[box type=”bio”] Learning Point of the Article: [/box]
En bloc excision of ventral scapular osteochondroma helps get rid of pseudo-winging of the scapula.
Case Report | Volume 10 | Issue 5 | JOCR August 2020 | Page 69-72 | S P Barnawal, B S Gandhi, A Rathod. DOI: 10.13107/jocr.2020.v10.i05.1844
Authors: S P Barnawal[1], B S Gandhi[1], A Rathod[1]
[1]Department of Orthopedics, Jawaharlal Institute of Postgraduate Medical Education and Research, Pondicherry, India.
Address of Correspondence:
Dr. Satish Prasad Barnawal,
Department of Orthopedics, Jawaharlal Institute of Postgraduate Medical Education and Research, Pondicherry, India.
E-mail: satishprasadbarnawal@gmail.com
Abstract
Introduction: Osteochondroma is the most common benign tumor of bone. Scapula is a very rare site for its occurrence.
Case Report: A 6-year-old male presented with swelling over the left scapular region for 3 months, which was insidious in onset and gradually progressing. There was a single swelling of approximately 3 × 3 × 2 cm3 over medial border of the left scapula. It was hard in consistency with well-defined margin and irregular surface, non-tender, immobile, arising for the underlying bone, and non-adherent to skin. There was pseudo-winging of scapula. The patient was referred with an anteroposterior view radiograph and a computed tomography scan. A working diagnosis of ventral scapular osteochondroma was made. Excision of lesion was done in prone position. There was no pseudo-winging post-excision. Osteochondroma is rare for scapula. Further, pseudo-winging of scapula is seldom.
Conclusion: Prone position with internal rotation of shoulder can make the surgery easy. Excision of the tumor helps get rid of pseudo-winging.
Keywords: Prone position, pseudo-winging, ventral scapular osteochondroma.
Introduction
Osteochondroma is the most common benign bone tumor [1]. While scapula is rarely involved, osteochondroma is the most common tumor of scapula [2]. About 4.0–4.6% of scapula tumors are osteochondroma [3]. When it occurs in scapula, it is usually ventral [4]. However, literature is scanty about ventral scapular osteochondroma (VSO) [5]. VSO is typically painless. Mechanical effect of tumor may cause pseudo-winging and pain [6]. Pertaining to area of affection, diagnosis of VSO is not always easily made, as a palpable mass may not be easily appreciated [4].
Case Report
