[box type=”bio”] Learning Point of the Article: [/box]
Knowledge about seropositivity load among patients enables the doctors to improve their safety measures and disease prevention strategy through appropriate planning and approach.
Case Report | Volume 10 | Issue 5 | JOCR August 2020 | Page 48-52 | Ravinder Kumar Banga, Jagdeep Singh, Sorabh Garg, Swarnesh Bhaskaran, Anshul Dahuja. DOI: 10.13107/jocr.2020.v10.i05.1834
Authors: Ravinder Kumar Banga[1], Jagdeep Singh[2], Sorabh Garg[2], Swarnesh Bhaskaran[2], Anshul Dahuja[2]
[1]Department of Orthopaedics, Government Medical College and Hospital, Patiala, Punjab, India,
[2]Department of Orthopaedics, Guru Gobind Singh Medical College and Hospital, Faridkot, Punjab, India.
Address of Correspondence:
Dr. Sorabh Garg,
Department of Orthopaedics, Guru Gobind Singh Medical College and Hospital, Faridkot, Punjab, India.
E-mail: sorgag@gmail.com
Abstract
Introduction: Exposure to blood and blood-borne viruses is major concern for orthopedic surgeons and operation theater staff because of constant exposure to sharp instruments and bodily fluids. The objective of this study was to assess the burden of seropositive patients in the orthopedic department of tertiary care hospitals in North India.
Materials and Methods: This retrospective study was carried out in author’s institute on indoor patients admitted from January 2015 to December 2017. A total of 8914 patients were included in the study and relevant clinical data were collected for seropositivity of hepatitis B virus (HBV), hepatitis C virus (HCV), and human immunodeficiency virus (HIV) in patients admitted in the orthopedic emergency department. These patients were routinely tested for seropositivity before undergoing various surgical procedures.
Results: A total of 8914 patients included in the study, out of which 7193 (80.7%) were male and 1721 (19.3%) were female. Out of total patients, 262 (2.9%) were found to be seropositive. Out of these patients, 31 (11.8%) were found to be positive for HIV, 190 (72.5%) for HCV, and 41(15.7%) for HBV. About 35.90% of patients with highest prevalence of seropositivity were truck drivers.
Conclusion: HIV, HBsAg, and HCV are common in this region with HCV infection being the major concern in Punjab. Screening for viral markers will help in adequate pre-operative planning, timely precautions, and immediate post-exposure prophylaxis in case of contact with blood or body fluids of seropositive patients.
Keywords: Seropositivity, Tertiary care hospitals, Orthopedic surgery.
Introduction
In health-care setups, the occupational exposure of blood-borne viruses is a major cause of concern. Surgeons and operation theater staff are at particular risk especially orthopedic surgeons, nurses, technicians and cleaning persons working in various health institutions because of continuous handling of sharp instruments like pins, wires, and blood. Blood-borne viruses of particular concern are human immunodeficiency virus (HIV), hepatitis B virus (HBV), and hepatitis-C virus. Health care workers (HCWs) can get exposed to these viruses through needlestick injury (NSI) and other injuries related to blood and other body fluids. The World Health Organization (WHO) estimates that more than 2 million injuries causes about 66,000 HBV, 16,000 hepatitis C virus (HCV), and about 1000 HIV infections among 35 million HCWs each year[1] (Rapiti et al., 2003). An Indian study found seroprevalance of HIV in patients attending emergency department to be 5.75% [2](Devi et al., 2010). Seropositivity rates for indoor patients were 5.85% for HBsAg 2.39% for anti-HCV antibodies, respectively[3] (Arif, 2015). Hence, there is general emphasis for the use of universal precautions for all health professionals, particularly those who work in emergency department, so as to limit occupational exposure. Screening for HIV, HCV, and HBV is common practice in surgical centers [4-7](McGowan, 2012; Mantha, 2005; Minz, 2010; Albrecht, 2012). This is particularly important in Indian setup with estimated number of people living with HIV (PLHIV) which is 0.27% of total population as in 2012 according to the National AIDS Control Organization (NACO) guidelines 2016. The prevalence of HCV and HBV is estimated to be 1% and 3.7%, respectively, according to the National Centre for Disease Control report 2014. The pre-operative screening of surgical patients may serve the following functions[8] (Ahmed and Bhattacharya, 2013). First, it will guide the health-care staff to use enhanced protective measures while handling seropositive patients. Special O.T. arrangements can be made before the surgery and it will be helpful in proper disposal of seropositive waste generated during the course of treatment. Finally, screening will guide for future treatment of seropositive patients. The present study aims to find out the incidence of seropositivity in trauma patients attending orthopedic emergency department of tertiary care hospitals and discuss its implications to health-care professionals working there and measures for preventing transmission of these infections to health-care individuals.
