 [box type=”bio”] Learning Point of the Article: [/box]
[box type=”bio”] Learning Point of the Article: [/box]
Galeazzi Fracture Dislocations present a surgical emergency and a comprehensive evaluation in the emergency room is essential to avoid missing such injury, in chronic cases every attempt should be made to avoid salvage procedures.
Case Report | Volume 10 | Issue 8 | JOCR November 2020 | Page 37-40 | Turki Abdullah S. Alajmi, Mohammad Suhail Altuwaijri, Hossam Hamad Alnaqa. DOI: 10.13107/jocr.2020.v10.i08.1850
Authors: Turki Abdullah S. Alajmi[1], Mohammad Suhail Altuwaijri[1], Hossam Hamad Alnaqa[1]
[1]Department of Orthopaedics, Prince Mohammed bin Abdulaziz Hospital, Riyadh, Saudi Arabia.
Address of Correspondence:
Dr. Turki Abdullah S. Alajmi,
Department of Orthopaedics, Prince Mohammed bin Abdulaziz Hospital – Riyadh, KSA.
E-mail: turki–aj@hotmail.com
Abstract
Introduction: Galeazzi fracture-dislocation is a unique entity of forearm fractures since they involve a fracture of the radius shaft, along with the dislocation of the distal radioulnar joint, the gold standard of treatment for adults is open reduction and internal fixation with or without repair or pinning of the DRUJ.
Case Report: We present a case of a 27-year-old male with a neglected Galeazzi fracture for over 2 months, the patient was treated with open reduction and internal fixation without the need of a salvage procedure and achieved excellent outcomes.
Conclusion: Galeazzi fractures are not uncommon, and any forearm fracture requires complete radiographic and clinical assessment to avoid dreadful complications of delayed management.
Keywords: Chronic, Distal radioulnar joint, Fracture-dislocation, Galeazzi.
Introduction
Galeazzi fracture represents a distinct spectrum of forearm injuries that represent approximately 7% of adult and 3% of pediatric forearm fractures, they are a unique injury which involves a fracture of the radial diaphysis, along with disruption or dislocation of the distal radioulnar joint (DRUJ) [1]. They were first described in 1877 by a British surgeon and then named after Galeazzi who reported a series of cases describing the incidence, mechanism, and treatment of these injuries [2]. Galeazzi fractures are inherently unstable due to the disruption of the DRUJ and possible disruption of the interosseous membrane (IOM), the triangular fibrocartilage complex (TFCC) is the main stabilizer of the DRUJ and the dorsal and volar radioulnar ligaments are the most important ligaments within the TFCC [3]. The IOM also has a complex structure of bands and cords that prevent translation of the radius and ulna and also transmit axial and rotational forces, the central band is the main restraint and stabilizer within the IOM [3]. Several classification systems have been proposed for Galeazzi fracture-dislocation, the first was described by Walsh, in which the fracture was classified based on its angulation, the position of the forearm (supination of pronation) on axial loading of the fractures will contribute to its apex (apex volar or apex palmar) [4]. On the other hand, two classification systems classify the fracture based on its distance from the DRUJ [5, 6], the most commonly used is the one by Retting [5], in which the fracture is either more than 7.5 cm away from the DRUJ or less, the main rationale behind this classification is that fractures < 7.5 cm are more prone to DRUJ instability according to the results of this study. Historically Galeazzi fractures is adult were treated with open reduction and internal fixation of the radius fracture with or without DRUJ repair and pinning, the is largely due to the highly unsatisfactory outcomes following closed treatment and chronic disability [1]. In pediatrics, however, Galeazzi fracture can be amenable to closed treatment with satisfactory outcomes due to several reasons including thick periosteum, stronger ligamentous restraints, and higher bone modeling capacity [7]. Galeazzi fracture-dislocations are usually managed acutely due to the apparent deformity, pain, and disability suffered by the patient, we have searched the literature and only found one case reporting a chronic Galeazzi fracture-dislocation [8], and therefore, we present our experience with this rare injury.
