[box type=”bio”] Learning Point of the Article: [/box]
[box type=”bio”] Learning Point of the Article: [/box]
Although rare, spinal brucellosis must remain as a differential diagnosis in any patient presenting with low back pain and fevers, and a thorough history of the patient’s complaints is an essential component to properly diagnosing and treating this infection.
Case Report | Volume 11 | Issue 3 | JOCR March 2021 | Page 1-5 | James M Rizkalla, Khalid Alhreish, Ishaq Y Syed. DOI: 10.13107/jocr.2021.v11.i03.2060
Authors: James M Rizkalla[1], Khalid Alhreish[1], Ishaq Y Syed[1]
[1]Department of Orthopaedic Surgery, Baylor University Medical Center, Dallas, Texas, United States.
Address of Correspondence:
Dr. James M Rizkalla,
Department of Orthopaedic Surgery, Baylor University Medical Center, Dallas, Texas, United States.
E-mail: jrizkall@gmail.com
Abstract
Introduction: The most common location of infection of brucellosis is the musculoskeletal system. It is estimated that the spine is involved in 2–54% of brucellosis infections, with the lumbar spine most commonly affected. We report an uncommon case of brucellar spondylodiscitis, in addition to the pathology, common presentation, and management of spinal brucellosis through additional literature review.
Case Report: A 65-year-old Hispanic male presented to an orthopedic spine surgeon with signs and symptoms concerning for metastatic disease to the spine. Investigation revealed that the patient had the rare diagnosis of brucellar spondylodiscitis. This only became apparent after detailed questioning of the patient’s history revealed his employment within a Mexican meat slaughterhouse and a regular consumer of unpasteurized Mexican cheeses.
Conclusion: Although uncommon, brucellosis spondylodiscitis should remain as a differential diagnosis in any patient who presents with back pain and fever. Detailed history taking and thorough physical examination remain vital in the work-up of brucellar spondylodiscitis. Understanding the pathology, radiographic findings, and necessary work-up are essential to properly treat this infection.
Keywords: Spine, Brucella, spinal brucellosis, infection, spondylodiscitis, discitis, abscess.
Introduction
Brucellosis is the most common bacterial zoonosis, with more than 500,000 cases annually worldwide [1], with the most endemic areas consisting of Mediterranean countries and the Middle East [2]. However, frequent misdiagnosis and underreporting lead to inaccuracies in epidemiological reports [3]. Brucellosis is caused by an intra-cellular bacterium of the genus Brucella, which can routinely infect many organ systems, tissues, and lead to systemic changes [2]. Infected farm animals are prominent vectors of brucellosis and are a primary source of transmission to humans [4]. Brucellosis is transmitted through contact with farm animals or drinking unpasteurized dairy products. Osteoarticular involvement is the most frequent complication of chronic brucellosis. However, the diagnosis of Brucella spondylodiscitis is difficult due to a common clinical presentation, which can be obscured by many other conditions or more common infections [5]. Of all the articular manifestations of brucellosis, spinal brucellosis is one of the most frequently involved locations. It is estimated that the spine is involved in 2–54% of Brucella infections, with the lumbar spine most commonly affected [6, 7, 8]. In general, speaking, patients with spinal brucellosis present with back pain. Although rare, patients must be evaluated for neurological deficits, which may signify the development of an epidural abscess and potential permanent injury. A spectrum of spinal brucellosis exists depending on the location of the infection. Brucellosis may infect the vertebral body causing spondylitis, the vertebral disc causing discitis, or both resulting in spondylodiscitis [6]. Brucellar spondylitis, or the infection of the vertebrae secondary to Brucella, is most commonly seen in men older than 40 years of age and has a prevalence rate of 2–60% [6, 8, 9]. The infection may be focal or diffuse. Focal brucellar spondylitis is typically located on the anterior aspect of the endplate at the junction of the vertebral disc and vertebral body [6]. In contrast, diffuse spondylitis describes osteomyelitis of the whole vertebral body [6, 10]. The foundation of diagnosing brucellar spondylitis is a microbiological or histopathological assessment of the tissue, typically through a core-needle bone biopsy. Brucella may travel and infect solely the intervertebral disc, resulting in a brucellar discitis. In addition to back pain, disc herniation and sciatica have been recognized as a potential complication of discitis [6, 11, 12]. Guglielmino et al. described a case of a patient with back pain and spondylolisthesis that was mismanaged due to the delayed, and unsuspected, diagnosis of Brucella discitis [6, 13]. This reiterates that variable clinical features and an overall lack of specific symptoms can frequently result in a delay in diagnosis of spinal brucellosis and potentially worse outcomes. In most severe cases, Brucella will infect both the vertebral body and the intervertebral disc, resulting in a spondylodiscitis. This is frequently recognized as the most severe form of the infection, due to its high rate of neurological sequelae due to abscess formation, despite antibiotic therapy [6]. It is important to image the entirety of the spine, as multi-focal skeletal involvement is seen in 3–14% of patients with spinal brucellosis [2, 6, 14]. The purpose of this case report is to emphasize the importance of a thorough history of the patient when presented with an infectious etiology. Diagnosing spinal brucellosis is a challenging diagnosis that should remain on the differential in all patients that present with back pain and signs of an infection. Spinal brucellosis may present in an unusual fashion. Therefore, a detailed evaluation, understanding of the pathophysiology of the bacteria, and treatment options are of critical importance to properly diagnose and care for a patient with acute spinal brucellosis.