Materials and Methods
This retrospective study was carried out in author’s institute. The clinical records of the indoor patients admitted from January 2015 to December 2017 (8914 patients) were included in the study and relevant clinical data were collected. These data included seropositivity of HBV, HCV, and HIV in patients admitted in the orthopedic emergency department. The data also included age, sex, occupation, surgical procedure conducted, socioeconomic status, drug abuse history, medical history, and central registration number of the patients. Patients admitted for diagnostic purposes and whose treatment was decided to be conservative which were excluded from the study. These patients were routinely tested for seropositivity before undergoing various surgical procedures.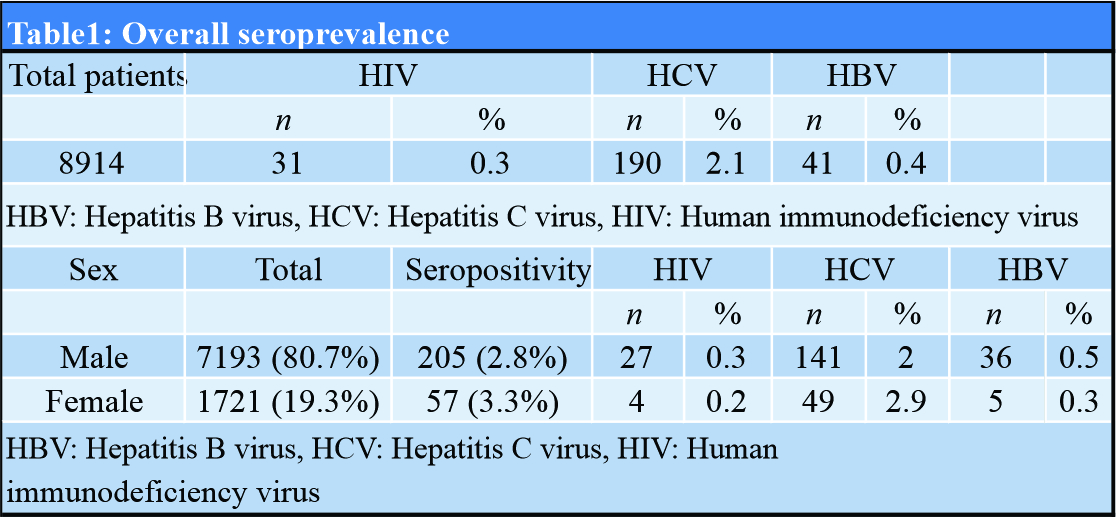
Serum samples were screened for HBV, HCV, and HIV infection using HEPA CARD, HCV TRI-DOT, and HIV TRI-DOT rapid card test, respectively. All these rapid card tests had 100% sensitivity. Rapid tests for viral marker detection are an easy, cost-effective, and time saving method with accuracy comparable to standard methods[9] (Allain and Lee, 2005). The patients having positive rapid card test were confirmed by ELISA for HIV. In case of HIV, two tests were conducted before labeling the patients positives per NACO guidelines. The data were recorded and analyzed.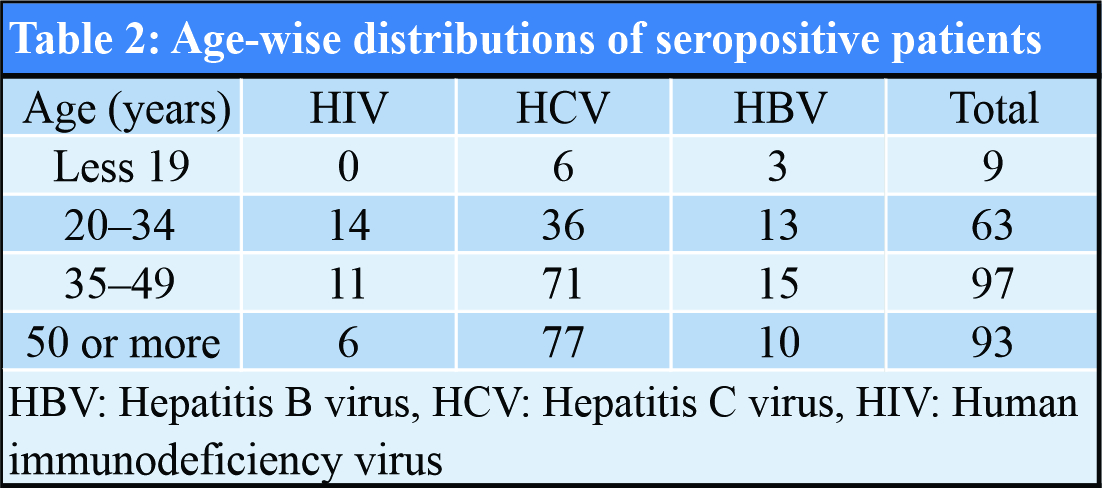
Results
A total of 8914 patients were included in the study, out of which 7193 (80.7%) were male and 1721 (19.3%) were female. Out of total patients, 262 (2.9%) were found to be seropositive. Out of 262 patients, 31 (11.8%) were found to be positive for HIV, 190 (72.5%) for HCV, and 41 (15.7%) for HBV. Details of data are shown in Table 1. It has been observed that 190 (72.5%) of the seropositive case had an age above 35 or more (Table 2). Table 3 shows the occupation of patients included in the study with highest prevalence of seropositivity found in drivers 35.4% (110/311 patients) followed by self-employed 2.5% (47/1861 patients) followed by farmer (1.7%) and laborers (1.5%). This prevalence could be attributed to high-risk behavior of unsafe sex associated with such occupation, especially in drivers, level of awareness education, and unsafe medical practice in rural areas such as syringe sharing and intravenous (IV) drug abuse.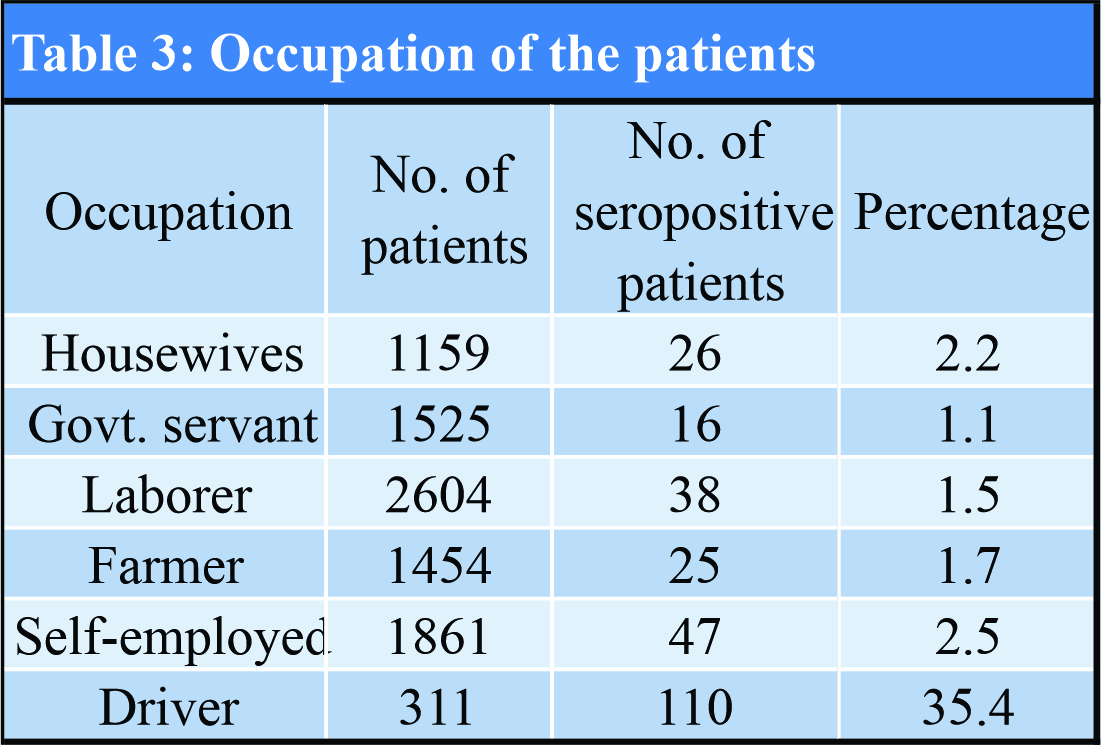
Discussion