Case Report
History
A 27-year-old man of Eastern Asian descent presented to our outpatient clinic with a complaint of the right forearm pain and deformity for over 2 months. The pain started 72 days back when the patient sustained a road traffic accident and fell from his motorbike on an outstretched hand, since then, he noticed the deformity in his forearm, and he first thought it was a simple contusion or bruise. The following days the swelling subsided, but the deformity did not resolve completely and he was not able to move his forearm as he could previously, and he did not seek medical attention due to the fact that he was afraid to lose his job. The patient came to us based on the advice of some relatives that he was visiting. Examination: On general examination, he was a well-built gentleman that was not in any pain or discomfort. Local examination of the right forearm showed an obvious deformity with minimal tenderness to palpation. The range of motion examination of the wrist was painful and showed a 30 flexion-extension arc and 60 of pronosupination. The right elbow, metacarpophalangeal, proximal, and distal interphalangeal joints showed a full painless range of motion. The distal neurological examination of the right upper extremity and distal pulses was intact and was compared to the contralateral limb. X-rays are shown in (Fig. 1, 2) which show a distal third radial shaft fracture, ulnar styloid fracture, and a disrupted DRUJ.
Surgical Technique
The surgery was under general anesthesia, the patient was placed supine and the right arm on a radiolucent arm table with a tourniquet, and then, he was draped and prepped using the sterile surgical technique. The tourniquet was inflated, and an anterior approach to the forearm (Henry) [9] was utilized. The intermuscular interval between the flexor carpi radialis and brachioradialis was used, the pronator teres were partially elevated for adequate surgical exposure, and the radial artery and superficial radial nerve were protected throughout the procedure. On exposure of the fracture, the callus was well-formed, so an osteotomy was performed, the fracture was reduced. A 3.5 mm dynamic compression plate with four bicortical screws above and three screws below was utilized. Bone allograft was also used to aid in healing. After anatomic reduction and restoration of the radial bow, the DRUJ was reduced spontaneously, it was tested intraoperatively by ballottement and ulnar pull and was found to be stable, so the decision was made not to extend the incision to the wrist nor to pin it after it was reduced and obviating the need to fix the ulnar styloid fracture. Multilayer closure was done, and then, the arm was splinted in supination (Fig. 3, 4).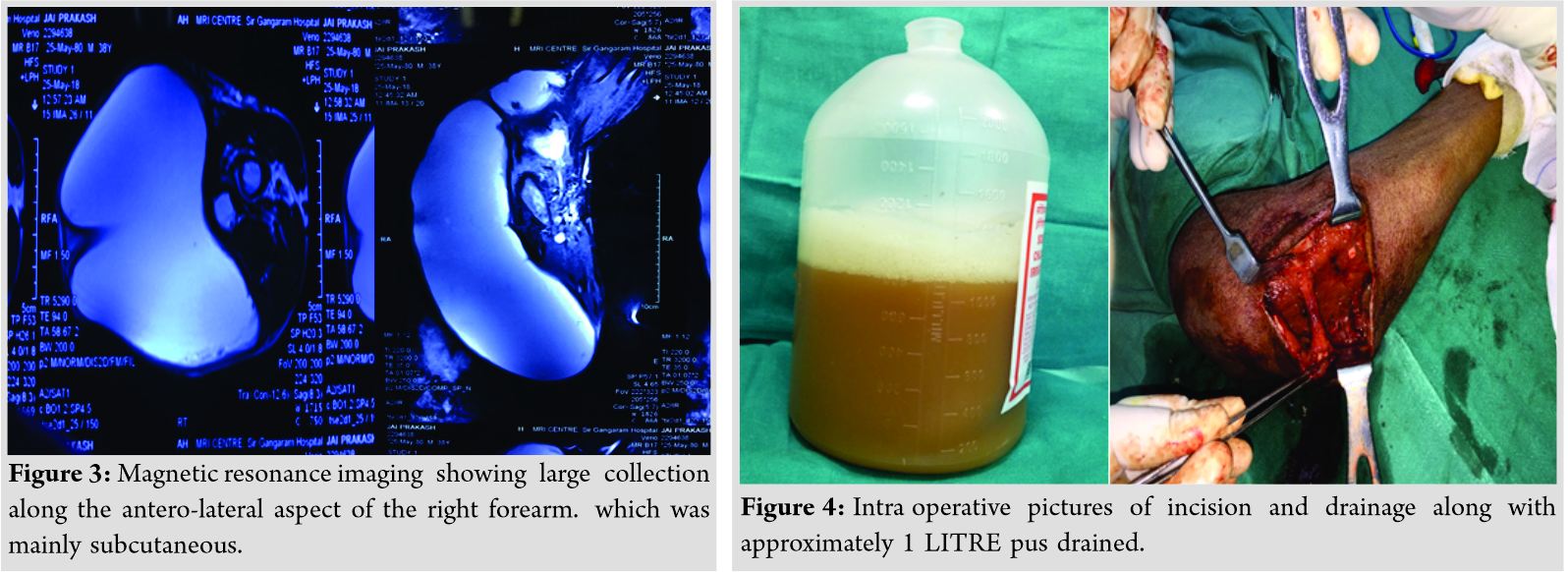
Follow-up and outcomes
At 2 weeks postoperatively, the clips were removed and the splint was discontinued, the patient was then referred to physical therapy for postoperative rehab in an attempt to restore his functional range of motion. (Fig. 5, 6) show his final follow-up with us 3 weeks postoperatively since he left the country to avoid the travel ban following the coronavirus pandemic. We have remained in contact with our patient and his local orthopedic surgeon, he was able to achieve radiographic union at 5 months, and his range of motion was 70o of wrist extension, 80o of wrist flexion, and 150o of pronosupination, as shown in (Fig. 7-10). The patient was discharged from orthopedic care 5 months postoperatively.
Discussion
