 [box type=”bio”] Learning Point of the Article: [/box]
[box type=”bio”] Learning Point of the Article: [/box]
Mechanical complications associated with implants should be always kept in mind while planning Minimal invasive surgery in spine.
Case Report | Volume 10 | Issue 7 | JOCR October 2020 | Page 34-38 | Bhaskar Sarkar, Nagaraj Manju Moger, Lakshmana Das, J Pragadeeshwaran, M H Chethan, Siddarth Dubey. DOI: 10.13107/jocr.2020.v10.i07.1908
Authors: Bhaskar Sarkar[1], Nagaraj Manju Moger[1], Lakshmana Das[1], J Pragadeeshwaran[1], M H Chethan[1], Siddarth Dubey[1]
[1]Department of Trauma Surgery, All India Institute of Medical Sciences, Rishikesh, Uttarkhand. India.
Address of Correspondence:
Dr. J Pragadeeshwaran,
Department of Orthopaedics, All India Institute of Medical Sciences, Rishikesh, Uttarkhand. India.
E-mail: akjpraga@gmail.com
Abstract
Introduction: Traumatic spine injury is one of the leading causes of morbidity and mortality in trauma patients. Open surgical procedure is associated with increased blood loss, surgical trauma, and increased recovery period. The goal of minimally invasive surgery (MIS) is to minimize iatrogenic trauma caused by open surgery.
Case Report: A 39-year-old female patient presented to us with complaints of severe pain in back following a fall from ten feet height 1-day back. She was diagnosed with L1 burst fracture and was managed by indirect fracture reduction and posterior instrumented stabilization from D12 to L2 by MIS. She presented to us with complaints of pain over back after 3 months of index surgery. Neurology was intact, and ESR and quantitative CRPH were normal. X-ray showed downward and outward displacement of left connecting rod with pedicle screws in situ.
Conclusion: Minimal invasive surgery in spine is associated with steep-learning curve and technical challenges. Mechanical complications associated with implants should be always kept in mind while planning the surgery.
Keywords: Minimal invasive surgery, spine trauma, burst fracture, rod migration, implant complications.
Introduction
Traumatic spine injury (TSI) is one of the leading causes of morbidity and mortality in trauma patients. Global incidence for TSI was 10.5 cases per 100,000 persons (95% CI 8.6–12.84 cases/100,000) that resulted in an estimated 768,473–790,695 cases of TSI worldwide each year as reported by Kumar et al. [1]. Spinal trauma is traditionally managed by decompression and fixation by instrumentation. Open surgical procedure is usually associated with increased blood loss, surgical trauma, and increased recovery period [2]. Significant devascularization and denervation of spinal musculature cause chronic pain after open surgery. The goal of minimally invasive surgery (MIS) is to minimize iatrogenic trauma caused by open surgery. MIS causes decreased denervation and muscle atrophy [3]. Wiltse et al. reported muscle-splitting approach in 1968, with same exposure to perform far-lateral discectomy, insertion of pedicle screws, and ipsi-contralateral decompression in lumbar spine, which formed the basic philosophy of minimal invasive surgery in spine [4]. MIS for spinal trauma was initially reported as endoscopic guided anterior approach in 2005 by Beisse et al. [5]. Assaker et al. presented the use of minimal access spinal techniques for the management of thoracolumbar trauma at Eurospine, Barcelona, Spain, 2005. He has described posterior approach as a stand-alone technique or in combination with an anterior endoscopic approach [6]. First report of a percutaneous transforaminal endoscopic approach combined with percutaneous pedicle screw fixation for the correction of altered sagittal plane alignment in thoracolumbar burst fractures was published in 2014 by Wang et al. [7]. Due to decreased morbidity and postoperative hospital stay compared to open surgeries, which involve extensive sub-periosteal stripping and prolonged retraction of soft-tissues resulting in significant ischemic necrosis of the paraspinal muscles and chronic back pain [8], MIS is gaining popularity over past two decades. Nonetheless, application of MIS principles in spine trauma still remains to be explored and, as per current evidence, has been reported to have a number of hardware-related complications [9]. We are reporting an unusual complication of migration of connecting rod that has been published only once in literature related to spine trauma [10], and in that process, we intend to present a narrative review of literature on failure of implants-related complications in MIS for thoracolumbar spinal injuries.