Case Report
A 65-year-old male presented to our department with a history of back pain with a low-grade fever for 3 weeks. His back pain was located in the mid dorsal region, which was purely mechanical in nature (pain increased on movements and coughing) and did not radiate along his ribs. It was not associated with any neurological symptoms such as tingling, numbness, imbalance, bowel/bladder dysfunction, or weakness in his lower extremities. Severity of pain was gradually increasing from 2/10 to 7/10 on VAS scale, despite conservative treatment by his primary care physician. His clinical picture was further complicated by a significant history of 40 pounds of weight loss over the past few months. At baseline, his medical history was significant for hypertension, hypercholesterolemia, and Type II diabetes. On examination, the patient had localized tenderness around T8-9 level without any deformity or swelling. Patent’s neurological examination did not reveal any abnormalities.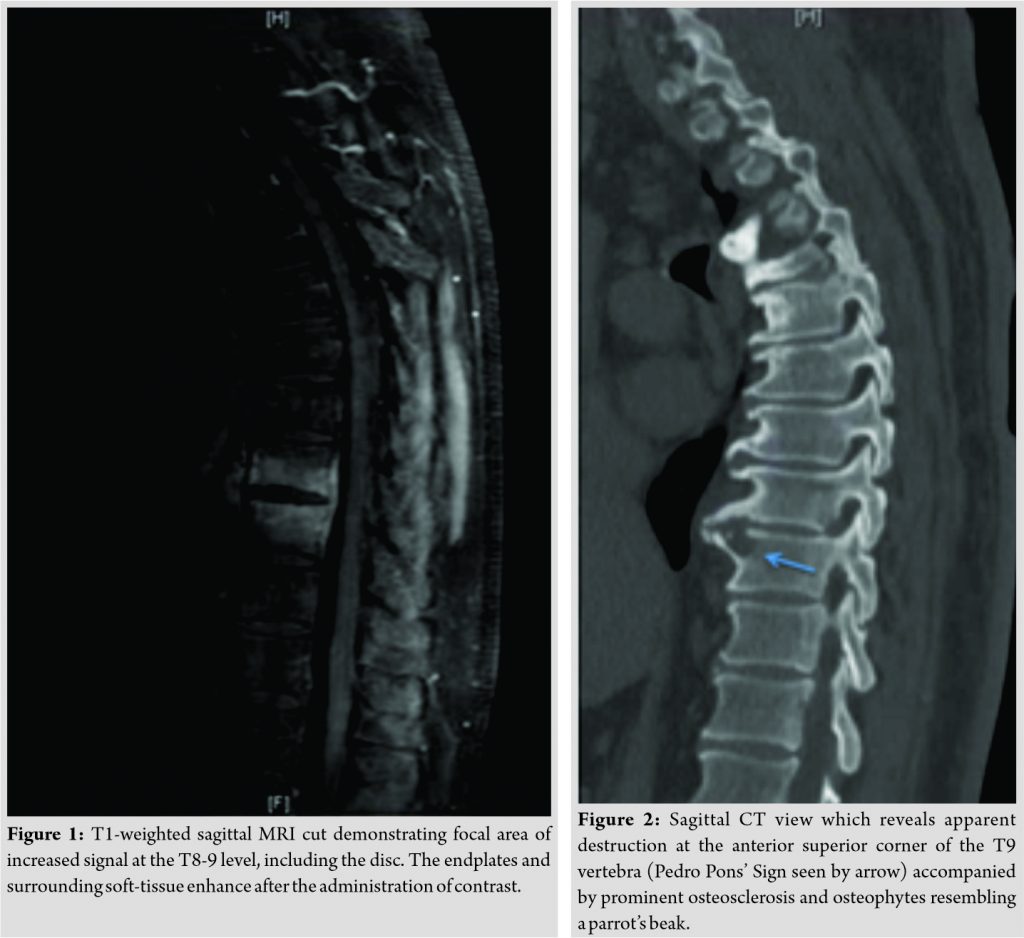
The patient was referred to us for further treatment and evaluation for a potential infection versus malignancy. The patient’s labs were significant for elevated inflammatory markers: Erythrocyte sedimentation rate of 45 and C-reactive protein of 2.1. Notably, the patient had traveled approximately 1 year ago to Mexico to work as a meat slaughterer. Denied any bowel or bladder issues. Denied any current chest pain, abdominal pain, or shortness of breath. Denied any difficulty walking or ambulating. Patient was ultimately told to come to the ED for a workup of his discitis and possible malignancy. On arrival to the emergency department, blood cultures were obtained and the patient was scheduled for a core needle bone biopsy of T9 as well as a core needle biopsy of the T8-T9 disc space, performed by the interventional radiology service. While awaiting results of the biopsy, CT scan was ordered for further work up and evaluation of the patient’s pathology. While admitted, more detailed interviewing ultimately revealed the patient’s work within a Mexican slaughterhouse and regular consumer of unpasteurized Mexican cheeses. With his recent travel, profession exposure, and MRI findings, tuberculosis or Brucella discitis remained at the top of the differential diagnoses.
Discussion
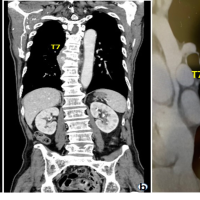
Spinal brucellosis is uncommon in developed nations [15]. Cases that surface in developed nations often arise from patients who have traveled from endemic areas or consumed unpasteurized dairy products [16, 17]. The difficulty in establishing a diagnosis of spinal brucellosis early in its infectious course is the nonspecific and subtle nature of the patient’s symptoms. While clinical symptoms and imaging provide a solid assessment of the patient, a diagnosis of brucellosis cannot be verified unless isolated from the blood, bone marrow, or other tissues [2]. Blood cultures are only positive 53–90% in patients with brucellosis. Thus, a bone marrow or liver culture is suggested due to the propensity of Brucella to survive intracellular killing by macrophage and polymorphonuclear cells in the reticuloendothelial system [18]. Oftentimes, bone biopsy is acquired to verify and further evaluate the micro-organism involved in the patient’s pathology. With regards to our case, the results of his bone biopsy showed