Routine performance of various screening pre-operative blood tests before elective surgery is a matter of debate. More often these investigations lead to inappropriate use of financial resources without making much difference to the clinical outcome and patient management [10](Phoenix, 2012). However, the issue of routine testing for blood-borne viruses (HIV, HCV, and HBsAg) has not been appropriately discussed in literature and no clear-cut guidelines exist for using them [11](Kumar and Srivastava, 2011). The arguments existing against the routine use of screening are greater emphasis given on seropositivity detection with little importance given for its subsequent management in the patients. There are also issues regarding sensitivity of these screening investigations and window period negativity[8] (Ahmed and Bhattacharya, 2013). Screening for blood-borne viruses gains particular importance in tertiary care settings which may be receiving a higher load of seropositive patients due to various reasons. These viral infections are associated with many serious and end-stage clinical conditions causing referral of such patients to tertiary care hospitals. There may be less preference for seropositive surgical patients at peripheral centers due to attitude of surgeons in the periphery to refer seropositive patients and higher costs involved at private hospitals leading to preferential use of tertiary government sector utilities by such patients. This is of particular concern to surgeons and health-care staff working in tertiary care hospitals, who have a more exposure to such patients and are at higher risk for such infections while handling these cases. Seropositivity in our study for HIV was found to be 0.3% which is equivalent to the community prevalence of HIV in India. Routine screening for HIV is recommended by previous studies [12](Odigie and Siminialayi, 2010) and is also found to be useful by the patients[13] (Drayton et al., 2010). The NACO guidelines are followed for all the patients undergoing HIV testing. It could help in early detection of infection and management according to the stage and viral load and before the onset of complications and AIDS. Seropositivity for HCV and HBV was found to be 2.1% and 0.4% in our study which could be due to unsafe practices in the rural areas with needle sharing, IV drug abuse. Community prevalence is higher for HCV out of which 0.5%–1.5% in India with the predominant modes of transmission of are likely to be unsafe therapeutic injections and blood transfusions [14](Puri et al., 2014). [15]Jindal et al., 2015, documented that 6.71% of patients to be anti-HCV positive. The most common risk factors noted were unsafe medical procedures (47.6%), which included history of therapeutic injections and major/minor surgeries followed by blood transfusion in 30.2% and dental procedures in 22.2%. Studies have also depicted that intravenous drug abuse is major risk factor in the occurrence of HCV