The successful outcomes of Galeazzi fracture treatment are mainly dependent on several factors which are anatomical reduction of the radius and restoration of the radial bow, reduction of the DRUJ, and restoration of the forearm axis of rotation. Any disproportion of the length between the radius and ulna, which are nearly parallel, will disrupt the complex mechanical relationship between them. These successful outcomes in adults can only be achieved by surgical fixation, as Hughston [10] has shown that closed treatment with closed reduction and immobilization has an unacceptably high failure rate of 92%. The classic approach to the radius in Galeazzi fractures is the volar (Henry) approach since it is technically easier and also has better soft-tissue coverage, although Riju has reported a study of 42 patient, in which they have used the dorsal (Thomson) approach with no difference in outcomes [11].Conventionally, the 3.5 dynamic compression plate has been used to reduce and fix Galeazzi fractures, and currently, there is insufficient evidence to support the locking plate construct with unicortical screws, especially with current evidence suggesting that dynamic plate may result in higher torsional stability [12]. On the other hand, closed treatment consisting of closed reduction and immobilization in above-elbow splint with the forearm in supination for 4–6 weeks has been the gold standard in treating pediatric Galeazzi fractures with successful results [7]. The success of closed treatment in the pediatric population is attributed to the elasticity and the strength of the DRUJ, the thick periosteum, and the higher fracture remodeling capacity [7]. Exceptions to closed treatment for the pediatric age group would be the inability to achieve closed reduction and loss of reduction during further follow-up. In a review of 41 pediatric patients with Galeazzi fractures, the author only reported 2 requiring ORIF with the remainder achieving satisfactory results [4]. Furthermore, irreducible DRUJ dislocations following Galeazzi fractures were not that uncommon; in one systemic review, they have found 17 cases of irreducible dislocations with more than half of them being missed either pre- or intraoperatively [13]. In dorsal dislocations, around 92% of the dislocations were secondary to an extensor tendon entrapment, including the extensor digit minimi, extensor carpi ulnaris, and extensor digitorum communis. However, in volar dislocations, more than 17% were due to entrapment of the ulnar head, and no tendons were identified in the remainder of volar dislocations to be the cause of irreducibility. Open reduction and internal fixation of the associated ulnar styloid fracture in Galeazzi fracture-dislocations remain to be a highly controversial topic; in one study, more than half the patients with instability of the DRUJ after fixation had an associated ulnar styloid fracture [14]. Nevertheless, DRUJ instability is subjective to many factors, including the distance of the radius fracture from the joint line, interposition of tendon and bony fragments, and also the size of the ulnar styloid fracture. In a case report of a patient that sustained an acute bilateral Galeazzi fracture-dislocation with bilateral ulnar styloid fractures, the right DRUJ was found to be unstable after fixing the radius fracture, so an ORIF of the ulnar styloid fracture was done; however, the right DRUJ was stable after fixation and reduction, and the right ulnar styloid fracture was not fixed, and the patient had excellent outcomes postoperatively [15]. On review of the literature, we have only found one case of a chronic Galeazzi fracture-dislocation, the patient had a possible open fracture at the time of injury, and due to the advanced degenerative changes, the patient underwent a distal radioulnar fusion (Sauvé-Kapandji) procedure [8]. Although an arthrodesis of a joint is a very reliable and durable procedure, single patient factors need to be taken into consideration. For example, the age difference between our patient’s, the duration of the injury, and the possibility of an open fracture and contamination all play a very critical role. We also recommend that arthrodesis should be the final decision for limb salvage, and other treatment options should be exhausted before attempting to fuse the DRUJ.