Case Presentation
A 39-year-old female patient presented to us with complaints of severe pain in back following a fall from ten feet height 1-day back. No history of back pain before trauma. Clinical examination did not reveal any neurologic deficit. Radiologic examination showed burst fracture of L1 (AO type A4) with 15 degrees of segmental kyphosis and thirty percent canal compromise (Fig. 1). She was managed with indirect fracture reduction and posterior instrumented stabilization from D12 to L2 by MIS (Fig. 2). Her further hospital stay was uneventful. She was mobilized full weight bearing with customized thoracic lumbar sacral orthotic (TLSO) brace on post-operative day 1 and was discharged on day 2. Her surgical site staples were removed on post-operative day 14 and there were no wound related complications. She presented to us with complaints of pain over back after 3 months of index surgery. On examination mild tenderness was present over surgical site without any sign of infection or inflammation. Neurology was intact, and ESR and quantitative CRPH were normal. X-ray showed downward and outward displacement of left connecting rod with pedicle screws in situ (Fig. 3). Patient was planned for removal of implant.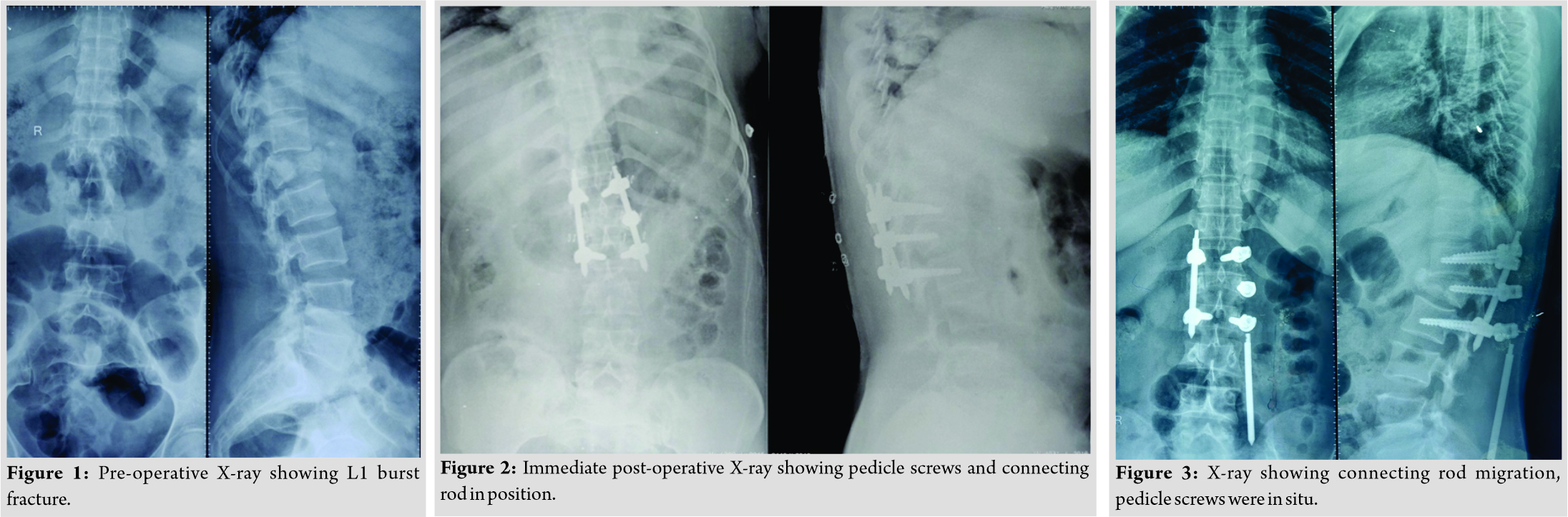
Intraoperatively, pedicle screws were found to be loose, but the cap was found to be tight. No collection or bony changes was found intraoperatively. The displaced rod was traced and removed through a subcutaneous tunnel, without extending the incision, along-with ipsilateral pedicle screws and contralateral connecting rod and pedicle screws. There were no radiologic signs of instability intraoperatively after implant removal. Postoperatively patient started on full weight bearing mobilization with customized TLSO brace and was not having any neurological deficit. Three months after the second surgery, patient is pain-free with Oswestry Disability Index of 30 %.