A 6-year-old male student presented to our outpatient clinic with swelling over the left scapular region for 3 months, which was insidious in onset and gradually progressing. There was no history of pain, trauma, fever, swelling elsewhere in the body, or decreased range of motion. There was no functional limitation. The past and birth history were insignificant. There was no history of similar illness in family members. He was not allergic to medication he had taken. His developmental milestones were comparable with his peer group. He was immunized as per his age.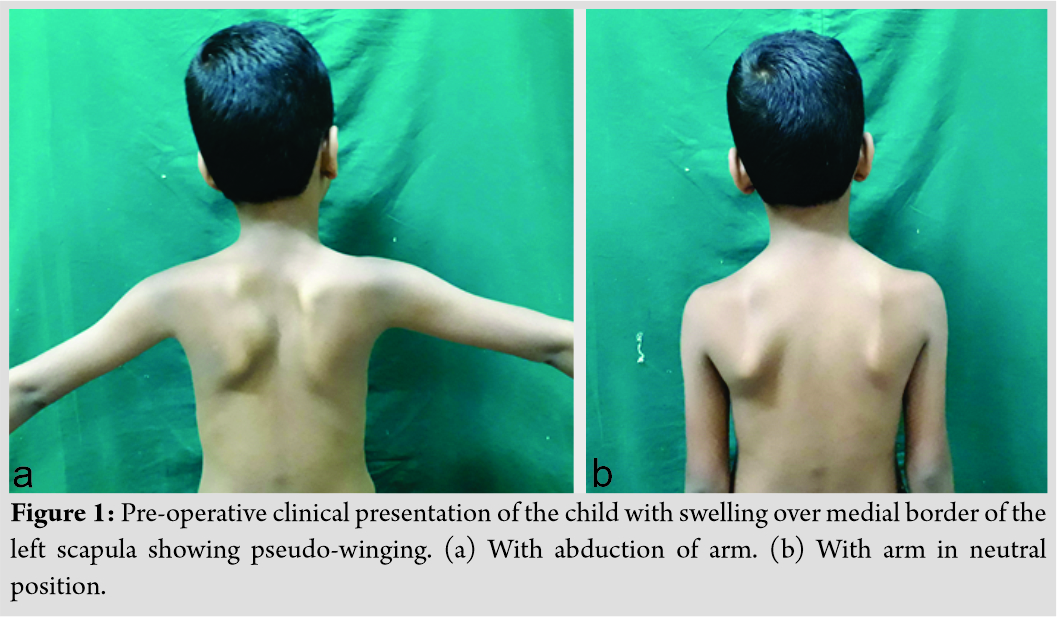
On examination, there was a single swelling of approximately 3 × 3 × 2 cm3 over medial border of the left scapula. Overlying skin was normal. It was hard in consistency with well-defined margin and irregular surface. It was non-tender, immobile, arising from underlying bone, and non-adherent to skin. It was non-fluctuant and non-compressible. Pseudo-winging of scapula was present as shown in (Fig. 1) with wall test because there was no tenderness, neurological examination was within normal limit, and range of movement in cervical spine along with extremity was normal. His activity of daily living was not affected. There were no signs of compression of nerves, vessels, or lymphatic system. No lymph nodes were palpable. Distal neurovascular status was within normal limit. There was no audible or palpable crepitus. Range of movement of the shoulder and cervical spine was normal. The patient was referred with an anteroposterior view radiograph and a computed tomography (CT) scan. No further radiological workup was attempted in view of radiation exposure. The CT scan demonstrated a well-corticated bony excrescence arising from ventral surface of the left lower part of body of scapula near inferior angle suggestive of exostosis (Fig. 2).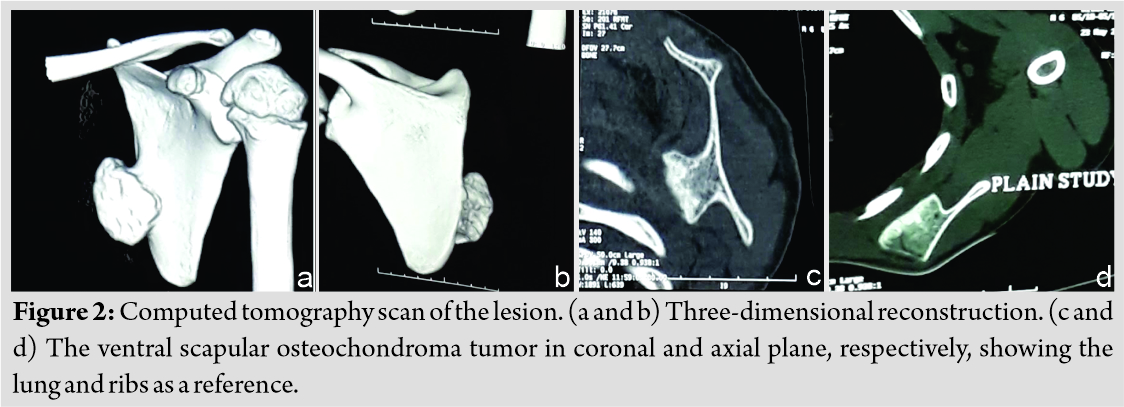 A working diagnosis of VSO was made. Excision of lesion was principally done for mechanical reasons and secondarily for pathologic assessment. It was done under general anesthesia with patient in prone position. Shoulder was rotated internally, which helped lift medial border of scapula. A 5 cm incision was given along inferomedial border. A muscle splitting approach of trapezius and rhomboid was used. En bloc excision of VSO was done. To prevent complications, meticulous dissection was done and hemostasis was obtained. It was removed as a single block to prevent seeding. No remnants were left. Sessile VSO of 3 × 3 × 1 cm3 was sent for histopathological assessment. The tumor was hard. It was composed of bone covered by a thick cartilage cap, as shown in (Fig. 3, 4). Thorough irrigation was done and the wound was closed in standard fashion. The surgery was over in 45 min.