infection in Punjab because of repeatedly sharing of syringes [16](Ambekar and Tripathi, 2008). Another study conducted by Sood et al. in the general population of Punjab showed that the prevalence of HCV was 5.2%. This finding emphasizes important role of pre-operative testing for HCV infection in patients[17] (Sood et al., 2012). Routine screening for viral markers is justifiable and recommended in resource rich and developed countries[8] (Ahmed and Bhattacharya, 2013), where there is a secondary aim of case detection and early treatment. However, screening in resource limited countries like India can be of equal importance. Early detection and treatment of seropositive cases will prevent end-stage disease and its complications leading to decreased economic burden in the future on the society. Early detection will help in reduction of further spread of disease. There would be additional advantage of this approach to health-care professionals including theater staff. Prior knowledge of seropositivity will allow timely application of suitable precautions such as protective eyewear and water proof gowns. Moreover, the health-care professionals could start post-exposure prophylaxis (PEP) immediately in case of an exposure. The role of universal precautions is utmost as prevention is always better than cure. There is a need for regular trainings on universal precautions and stress on following for prevention from these dreaded viral infections. It has been documented that HCWs from developing countries show suboptimal adherence to “universal precautions” and documentation of exposures and their awareness about PEP is poor [18-19](Gounden and Moodley, 2002; Chogle et al., 2002). Training programs need to be organized constantly, especially in countries like India where the staff turnover, especially that of nurses, is very high and these new HCWs might be completely alien to using new and safer devices. Literature findings suggest that surgery residents are at greatest risk. For new residents, additional procedural skill sharp instruments may decrease NSI. Resident education and training during orientation may reduce risk. However, a majority of residents felt comfortable in procedures with instruments causing injury [20](Lee, 2014). Despite resident-reported mastery, caution to avoid both overconfidence and decreased attention to NSI risk is warranted. PEP for HIV and HBV exposure should be done according to NACO guidelines given by Ministry of Health and Family Welfare [21](Manoj et al., 2011). HBsAg prophylaxis id given to all the health-care staff and the PEP is recommended accordingly in the form of hepatitis B immune globulin and/or vaccine is offered for HBV