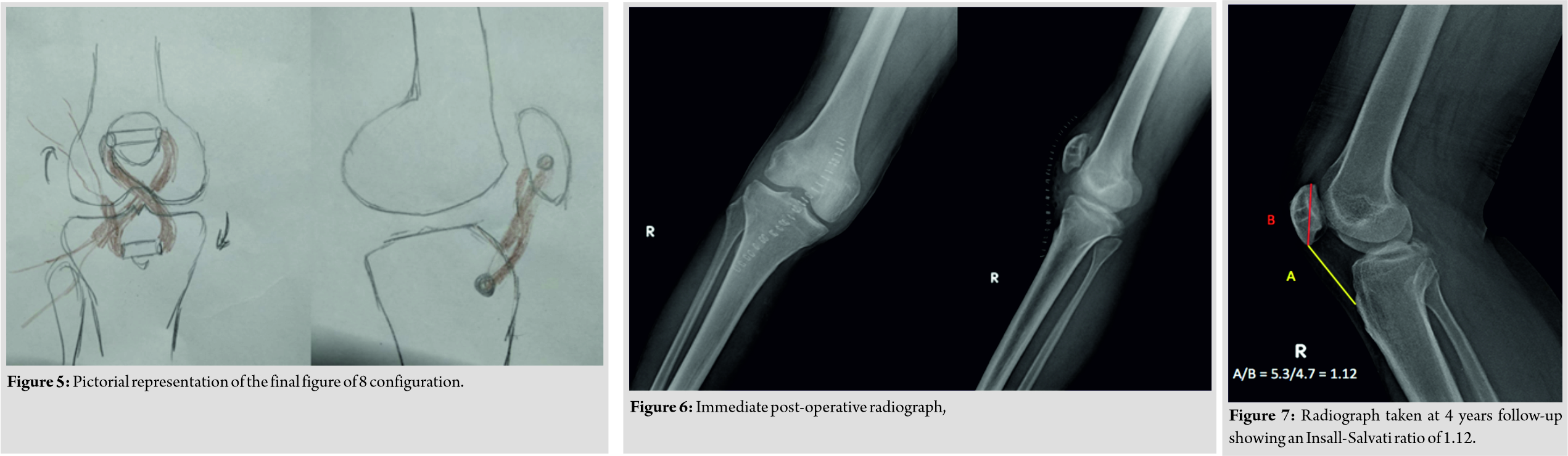
Discussion
Surgery of neglected patellar tendon rupture is challenging due to adhesions, quadriceps atrophy, and proximal patellar migration [6]. Factors determining surgery for these cases are tissue quality, native tissue remnants, comorbidities, and pre-operative activity levels [7]. Tourniquet was avoided as this would have tethered the contracted quadriceps and caused difficulty in achieving patellar height [6]. Cannulated cancellous screws and tensioning device are used to achieve patellar height [8]. We were prepared to use these screws in case the height that would not have been corrected by adequate soft-tissue release. We measured and compared the patellar height with the contralateral side. This was similar to the method mentioned by Harato et al. [8]. Another advantage of not using a tourniquet was reduced post-operative pain. It has been proven that using a tourniquet gives a better surgical field, decreases operative time and blood loss. However, we used spinal anesthesia with fentanyl which helped to reduce blood loss and patient’s pre-operative hemoglobin was an encouraging factor to avoid tourniquet. Quadriceps lengthening is an established procedure done for contracted quadriceps to achieve patellar height. However, this reduces its strength, as noted by cybex testing [9]. This is debilitating in physically active individuals, especially when getting up from squatting position repeatedly. De Faria et al. [10] treated a chronic rupture in two stages. They applied a 3.5 mm Steinmann pin through the proximal third of the patella and gradually increased weights to the traction to get the patella inferiorly. They achieved distal migration of patella with traction which helped in tendon reconstruction. Steinmann pin can cause patella fracture and pin tract infection, in which we were wary of since the patient had sustained a deep cut lacerated wound 6 months back. Considering the patient’s age, the bone quality was questionable; hence, we deferred the use of Steinmann pin. Fixation of the tendoachilles’ allograft with calcaneal bone graft over proximal tibia can be achieved by shaping the calcaneal bone block into 45 degree proximal bevel and inserting it by creating corticotomy followed by screw fixation [7]. However, this technique can cause stress fracture which delays weight-bearing and mobilization. Chronic patellar tendon rupture can be reconstructed using hamstring autografts and augmentation techniques [6, 11]. Augmentation with synthetic materials, though an excellent method, is expensive. A 2019 meta-analysis concluded that there were no significant differences in functional outcomes, failures, infections, and revision reconstruction surgeries between allograft and synthetic material group [12]. Autologous hamstring grafts though easy to harvest, cause donor site morbidity, saphenous nerve injury [13], and also reduce hamstring muscle strength which affects squatting [14]. We were concerned about the scar over the anterior aspect of the knee and the chance of infection in case of repeated surgeries like implant removal. Falconiero and Pallis [9] corrected the patellar height using a suprapatellar wire which was removed after 8 weeks. Interference screw gives good fixation of the graft. However, it can cut the graft [10] or cause knee pain necessitating its removal [15]. These were the reasons why we avoided using metallic implants. To the best of our knowledge, this is the first reported case where a patellar tendon reconstruction is done without implants or synthetic augmentation. Allograft is a good alternative to autograft provided, it is procured from a good tissue bank to avoid infection and compromise in tissue quality. Results of this technique are excellent, provided strict post-operative rehabilitation is followed.