On the other hand, closed treatment consisting of closed reduction and immobilization in above-elbow splint with the forearm in supination for 4–6 weeks has been the gold standard in treating pediatric Galeazzi fractures with successful results [7]. The success of closed treatment in the pediatric population is attributed to the elasticity and the strength of the DRUJ, the thick periosteum, and the higher fracture remodeling capacity [7]. Exceptions to closed treatment for the pediatric age group would be the inability to achieve closed reduction and loss of reduction during further follow-up. In a review of 41 pediatric patients with Galeazzi fractures, the author only reported 2 requiring ORIF with the remainder achieving satisfactory results [4]. Furthermore, irreducible DRUJ dislocations following Galeazzi fractures were not that uncommon; in one systemic review, they have found 17 cases of irreducible dislocations with more than half of them being missed either pre- or intraoperatively [13]. In dorsal dislocations, around 92% of the dislocations were secondary to an extensor tendon entrapment, including the extensor digit minimi, extensor carpi ulnaris, and extensor digitorum communis. However, in volar dislocations, more than 17% were due to entrapment of the ulnar head, and no tendons were identified in the remainder of volar dislocations to be the cause of irreducibility. Open reduction and internal fixation of the associated ulnar styloid fracture in Galeazzi fracture-dislocations remain to be a highly controversial topic; in one study, more than half the patients with instability of the DRUJ after fixation had an associated ulnar styloid fracture [14]. Nevertheless, DRUJ instability is subjective to many factors, including the distance of the radius fracture from the joint line, interposition of tendon and bony fragments, and also the size of the ulnar styloid fracture. In a case report of a patient that sustained an acute bilateral Galeazzi fracture-dislocation with bilateral ulnar styloid fractures, the right DRUJ was found to be unstable after fixing the radius fracture, so an ORIF of the ulnar styloid fracture was done; however, the right DRUJ was stable after fixation and reduction, and the right ulnar styloid fracture was not fixed, and the patient had excellent outcomes postoperatively [15]. On review of the literature, we have only found one case of a chronic Galeazzi fracture-dislocation, the patient had a possible open fracture at the time of injury, and due to the advanced degenerative changes, the patient underwent a distal radioulnar fusion (Sauvé-Kapandji) procedure [8]. Although an arthrodesis of a joint is a very reliable and durable procedure, single patient factors need to be taken into consideration. For example, the age difference between our patient’s, the duration of the injury, and the possibility of an open fracture and contamination all play a very critical role. We also recommend that arthrodesis should be the final decision for limb salvage, and other treatment options should be exhausted before attempting to fuse the DRUJ.