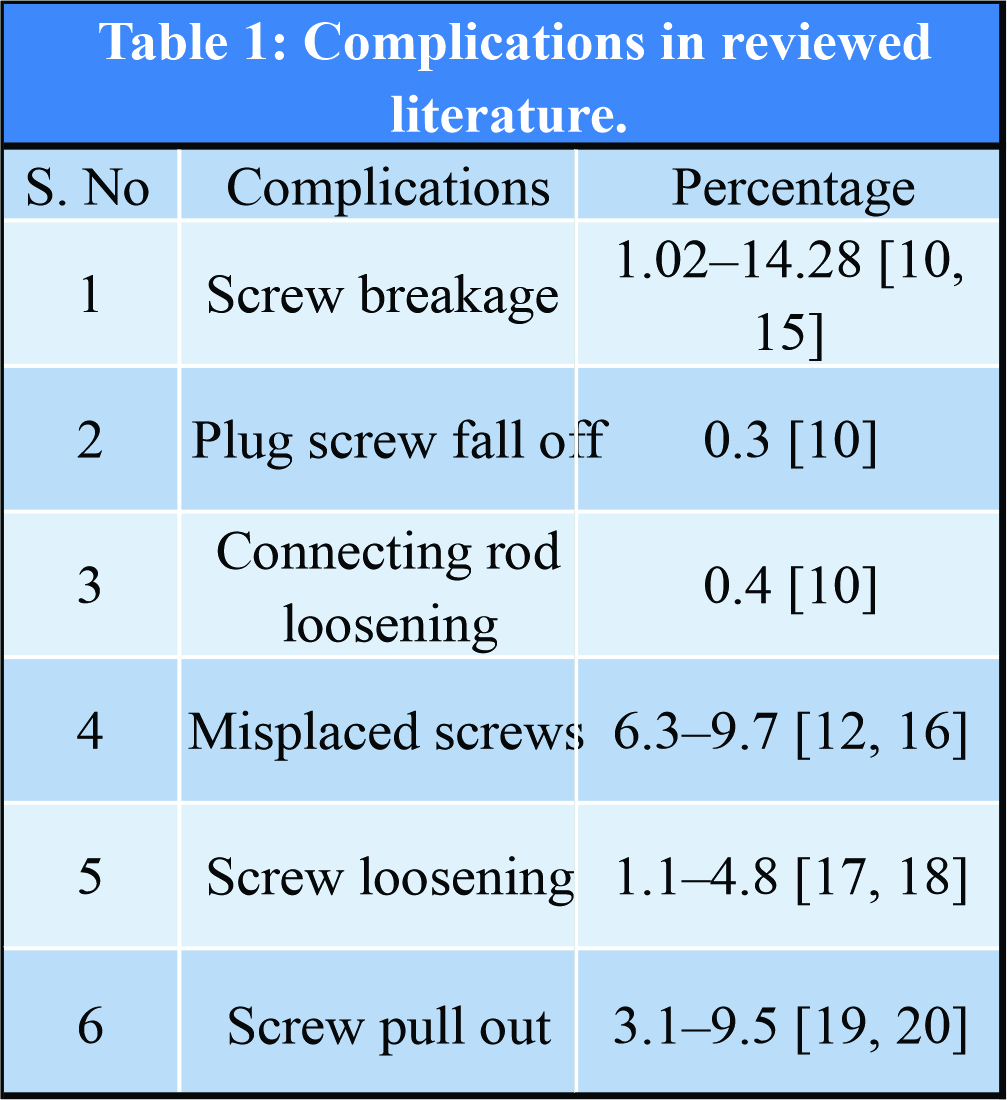
Discussion
Due to limited work-space available in MISS, there is obvious difficulty in locating anatomical landmarks that can result in injury to facet capsule, nerve root, dura, and cord. Such a complication may necessitate open or revision procedures. Although less morbid, minimal invasive surgery is reported to be associated with certain hardware related complications [10].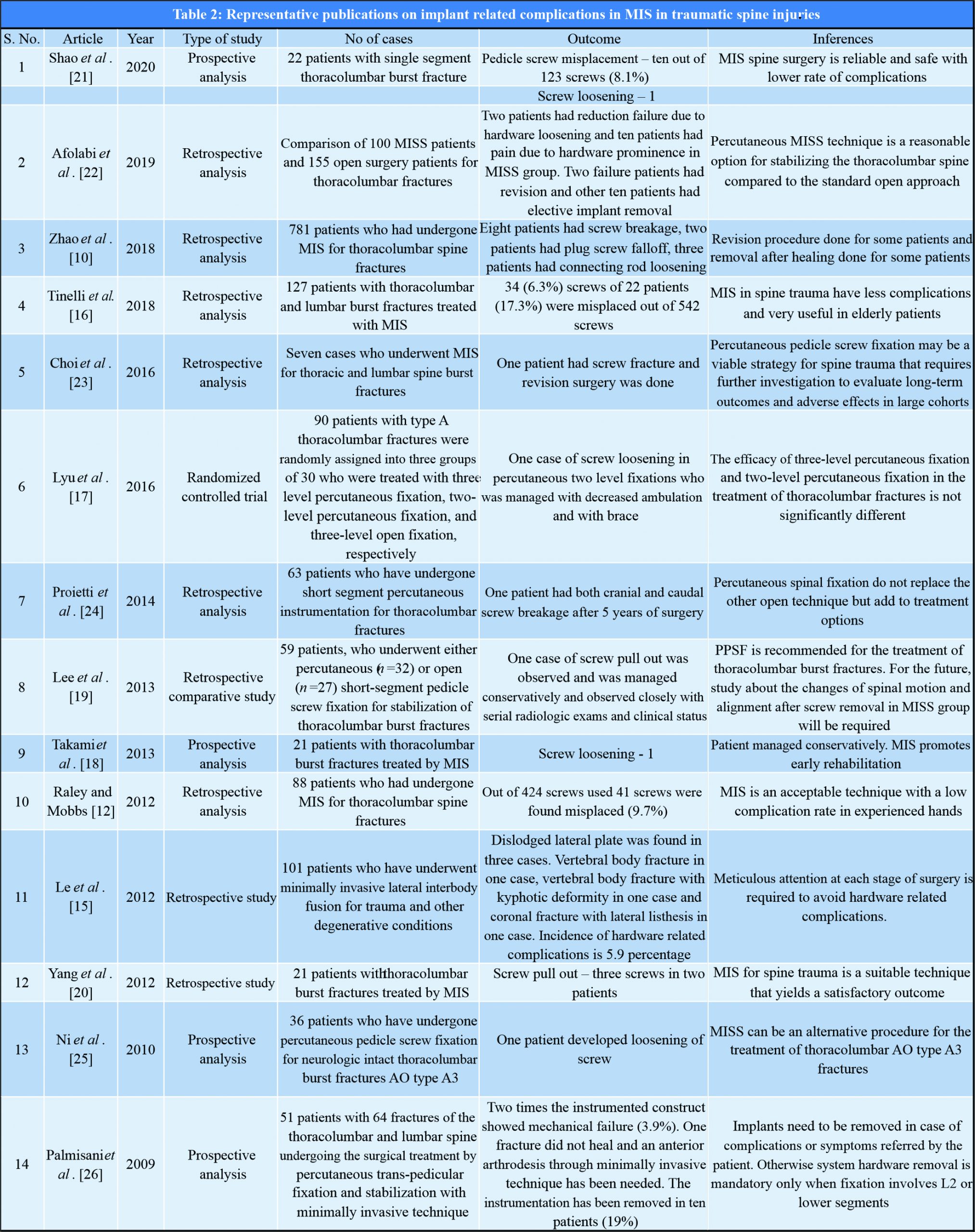
We can divide these broadly into two categories: Organ injuries from hardware and failure of implant. The list includes, though not exclusive of, intraoperative guidewire breakage, abdominal aorta injury, dura mater injury, pedicle screw misplacement, screw breakage, plug screw falling off, connecting rod loosening, and poor reduction [10]. Complication rates for MIS and open surgeries did not differ significantly [11]. A number of recent studies have compared outcomes of open versus MIS and complication rates in both modalities. In a study of 424 percutaneous placed pedicle screws done by Raley and Mobbs, post-operative CT scans demonstrated 41 misplaced screws (9.7%). Lateral cortical breaches were more common (n = 30) than medial breaches (n = 11), and neurological injury as a result of these breaches occurred with two screws (0.5%) [12]. Kramer et al. reported hardware failure, in the form of loss of correction or progressive increase in kyphosis, in 4 of 11 thoracolumbar fractures treated with short-segment fixation performed through a standard open approach with posterolateral fusion within a 2-year follow-up [13]. Biomechanical investigation comparing construct bending stiffness, torsional stiffness, and cycles to failure were done between patients who have undergone MIS versus universal spine stabilization system (USS) by Kubosch et al. [14] shows that construct in MIS is showing significant loss of correction compared to USS. Le et al. did a retrospective study on 101 patients who have underwent minimally invasive lateral interbody fusion for trauma and other degenerative conditions and found that hardware related complications were 5.9% [15]. In our patient, mechanical failure seems to be the reason for loosening of implants. Even though bony union was achieved, construct got weakened on cyclical load from activities of daily living over. The unique features of this case is that the dislodged connecting rod is asymptomatic and without neurological impairment. Even though the construct became weak, bony union was achieved. Patient did not need any revision procedure for stabilization. We removed the implants and postoperatively patient had no neurological deficit and was mobilized full weight bearing with brace. Implant-related complications can be avoided with proper surgical technique and selecting appropriate implants. Timely identification of complications and revision surgeries helps in improving outcome. Percentage of various complications in the studies, we analyzed are compiles in [Table 1]. A compilation of most relevant latest studies on MIS in spinal trauma and the complications in those studies is shown in [Table 2].