Conclusion
Neglected patellar tendon rupture requires reconstruction surgery as the end-to-end repair is difficult due to poor tissue quality. It requires adequate soft-tissue release to achieve patellar height. Allograft without augmentation or metallic implants gives excellent results provided that a strict rehabilitation protocol is followed.
Clinical Message
Neglected patellar tendon rupture cases can be treated with allograft through transosseous tunnels without the use of synthetic augmentation or metallic implants giving excellent clinical and radiological results.
References
1. Pengas IP, Assiotis A, Khan W, Spalding T. Adult native knee extensor mechanism ruptures. Injury 2016;47:2065-70.
2. Waligora AC, Johanson NA, Hirsch BE. Clinical anatomy of the quadriceps femoris and extensor apparatus of the knee. Clin Orthop Relat Res 2009;467:3297-306.
3. Zernicke RF, Garhammer JO, Jobe FW. Human patellar-tendon rupture. J Bone Joint Surg Am 1977;59:179-83.
4. Phillips K, Costantino TG. Diagnosis of patellar tendon rupture by emergency ultrasound. J Emerg Med 2014;47:204-6.
5. Core M, Anract P, Raffin J, Biau DJ. Traumatic patellar tendon rupture repair using synthetic ligament augmentation. J Knee Surg 2019;33:804-9.
6. Tsitskaris K, Subramanian P, Crone D. Neglected patellar tendon rupture. Reconstruction using semitendinosus-gracilis tendon grafts and Fiber Wire augmentation. JRSM Short Rep 2013;4:2042533313490286.
7. Ares O, Lozano LM, Medrano-Nájera C, Popescu D, Martínez-Pastor JC, Segur JM, et al. New modified Achilles tendon allograft for treatment of chronic patellar tendon ruptures following total knee arthroplasty. Arch Orthop Trauma Surg 2014;134:713-7.
8. Harato K, Kobayashi S, Udagawa K, Iwama Y, Masumoto K, Enomoto H, et al. Surgical technique to bring down the patellar height and to reconstruct the tendon for chronic patellar tendon rupture. Arthrosc Tech 2017;6:e1897-901.
9. Falconiero RP, Pallis MP. Chronic rupture of a patellar tendon: A technique for reconstruction with Achilles allograft. Arthroscopy 1996;12:623-6.
10. de Faria JL, de Barros Carvalho M, Marques AC, Cavanellas NT, de Sousa EB, Barretto JM, et al. Surgical treatment for chronic rupture of the patellar tendon performed in 2 stages. Arthrosc Tech 2019;9:e159-66.
11. Samagh SP, Huyke FA, Buchler L, Terry MA, Tjong VK. Treatment of a neglected patellar tendon rupture with a modified surgical technique: Ipsilateral semitendinosus autograft reconstruction with suture tape augmentation. Case Rep Orthop 2018;2018:2037638.
12. Deren ME, Pannu TS, Villa JM, Firtha M, Riesgo AM, Higuera CA. Meta-analysis comparing allograft to synthetic reconstruction for extensor mechanism disruption after total knee arthroplasty. J Knee Surg 2019.
13. Sharaby MM, Alfikey A, Alhabsi IS, Al-Ghannami S. No difference in sensory outcome between vertical and oblique incisions for hamstring graft harvest during ACL reconstruction. Knee Surg Sports Traumatol Arthrosc 2019;27:146-52.
14. Nomura Y, Kuramochi R, Fukubayashi T. Evaluation of hamstring muscle strength and morphology after anterior cruciate ligament reconstruction. Scand J Med Sci Sports 2015;25:301-7.
15. Kramer DE, Kalish LA, Kocher MS, Yen YM, Micheli LJ, Heyworth BE. Complications of bioabsorbable tibial interference screws after anterior cruciate ligament reconstruction in pediatric and adolescent athletes. Orthop J Sports Med 2020;8:2325967120904010.
 |
 |
 |
 |
| Dr. Sharath Kittanakere Ramanath | Dr. Rahul Hemant Shah | Dr. Sandesh Patil | Dr. Shreyas Umesh |
| How to Cite This Article: Ramanath SK, Shah RH, Patil S, Umesh S. Reconstruction of Neglected Patellar Tendon Rupture using Tendoachilles’ Allograft with Transosseous Tunnels: A Case Report. Journal of Orthopaedic Case Reports 2020 August;10(5): 27-30 |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com