Conclusion
Galeazzi fracture-dislocations are not uncommon, ORIF with anatomic reduction of the DRUJ is paramount to achieve functional outcomes in adults. All Galeazzi fractures should be tested for DRUJ instability pre-, intra-, and postoperatively for optimum functional outcomes, and concomitant ulnar styloid fractures should be fixed if there is residual DRUJ instability. Chronic Galeazzi fractures are extremely rare in the literature, and late diagnosis can lead to arthrodesis, prolonged rehab, and possible suboptimal functional outcomes if not managed properly.
Clinical Message
Galeazzi fracture-dislocations are a unique spectrum of injuries, they require a high index of clinical suspicion in radius fracture, as acute injuries have a wide array of management options, chronic injuries also have a relatively good number of options with supporting evidence. Every attempt to salvage the DRUJ and preserve function should be made in chronic injuries.
References
1. Giannoulis FS, Sotereanos DG. Galeazzi fractures and dislocations. Hand Clin 2007;23:153-63, 5.
2. Sebastin SJ, Chung KC. A historical report on Riccardo Galeazzi and the management of Galeazzi fractures. J Hand Surg Am 2010;35:1870-7.
3. Slutsky DJ. Interosseous membrane and its effect on the distal radioulnar joint. J Wrist Surg 2016;5:171.
4. Walsh HP, McLaren CA, Owen R. Galeazzi fractures in children. J Bone Joint Surg Br 1987;69:730-3.
5. Rettig ME, Raskin KB. Galeazzi fracture-dislocation: A new treatment-oriented classification. J Hand Surg Am 2001;26:228-35.
6. Maculé Beneyto F, Renú JM, Claramunt AF, Soler RR. Treatment of Galeazzi fracture-dislocations. J Trauma 1994;36:352-5.
7. Rodríguez-Merchán EC. Pediatric fractures of the forearm. Clin Orthop Relat Res 2005;432:65-72.
8. Truffin RY, López CR, Pérez MO. Treatment of a chronic Galeazzi fracture-dislocation. A case report. Medisur 2016;14:549-54.
9. Henry AK. Extensile Exposure. 2nd ed. Baltimore, Maryland: Williams & Wilkins; 1970. p. 100.
10. Hughston JC. Fracture of the distal radial shaft; mistakes in management. J Bone Joint Surg Am 1957;39-A:249-64.
11. Riju KP. Surgical management of Galeazzi fractures-a clinical study of 42 patients. Int J Sci Study 2017;5:171-8.
12. Roberts JW, Grindel SI, Rebholz B, Wang M. Biomechanical evaluation of locking plate radial shaft fixation: Unicortical locking fixation versus mixed bicortical and unicortical fixation in a sawbone model. J Hand Surg Am 2007;32:971-5.
13. Yohe NJ, de Tolla J, Kaye MB, Edelstein DM, Choueka J. Irreducible Galeazzi fracture-dislocations. Hand (NY) 2019;14:249-52.
14. Tsismenakis T, Tornetta P 3rd. Galeazzi fractures: Is DRUJ instability predicted by current guidelines? Injury 2016;47:1472-7.
15. Komura S, Nonomura H, Satake T, Yokoi T. Bilateral Galeazzi fracture-dislocations: A case report of early rehabilitation. Strategies Trauma Limb Reconstr 2012;7:99-104.
 |
 |
 |
| Dr. Turki Abdullah S. Alajmi | Dr. Mohammad Suhail Altuwaijri | Dr. Hossam Hamad Alnaqa |
| How to Cite This Article: Alajmi TA, Altuwaijri MS, Alnaqa HH. Chronic Galeazzi Fracture-Dislocation: A Case Report. Journal of Orthopaedic Case Reports 2020 November;10(8): 37-40. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com