Conclusion
Minimal invasive surgery in spine is associated with long learning curve and technical challenges. Mechanical complications associated with implants should be always kept in mind while planning the surgery. Careful selection of patients and implants with proper technique of MIS in spine will be advantageous than open surgeries.
Clinical Message
Migration of connecting rod is an extremely rare and unusual complication in MIS spine surgery that has been published only once in literature related to spine trauma. We are adding another such case to the literature.
References
1. Kumar R, Lim J, Mekary RA, Rattani A, Dewan MC, Sharif SY, et al. Traumatic spinal injury: Global epidemiology and worldwide volume. World Neurosurg 2018;113:e345-63.
2. Seng C, Siddiqui MA, Wong KP, Zhang K, Yeo W, Tan SB, et al. Five-year outcomes of minimally invasive versus open transforaminal lumbar interbody fusion: A matched-pair comparison study. Spine (Phila Pa 1976) 2013;38:2049-55.
3. Hung C, Wu M, Hong R, Weng M, Yu G. Comparison of multifidus muscle atrophy after posterior lumbar interbody fusion with conventional and cortical bone trajectory. Clin Neurol Neurosurg 2020;145:41-5.
4. WILTSE LL, BATEMAN JG, HUTCHINSON RH, NELSON WE. The Paraspinal Sacrospinalis-Splitting Approach to the Lumbar Spine. JBJS. 1968;50(5).
5. Beisse R, Mückley T, Schmidt M, Hauschild M, Bühren V. Surgical technique and results of endoscopic anterior spinal canal decompression. J Neurosurg Spine 2005;2:128-36.
6. Assaker R. Minimal access spinal technologies : State-of-the-art, indications, and techniques. Joint Bone Spine 2004;71:459-69.
7. Wang Y, Ning C, Yao L, Huang X, Zhao C, Chen B, et al. Transforaminal endoscopy in lumbar burst fracture. Medicine (Baltimore) 2017;96:e8640.
8. Fourney DR, Dettori JR, Norvell DC, Dekutoski MB. Does minimal access tubular assisted spine surgery increase or decrease complications in spinal decompression or fusion? Spine (Phila Pa 1976) 2010;35:S57-65.
9. Januszewski J, Vivas AC, Uribe JS. Limitations and complications of minimally invasive spinal surgery in adult deformity. Ann Transl Med 2018;6:109.
10. Zhao Q, Zhang H, Hao D, Guo H, Wang B, He B. Complications of percutaneous pedicle screw fixation in treating thoracolumbar and lumbar fracture. Medicine (Baltimore) 2018;97:e11560.
11. Wu X, Zhang B, Zhang C, Wu X, Zhang Q. Efficacy and safety of minimal pedicle screw fixation for thoracolumbar fractures : A meta-analysis. Eur Rev Med Pharmacol Sci 2018;22:45-52.
12. Raley DA, Mobbs RJ. Retrospective computed tomography scan analysis of percutaneously inserted pedicle screws for posterior transpedicular stabilization of the thoracic and lumbar spine: Accuracy and complication rates. Spine (Phila Pa 1976) 2012;37:1092-100.