A working diagnosis of VSO was made. Excision of lesion was principally done for mechanical reasons and secondarily for pathologic assessment. It was done under general anesthesia with patient in prone position. Shoulder was rotated internally, which helped lift medial border of scapula. A 5 cm incision was given along inferomedial border. A muscle splitting approach of trapezius and rhomboid was used. En bloc excision of VSO was done. To prevent complications, meticulous dissection was done and hemostasis was obtained. It was removed as a single block to prevent seeding. No remnants were left. Sessile VSO of 3 × 3 × 1 cm3 was sent for histopathological assessment. The tumor was hard. It was composed of bone covered by a thick cartilage cap, as shown in (Fig. 3, 4). Thorough irrigation was done and the wound was closed in standard fashion. The surgery was over in 45 min.
He was given prophylactic intravenous ceftriaxone two doses post-surgery. The child was given arm sling for a week. Range of movement exercises of shoulder joint was started then. Wound inspection in post-operative day 4 and 8 was clean. Suture removal was done in the 14th day of the procedure. The child had an uneventful post-operative period.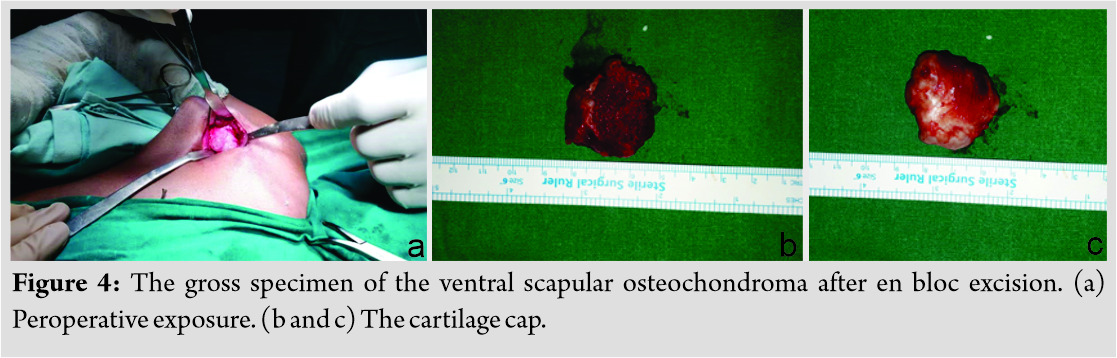
Histopathological evaluation stated that it was a tumor with a cartilage cap composed of chondrocytes in a growth plate-like pattern with an overlying fibrous perichondral and underlying fragments of trabeculae bone and bone marrow elements consistent with diagnosis of osteochondroma (Fig. 5). The cartilage cap was 0.3 cm thick on histopathological assessment. He has been free of symptoms. He has full and painless range of movements and the complete disappearance of pseudo-winging (Fig. 6). There are not any signs of recurrence so far. It has been 20 months after en bloc excision. Our plan is to follow up till skeletal maturity.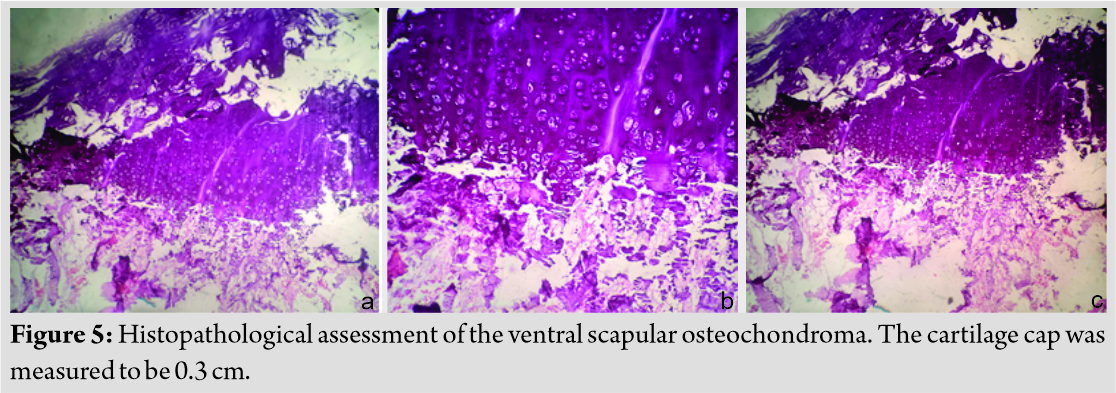
Discussion
In a study of 1853 cases of bone cancer, scapula had a share of 3.6% [7]. Osteochondroma is a type of benign cartilaginous tumor [8]. It is the most common benign bone tumor [9]. It commonly involves metaphyses of long bones around knee and proximal humerus [10]. Such parts make up to 90% of occurrence site [5]. Flat bones such as scapula and pelvis are rare sites [5]. Osteochondroma has involved scapula in 3.0–4.6% of all reported cases and comprise 14.4% of all tumors of scapula [11]. It is the most common benign primary bone tumor of scapula [12].
