[box type=”bio”] Learning Point of the Article: [/box]
[box type=”bio”] Learning Point of the Article: [/box]
Osteomyelitis caused by Streptococcus anginosus is a rare entity and it demands a thorough clinical history and physical examination including the oral cavity.
Case Report | Volume 10 | Issue 9 | JOCR December 2020 | Page 19-22 | Luís Mata Ribeiro, Sara Carvalho, Diogo Guimarães, Manuel Vilela, Ana S. Guerra. DOI: 10.13107/jocr.2020.v10.i09.1888
Authors: Luís Mata Ribeiro[1], Sara Carvalho[1], Diogo Guimarães[1], Manuel Vilela[1], Ana S. Guerra[1]
[1]Department of Plastic and Reconstructive Surgery, Hospital São José (Centro Hospitalar Lisboa Central), Rua José António Serrano, 1150-199 Lisbon, Portugal.
Address of Correspondence:
Dr. Luís Mata Ribeiro,
Department of Plastic and Reconstructive Surgery, Hospital São José (Centro Hospitalar Lisboa Central), Rua José António Serrano, 1150-199 Lisbon, Portugal.
E-mail: luis1989ribeiro@gmail.com
Abstract
Introduction: Osteomyelitis of the hand is a rare entity and almost always occurs after catastrophic injuries. Streptococcus anginosus is a part of the normal microbial flora of the oral cavity and the gastrointestinal tract. It is frequently associated with purulent infections in several anatomic locations but rarely harms bony structures. The occurrence of osteomyelitis of the hand caused by this microorganism is very unusual.
Case Report: We report the clinical case of a 58-year-old Caucasian male, ex-smoker, with a medical history of a chronic hepatitis C virus infection, liver cirrhosis, and diabetes mellitus that developed extensive osteomyelitis of the middle and distal phalanx of his right ring finger caused by S. anginosus and needed amputation for infection control. He had suffered a cut with a steel grinder on that finger 2 weeks before coming to the emergency department. He was also had been submitted to a dental procedure (tooth extraction) the exact day before the trauma. We believe that the most likely origin of the osteomyelitis was a transient bacteremia caused by the dental procedure that led to hematogenous seeding of several oral commensal microbes, including S. anginosus, that ended up infecting an area with low immune capacity due to the trauma.
Conclusion: S. anginosus causes purulent infections in multiple locations and affects more often immunocompromised patients, especially those with cirrhosis and diabetes mellitus. Even though it is not often associated with osteomyelitis, we should have a high level of suspicion if the patient has an intraoral disease or a history of dental or gastrointestinal procedures. The infection is severe, often leading to the need for radical debridements.
Keywords: Phalangeal osteomyelitis, Streptococcus anginosus, hematogenous, suppuration.
Introduction
Infections of the hand are common and can have devastating consequences. Nonetheless, osteomyelitis is rarely seen in the carpus or the tubular bones of the hand [1]. Most frequently it happens after a traumatic or contaminating accident leading to direct bone injury or from contiguous spread from nearby soft tissue. Less common is the hematogenous dissemination. Staphylococcus aureus and Gram-negative bacteria are the most frequent pathogens in adults [2]. Streptococcus anginosus is known for its aggressive behavior and is frequently associated with invasive pyogenic infections, notably on the liver and brain [3]. Despite this, it is very rarely associated with osteomyelitis [1, 4, 5, 6, 7, 8]. We present a case of phalangeal osteomyelitis caused by S. anginosus in an adult male.
Case Report
A 58-year-old man presented to the emergency department with a swollen and painful ring finger of the right hand and a purulent discharge through a small wound on the dorsal aspect of the distal phalanx. Twelve days before the admission, the patient admitted having sustained a small cut with a steel grinder in the location described above. He did daily dressings at home for 5 days, but as the pain increased and the finger started to swell, he went to the emergency department of another hospital where he was prescribed an antibiotic (amoxicillin/clavulanic acid) and anti-inflammatory drugs and was sent home. The symptoms did not improve, and after a week, the patient sought additional help. The exact day before the trauma the patient was submitted to a tooth extraction (due to a vertical fracture of the right inferior molar). The procedure was uneventful, without the need for suture or antibiotics. The patient denied fever, rashes, arthralgias, myalgias, and headaches.
His medical history comprised a long-standing hepatitis C virus infection with liver cirrhosis, hepatocellular carcinoma (submitted to embolization 3 years previously), porphyria cutanea tarda, and non-insulin-dependent diabetes mellitus. He was an ex-smoker. On physical examination, he had normal vital signs and a temperature of 36,9°C. There were moderate tenderness and swelling as well as skin erythema throughout the distal phalanx of his right ring finger and a purulent discharge through a dorsal wound. Pain was elicited with flexion of the finger, but the range of motion seemed unaffected. There were no periodontal abscesses or other signs of oral disease. The examination was otherwise regular.