13. Kramer DL, Rodgers WB, Mansfield FL. Transpedicular instrumentation and short-segment fusion of thoracolumbar fractures: A prospective study using a single instrumentation system. J Orthop Trauma 1995;9:499-506.
14. Kubosch D, Kubosch EJ, Gueorguiev B, Zderic I, Windolf M, Izadpanah K, et al. Biomechanical investigation of a minimally invasive posterior spine stabilization system in comparison to the universal spinal system (USS). BMC Musculoskelet Disord 2016;17:134.
15. Le TV, Smith DA, Greenberg MS, Dakwar E, Baaj AA, Uribe JS. Complications of lateral plating in the minimally invasive lateral transpsoas approach. J Neurosurg Spine 2012;16:302-7.
16. Tinelli M, Töpfer F, Kreinest M, Matschke S, Grützner PA, Suda AJ. Minimally invasive reduction and percutaneous posterior fixation of one-level traumatic thoraco-lumbar and lumbar spine fractures. Eur J Orthop Surg Traumatol 2018;28:1581-7.
17. Lyu J, Chen K, Tang Z, Chen Y, Li M, Zhang Q. A comparison of three different surgical procedures in the treatment of Type A thoracolumbar fractures: A randomized controlled trial. Int Orthop 2016;40:1233-8.
18. Takami M, Yamada H, Nohda K, Yoshida M. A minimally invasive surgery combining temporary percutaneous pedicle screw fixation without fusion and vertebroplasty with transpedicular intracorporeal hydroxyapatite blocks grafting for fresh thoracolumbar burst fractures: Prospective study. Eur J Orthop Surg Traumatol 2014;24:S159-65.
19. Lee J, Jang J, Kim T. Percutaneous short-segment pedicle screw placement without fusion in the treatment of thoracolumbar burst fractures: Is it effective ?: Comparative study with open short-segment pedicle screw fixation with posterolateral fusion. Acta Neurochir (Wien) 2013;155:2305-12.
20. Yang WE, Ng ZX, Koh KM, Low SW, Lwin S, Choy KS, et al. Percutaneous pedicle screw fixation for thoracolumbar burst fracture: A Singapore experience. Singapore Med J 2012;53:577-81.
21. Shao RX, Zhou H, Peng L, Pan H, Yue J, Hu QF. Clinical efficacy and outcome of intelligently inflatable reduction in conjunction with percutaneous pedicle screw fixation for treating thoracolumbar burst fractures. J Int Med Res 2020;48:300060520903658.
22. Afolabi A, Weir TB, Usmani MF, Camacho JE, Bruckner JJ, Gopinath R, et al. Comparison of percutaneous minimally invasive versus open posterior spine surgery for fixation of thoracolumbar fractures: A retrospective matched cohort analysis. J Orthop 2020;18:185-90.
23. Choi PA, Sekula RF. Minimally invasive spine surgery for unstable thoracolumbar burst fractures: A case series. Surg J (NY) 2016;2:e131-8.
24. Proietti L, Scaramuzzo L, Schirò GR, Sessa S, Aurizio GD, Tamburrelli FC. Posterior percutaneous reduction and fixation of thoraco-lumbar burst fractures. Orthop Traumatol Surg Res 2014;100:455-60.
25. Ni W, Huang Y, Chi Y, Xu H, Lin Y. Percutaneous pedicle screw fixation for neurologic intact thoracolumbar burst fractures. J Spinal Disord Tech 2010;23:530-7.
26. Palmisani M, Gasbarrini A, Brodano GB, De Iure F, Cappuccio M, Boriani L, et al. Minimally invasive percutaneous fixation in the treatment of thoracic and lumbar spine fractures. Eur Spine J 2009;18 Suppl 1:71-4.
 |
 |
 |
 |
 |
 |
| Dr. Bhaskar Sarkar | Dr. Nagaraj Manju Moger | Dr. Lakshmana Das | Dr. J Pragadeeshwaran | Dr. M H Chethan | Dr. Siddarth Dubey |
| How to Cite This Article: Sarkar B, Moger NM, Das L, Pragadeeshwaran J, Chethan MH, Dubey S. Migration of Rod: A Case Report of Rare Complication of Minimal Invasive Surgery in Spinal Trauma with Narrative Review of Literature.. Journal of Orthopaedic Case Reports 2020 October;10(7): 34-38. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com