Clinical Presentation
It affects mainly male in bone growth periods [13]. VSO is usually first seen at 6–20 years of age [10]. The size increases as skeleton grows [11]. Tumor growth typically ceases after closure of physis [8]. VSO is a rare cause of scapular pseudo-winging [3]. The child had visited our clinic for the same reason. VSO causing prominence of medial border is shown in Fig. 1. Further, Fig. 6 demonstrates its disappearance after excision. VSO is usually painless. Patients may present with complaints such as pain, decreased range of movement, and crepitus [14]. Snapping scapula and cosmetic deformities are some of other presentations [5]. Mechanical irritation against rib cage often leads to bursa formation [13]. Fracture of bony stalk of tumor and nerve impingement may occur [14]. These complications along with bursal inflammation may cause discomfort [8]. It causes snapping usually in adolescence or early adulthood [15]. Our patient had none of these symptoms. He had visited our clinic for pseudo-winging alone.
Pathology
Osteochondroma is a developmental physeal growth defect [15]. VSO may be a sessile or pedunculated [14]. Many causes of scapulothoracic bursitis have been described including VSO [16].
Diagnosis
VSO is diagnosed frequently by clinical assessment and imaging, whereas confirmation is done by histopathologic evaluation [17]. VSO may be difficult to identify clinically pertaining to its location. One may miss it on plain radiographs [9]. CT or magnetic resonance imaging (MRI) helps establish a diagnosis [16]. CT scan helps in characterizing lesion and planning treatment. MRI is usually reserved for malignant transformation suspicion [14]. MRI aids in measurement cartilaginous cap thickness. A cap thinner than 1 cm usually indicates a benign lesion. Thickness of more than 2 cm generally relates to malignant change [2]. A cartilaginous cap with thickness <1 cm in biopsy indicates a benign condition, whereas a cap thicker than 2 cm should raise concern for malignant transformation [5]. In our case, the cartilaginous cap thickness was 0.3 cm.
Treatment
Different resection techniques are described for VSO. The consensus is removal whole lesion with its stalk, if present [8]. En bloc resection is indicated when lesion is large or when it produces symptoms [9]. Patients respond well to removal of lesions [9]. Surgical resection of VSO helps relieve symptoms [15]. Excision can be done either by open means or arthroscopically [6]. We had done en bloc excision by giving cosmetically superior 5 cm incision. There is no universal position. Whereas lateral position has been described, we found prone position more comfortable for approach. Further, internal rotation of the shoulder joint helped make the tumor prominent.
Prognosis and complications
Prognosis of single lesion is excellent [2]. Relapse is rare but occurs on leaving unclear resection margins [13]. Risk of malignant transformation is 1–2% but increases in multiple lesions [4]. Malignant transformation is estimated approximately 1% for solitary and up to 5% for multiple lesions [1]. Sarcomatous degeneration has been reported in hereditary multiple exostoses [13]. The child had a single lesion so we expect no recurrence. Growth after maturity is indicative of malignant transformation [12]. Further, cartilage cap thickness >2 cm is worrisome for malignant transformation [3]. Other signs include stippled calcification in cap, increase in size after skeletal maturity, and sudden increase in pain [17]. The histopathological assessment measured cartilaginous cap to be 0.3 cm in our patient.