exposure. In case of HCV, there is dilemma as to the benefit in cases who have needle exposure and is not given routinely [22] (Panlilio et al., 2001). Regarding limitation in this study, we collected the data of two tertiary care centers belonging to one demographic region. To provide more accurate and reliable data on patients with seropositivity load in orthopedics in this particular region of India, further larger studies should be carried out which should include all the departments of all tertiary care hospitals and other district hospitals. Another limitation is that we did not correlate the effect of seropositivity on clinical outcome in terms of wound healing or infections. Accordingly, future studies should be done to find its correlation with larger sample size.
Conclusion
HCV positivity is major burden in health-care system of Punjab which needs to tackle down with definitive solutions, to confine this problem .There is a need for provision of education and facilities in the peripheral institutions so that workload of seropositive patients can be shared. Blood sampling being an integral part of workup before surgery should routinely include screening for viral markers. It will help in adequate pre-operative planning, timely precautions, and immediate PEP in case of contact with blood or body fluids of seropositive patients. In addition, there will be a chance for early case detection and its subsequent management.
Clinical Message
Seropositivity load in tertiary care hospitals in North India is a major concern, with HCV infection being distributed avidly in Punjab. Seropositivity helps screen patients for viral markers and plan corresponding pre-operative and post-operative measures in case of contact with body fluids of such patients.
References
1. Rapiti E, Prüss-Üstün A, Hutin Y. Sharps Injuries: Global Burden of Disease from Sharps Injuries to Health-care Workers, WHO Environmental Burden of Disease Series. Geneva: World Health Organization; 2003.
2. Devi P, Arora U, Yadav S, Malhotra S. Seroprevalence of HIV infection among the patients attending various emergency departments in a tertiary care hospital. Indian J Sex Transm Dis AIDS 2010;31:27-9.
3. Arif SH, Afrose R, Khan AI, Akram M, Singh SK. Seropositivity rates for hepatitis B and C viruses in indoor patients of a tertiary care centre of Northern India. Int J Curr Microbiol Appl Sci 2015;1:243-7.
4. McGowan DR, Norris JM, Smith MD, Lad M. Routine testing for HIV in patients undergoing elective surgery. Lancet 2012;380:e5.
5. Mantha S, Roizen MF, Madduri J, Rajender Y, Naidu KS, Gayatri K. Usefulness of routine preoperative testing: A prospective single-observer study. J Clin Anesth 2005;17:51-7.