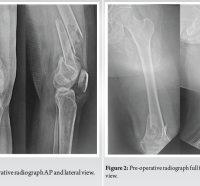
Initial laboratory studies revealed a normal hemoglobin level (15,4 × 10 g/L) and white blood cell count (7,84 × 10^9/L) as well as a normal C-reactive protein level (3,7 mg/L). The X-ray showed a transverse fracture of the base of the distal phalanx with periosteal reaction (Fig. 1). The patient was started on empiric endovenous antibiotic therapy (clindamycin and amoxicillin/clavulanic acid) and was taken to the operating room. A sample of the purulent discharge was collected for microbiological analysis. and The finger was submitted to debridement of soft tissue and unhealthy bone, washing, and osteosynthesis with two Kirschner wires (with a slight shortening of the distal phalanx). After 2 days, the microbiological results came back positive for S. anginosus, and the patient was discharged home the next day medicated with cefuroxime (chosen according to the microbiological sensitivity tests), maintaining strict hand elevation and changing dressings every 2 days. The immediate post-operative phase went uneventfully, but 2 weeks later, the patient noticed a small liquid discharge through the dorsal wound and began having moderate pain in that location (Fig. 2). The X-ray showed extensive osteomyelitis of the distal and middle phalanx (Fig. 3a, b). The patient was reoperated: Amputation at the proximal third of the middle phalanx (preserving the central slip of the extensor apparatus and the flexor digitorum superficialis insertions) and coverage of the stump with a volar flap. Cultural tests were negative this time. The patient maintained the same antibiotic (three additional weeks) and post-operative regimen described above. The healing was uneventful. Twelve months later, the patient was asymptomatic. Soft-tissue coverage is stable with normal scarring and the X-rays show no signs of residual osteomyelitis (Fig. 4).
Discussion
Osteomyelitis is a severe infection that can compromise the vascular network of the bone and lead to intramedullary/subperiosteal abscesses or bony sequestrum [9]. Osteomyelitis in the hand is most frequently caused by direct contamination (open trauma) or by contiguous spread from a soft-tissue infection, like a felon or tenosynovitis [1, 9]. In a minority of patients, it can be caused by hematogenous spread. S. anginosus is a facultative anaerobe and is a member of S. anginosus group (SAG), also known as Streptococcus milleri group. SAG has distinct features from other streptococci in that they can cause pyogenic infections in several locations [5]. S. anginosus is a part of the normal flora of the oropharynx, genitourinary tract, and gastrointestinal tract [10, 11]. It has been found to cause many purulent infections with a propensity for the intra-abdominal area (liver and pelvic abscesses and peritonitis), respiratory tract (pleural empyemas and lung abscesses), and brain/meningeal infections [6, 10, 11]. Despite this aggressive behavior, it is a very unusual cause of osteomyelitis. Among patients with this kind of infection, its’ incidence rate is reported between 3,7 and 9% [5, 6, 7, 12], and most frequently the infection is located in the mandible or in the long tubular bones of the lower limbs. This clinical case demonstrates an example of osteomyelitis in an unusual location (finger phalanx) and has two potential mechanisms involved. First, the patient suffered a trauma to his right ring finger with a steel blade which may have contaminated the area and led to the soft tissue and bone infection. Nevertheless, the microorganisms usually responsible for this kind of the infection in this particular setting are S. aureus, coagulase-negative staphylococci, and Gram-negative bacteria (Pseudomonas aeruginosa, Klebsiella pneumoniae, or Enterobacter). Second, the patient was submitted to a tooth extraction <24 h before the hand trauma. It is well established in the literature the presence of bacteria in the bloodstream following dental extractions. It was thought to be a transitory period lasting only a few seconds or minutes, but several recent studies question that idea [10, 13]. Livingston et al. reported a liver abscess following a routine dental cleaning in an immunocompetent adult male [10]. It is possible that in this case, a transient bacteremia occurred after the dental procedure and the seeding mechanism led the bacteria to an area of injury, a “locus minoris resistentiae” [9]. Other additional circumstances that support the hematogenous spread of the infection are the patients’ comorbidities. Hematogenous infections are predominantly encountered in immunocompromised and diabetics [9], and S. anginosus infections are mostly found in male adults with a history of cirrhosis, neoplasia, diabetes mellitus, and smoking [7, 14, 15]. The treatment of osteomyelitis consists of antibiotics, adequate surgical debridement, and bone fixation [2, 9]. Griffin et al., who published the biggest case series of osteomyelitis caused by S. anginosus, reported a prolonged need for antibiotic treatment and the need for multiple surgeries (≥3 on average) [6]. Chatelain et al. corroborated these findings and also noticed a high number of radical reconstructive procedures (2/3) [4]. Regarding antibiotic choice, S. anginosus is almost always susceptible to penicillin and in most published literature beta-lactam antibiotics are the treatment of choice for SAG infections [7, 15]. The adequate duration of antibiotic treatment has not been established yet. Most authors recommend between 4 and 10 weeks [2, 3, 6, 12].