Conclusion
Osteochondroma is rare for scapula. Further, pseudo-winging of scapula due to VSO is seldom. Prone position with internal rotation of shoulder can make the surgery easy.
Clinical Message
Excision of the VSO helps gets rid of pseudo-wining.
References
1. Ogawa K, Inokuchi W. Solitary osteochondroma of the ventral scapula associated with large bursa formation and pseudowinging of the scapula: A case report and literature review. Case Rep Orthop 2018;2018:1-7.
2. Orth P, Anagnostakos K, Fritsch E, Kohn D, Madry H. Static winging of the scapula caused by osteochondroma in adults: A case series. J Med Case Rep 2012;6:363.
3. Flugstad NA, Sanger JR, Hackbarth DA. Pseudo-winging of the scapula caused by scapular osteochondroma: Review of literature and case report. Hand 2015;10:353-6.
4. Clarke DO, Crichlow A, Christmas M, Vaughan K, Mullings S, Neil I, et al. The unusual osteochondroma: A case of snapping scapula syndrome and review of the literature. Orthop Traumatol Surg Res 2017;103:1295-8.
5. Chun D, Cho J, Choi IH, Yi Y, Kim JY, Kim JH, et al. Osteochondroma of ventral scapula associated with chest pain due to rib cage compression: A case report. Medicine (Baltimore) 2018;97:e0510.
6. Çıtlak A, Akgün U, Bulut T, Aslan C, Mete BD, Şener M. Subacromial osteochondroma: A rare cause of impingement syndrome. Int J Surg Case Rep 2015;6:126-8.
7. Khan Z, Gerrish AM, Grimer RJ. An epidemiological survey of tumour or tumour like conditions in the scapula and periscapular region. SICOT J 2016;2:34.
8. Alatassi R, Koaban S, Almugebel I, Alshehri A. Scapular osteochondroma with winging: A case report. Int J Surg Case Rep 2018;45:138-42.
9. Sivananda P. Osteochondroma of the ventral scapula causing scapular static winging and secondary rib erosion. J Clin Diagn Res 2014;8:LD03-5.
10. Gökkus K. Osteochondromas originating from unusual locations complicating orthopedic discipline: Case series. Jt Dis Relat Surg 2015;26:100-9.
11. Kwon O, Kelly JI. Delayed presentation of osteochondroma on the ventral surface of the scapula. Int J Shoulder Surg 2012;6:61.
12. Jindal M. Delayed presentation of osteochondroma at superior angle of scapula a case report. J Orthop Case Rep 2016;6:32-4.
13. Perez D, Cano JR, Caballero J, Lopez L. Minimally-invasive resection of a scapular osteochondroma. Interact Cardiovasc Thorac Surg 2011;13:468-70.
14. Chillemi C, Franceschini V, Ippolito G, Pasquali R, Diotallevi R, Petrozza V, et al. Osteochondroma as a cause of scapular winging in an adolescent: A case report and review of the literature. J Med Case Rep 2013;7:220.
15. Dharmadhikari RP. Painful snapping and pseudo-winging scapula due to a large scapular osteochondroma. J Orthop Case Rep 2012;2:10-3.
16. Tuncer K, Izgi E, Cankaya B, Ogul H, Kantarci M. Huge bursitis and bursal synovial osteochondromatosis associated with scapular osteochondroma mimicking a giant calcific mass of the chest wall: A case report. Am J Phys Med Rehabil 2018;1-3.
17. Tittal P, Pawar I, Kapoor SK. Pseudo-winging of scapula due to benign lesions of ventral surface of scapula two unusual causes. J Clin Orthop Trauma 2015;6:30-5.
 |
 |
 |
| Dr. S P Barnawal | Dr. B S Gandhi | Dr. A Rathod |
| How to Cite This Article: Barnawal SP, Gandhi BS, Rathod A. Pseudo-winging of Scapula due to Ventral Scapular Osteochondroma: A Case Report and Literature Review. Journal of Orthopaedic Case Reports 2020 August;10(5): 69-72 |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com