6. Minz RW, Singh S, Varma S, Mathuria SN, Aggrawal R, Sehgal S. Relevance of opt-out screening for HIV in emergency and pre-surgery patients in a tertiary care centre in Northern India: A pilot study. Indian J Pathol Microbiol 2010;53:287-9.
7. Albrecht E, Frascarolo P, Meystre-Agustoni G, Farron A, Gilliard N, Darling K. An analysis of patients’ understanding of routine preoperative blood tests and HIV screening. Is no news really good news? HIV Med 2012;13:439-43.
8. Ahmed R, Bhattacharya S. Universal screening versus universal precautions in the context of preoperative screening for HIV, HBV, HCV in India. Indian J Med Microbiol 2013;31:219.
9. Allain JP, Lee H. Rapid tests for detection of viral markers in blood transfusion. Expert Rev Mol Diagn 2005;5:31-41.
10. Phoenix GK, Elliott T, Chan JK, Das SK. Preoperative blood tests in elective general surgery: Cost and clinical implications. J Perioper Pract 2012;22:282-8.
11. Kumar A, Srivastava U. Role of routine laboratory investigations in preoperative evaluation. J Anaesthesiol Clin Pharmacol 2011;27:174-9.
12. Odigie JO, Siminialayi IM. Perception and attitude of theatre staff to preoperative HIV testing at the University of Port Harcourt teaching hospital. Asian Pac J Trop Med 2010;3:145-7.
13. Drayton R, Keane F, Prentice E. Patients’ attitudes towards increasing the offer of HIV testing in primary and secondary care. Int J STD AIDS 2010;21:563-6.
14. Puri P, Anand AC, Saraswat VA. Consensus statement of HCV task force of the Indian national association for study of the liver (INASL). Part I: Status report of HCV infection in India. J Clin Exp Hepatol 2014;4:106-16.
15. Jindal N, Bansal R, Grover P, Malhotra R. Risk factors and genotypes of HCV infected patients attending tertiary care hospital in North India. Indian J Med Microbiol 2015;33:189-90.
16. Ambekar A, Tripathi BM. Size Estimation of Injecting Drug Use in Punjab and Haryana. Geneva: UNAIDS; 2008.
17. Sood A, Sarin SK, Midha V, Hissar S, Sandeep N, Bansal P, et al. Prevalence of hepatitis C virus in a selected geographical area of Northern India: A population based survey. Indian J Gastroenterol 2012;31:232-6.
18. Gounden YP, Moodley J. Exposure to human immunodeficiency virus among healthcare workers in South Africa. Int J Gynaecol Obstet 2002;69:265-70.
19. Chogle NL, Chogle MN, Divatia JV, Dasgupta D. Awareness of post exposure prophylaxix guidelines against occupational exposure to HIV in Mumbai hospital. Natl Med J India 2002;15:69-72.
20. Lee JJ, Kok SH, Cheng SJ, Lin LD, Lin CP. Needle stick and sharp injuries among dental health workers at a university hospital. J Formos Med Assoc 2014;113:227-33.
21. Shevkani M, Kavina B, Kumar P, Purohit, H, Nihalani U, Shah A. An overview of post exposure prophylaxis for HIV in health care personals: Gujarat scenario. Indian J Sex Transm Dis AIDS 2011;32:9-13.
22. Panlilio AL, Cardo DM, Grohskopf LA, Heneine W, Ross CS. Updated U.S. Public health service guidelines for the management of occupational exposures to HBV, HCV, and HIV and recommendations for postexposure prophylaxis. MMWR Recomm Rep 2001;50:1-52.
 |
 |
 |
 |
 |
| Dr. Ravinder Kumar Banga | Dr. Jagdeep Singh | Dr. Sorabh Garg | Dr. Swarnesh Bhaskaran | Dr. Anshul Dahuja |
| How to Cite This Article: Banga RK, Singh J, Garg S, Bhaskaran S, Dahuja A. Seropositivity Load in Orthopedic Surgery at Tertiary Care Hospitals in North India – An Observational Study. Journal of Orthopaedic Case Reports 2020 August;10(5): 48-52. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com