Conclusion
S. anginosus osteomyelitis has a propensity to occur in middle-aged men who are smokers and immunocompromised. This bacteria causes a locally aggressive infection and is associated with multiple surgeries and prolonged antibiotic therapy. This case highlights the need to be suspicious about a possible oral source of infection since even routine dental cleaning can put the patients at risk for developing infectious complications. Beta-lactam antibiotics and extensive surgical debridement are the mainstays of treatment.
Clinical Message
Osteomyelitis caused by S. anginosus is a rare entity and it demands a thorough clinical history and physical examination including the oral cavity. Antibiotics and prompt surgical debridement are crucial for a good outcome.
References
1. Reilly KE, Linz JC, Stern PJ, Giza E, Wyrick JD. Osteomyelitis of the tubular bones of the hand. J Hand Surg Am 1997;22:644-9.
2. Janssen EH, De Bree LC, Kant KM, Van Wijngaarden P. Spontaneous fracture of the femur due to osteomyelitis caused by the Streptococcus anginosus group. Neth J Med 2017;75:121-4.
3. Giuliano S, Rubini G, Conte A, Goldoni P, Falcone M, Vena A, et al. Streptococcus anginosus group disseminated infection: Case report and review of literature. Infez Med 2012;20:145-54.
4. Chatelain S, Lombardi T, Scolozzi P. Streptococcus anginosus dental implant-related osteomyelitis of the jaws: An insidious and calamitous entity. J Oral Maxillofac Surg 2018;76:1187-93.
5. Suzuki H, Hase R, Otsuka Y, Hosokawa N. Bloodstream infections caused by Streptococcus anginosus group bacteria: A retrospective analysis of 78 cases at a Japanese Tertiary Hospital. J Infect Chemother 2016;22:456-60.
6. Griffin AT, Timbrook T, Harting J, Christensen D. Streptococcus anginosus group and osteomyelitis: A single centre clinical experience. Postgrad Med J 2013;89:262-5.
7. Fazili T, Riddell S, Kiska D, Endy T, Giurgea L, Sharngoe C, et al. Streptococcus anginosus group bacterial infections. Am J Med Sci 2017;354:257-61.
8. Kobo O, Nikola S, Geffen Y, Paul M. The pyogenic potential of the different Streptococcus anginosus group bacterial species: Retrospective cohort study. Epidemiol Infect 2017;145:3065-9.
9. Germann G, Petracic A, Wittemann M, Raff T. Hematogenous osteomyelitis of the hand skeleton in adults after dental maxillary infections. Ann Plast Surg 1996;37:106-10.
10. Livingston LV, Perez-Colon E. Streptococcus intermedius bacteremia and liver abscess following a routine dental cleaning. Case Rep Infect Dis 2014;2014:954046.
11. Neumayr A, Kubitz R, Bode JG, Bilk B, Häussinger D. Multiple liver abscesses with isolation of Streptococcus intermedius related to a pyogenic dental infection in an immuno-competent patient. Eur J Med Res 2010;15:319-22.
12. Krebs NM, Krebs RC, Yaish AM. Femoral osteomyelitis presenting as a pathologic fracture in a 53 year old male: A rare case report. J Orthop Case Rep 2017;7:85-8.
13. Tomás I, Pereira F, Llucián R, Poveda R, Diz P, Bagán JV. Prevalence of bacteraemia following third molar surgery. Oral Dis 2008;14:89-94.
14. Jacobs JA, Pietersen HG, Stobberingh EE, Soeters PB. Bacteremia involving the “Streptococcus milleri” group: Analysis of 19 cases. Clin Infect Dis 1994;19:704-13.
15. Wenzler E, Chandrasekaran V, Salvador P, Anwar M, Pancholi P, McGwire BS. Clinical and microbiological outcomes in patients with Streptococcus anginosus group bacteraemia identified through use of a rapid microarray assay. J Med Microbiol 2015;64:1369-74.
 |
 |
 |
 |
 |
| Dr. Luís Mata Ribeiro | Dr. Sara Carvalho | Dr. Diogo Guimarães | Dr. Manuel Vilela | Dr. Ana S. Guerra |
| How to Cite This Article: Mata Ribeiro L, Carvalho S, Guimarães D, Vilela M, Guerra AS. Streptococcus anginosus and Phalangeal Osteomyelitis: An Unusual Presentation. Journal of Orthopaedic Case Reports 2020 December;10(9): 19-22. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com