non-descript changes that could be minute granulomas within the marrow–increasing the likelihood of Brucella infection. Ultimately, blood cultures grew gram-negative coccobacilli confirming the diagnosis of brucellosis spondylodiscitis. Diagnosis of spinal brucellosis begins with a history. A thorough and detailed history is critical to a timely diagnosis of spinal brucellosis. Inquiring for events that may indicate interaction with farm animals, such as occupational work, or simply visiting endemic areas could indicate possible brucellosis.[5]. Brucella is characterized by an acute phase, with general symptoms such as an undulating fever, weight loss, and fatigue, and a chronic phase, presenting years after initial exposure, characterized by osteomyelitis presenting with spells of back pain, arthralgias, and sweating [1]. There are many different ways that brucellosis presents in the musculoskeletal system including, but not limited to: osteomyelitis, bursitis, tenosynovitis, spondylitis, and sacroiliitis [6]. Targeted sites are variable by age, but the spine is oftentimes targeted in the elderly. In children and young adults, the sacroiliac joints and knee are predominant sites [2]. Clinical symptoms and a proper history can help clue into a diagnosis of brucellar spondylodiscitis infection; however, bone scintigraphy, CT, or MRI can assist with the diagnosis [2]. Of all imaging methods, MRI is the most preferred means of recognizing brucellar spondylodiscitis, as it offers better specificity and can assess the extent of disco-vertebral involvement, in addition to involvement of the soft tissues and epidural space (Fig. 1) [19]. Standard radiographic imaging may reveal focal erosions of the superior or inferior vertebral body angle. This ultimately leads to disc collapse [2]. CT scans are useful to evaluate for potential bony abnormalities, though as stated, MRI scan with and without contrast will assist with the diagnosis, localization of the spondylodiscitis, formation of a potential epidural abscess, or compression of the spine and nerves related to the brucellosis [6, 20]. Also visualized best on MRI are lesions of focal destruction on the anterosuperior corner of the vertebral body, termed “Pedro Pons’ Sign.” This lesion, in addition to prominent osteosclerosis of the vertebral body, is pathognomonic for brucellar spondylodiscitis [6, 21, 22]. The Pedro Pons’ sign was described originally by Pedro-Pons and Farreras in 1944 [22, 23]. They described it as a destructive appearance at the anterosuperior aspect of the vertebral body, with associated osteosclerosis and osteophyte formation. These, in combination, are characteristic findings of brucellar spondylitis [6, 22, 24]. This was evident on imaging of our patient as well (Fig. 2). Brucellar spondylitis remains a diagnosis primarily treated with medical, as opposed to surgical, therapies. The goal of treatment is to appropriately treat the disease, its signs and symptoms, as well as to prevent relapse of the infection. Without destabilization of the spine or development of a cord-compressing abscess, the mainstay of treatment remains long-term IV antibiotics. With respect to spinal spondylodiscitis, long-term anti-microbial therapy is necessary to prevent relapses. Treatment length of brucellar spondylitis has not been standardized, yet treatment should generally past 3–6 months [6]. The most commonly used antibiotics are a triple therapy of doxycycline, rifampin, and an aminoglycoside. Patients who fail conservative treatment with IV antibiotics or who present with neurological deficits necessitate surgical intervention at that time [6, 25, 26]. In our case, the patient received a PICC line for long-term IV antibiotics and was placed on gentamicin for a total of 10 days then transitioning to doxycycline and rifampin for 12 weeks of IV therapy. Patient was seen at follow-up 3 months later with subsidence of his pain, resolution of his fevers, and normalization of his inflammatory markers. Patient was followed up until the 1 year mark, with repeat MRI, indicating resolution of his infectious etiology and overall improvement of symptoms. One limitation of our study was that we did not recognize his exposure to farm animals until after his admission. Regardless of our thorough questioning, it did not surface until days later that he had direct exposure to farm animals which served as a vector for his infection. Although this did not alter his inpatient duration or course, this could have been avoided with direct questioning regarding animal exposure. In addition, though no surgical intervention was needed in this case, clinicians must remain vigilant and cognizant that epidural abscess formation may result from an adjacent discitis and that surgical decompression may be warranted for improved patient outcome.
Conclusion
The most common location of infection of brucellosis is the musculoskeletal system, with a rate of 10–85% [6]. The sacroiliac joints, as well as the lumbar spine, tend to be the most commonly affected sites of infection [6]. Although an uncommon reason for low back pain, it must be considered on the differential diagnosis when working up a patient for lumbar pain. A thorough history and physical exam may suggest an infectious etiology, in which inflammatory markers and advanced imaging can be used to better understand the patient’s pathology and potentially identify radiographic clues, such as the Pedro Pons’ sign, to assist with the diagnosis. Spondylodiscitis is the most severe form of musculoskeletal involvement of brucellosis, due to its potential to develop an epidural abscess, and should be treated emergently with decompression to minimize the risk of long-term neurological damage, if nerve compression occurs. This case and review of the literature discusses critical teaching points to understanding the pathology and treatment algorithm of spinal brucellosis. Brucellosis should continue to be considered as a potential diagnosis for patients with sciatica, axial back pain, and septic arthritis.
Clinical Message
Diagnosing spinal brucellosis can be challenging. These infections may present in an unusual fashion. Although rare, spinal brucellosis must remain as a differential diagnosis in any patient presenting with low back pain and fevers. A detailed evaluation, particularly a thorough history of the patient’s complaints, is essential to properly diagnosing and treating this infection.
References
1. Herrick JA, Lederman RJ, Sullivan B, Powers JH, Palmore TN. Brucella arteritis: Clinical manifestations, treatment, and prognosis. Lancet Infect Dis 2014;14:520-6.
2. Bouaziz MC, Ladeb MF, Chakroun M, Chaabane S. Spinal brucellosis: A review. Skeletal Radiol 2008;37:785-90.
3. Al Anazi M, AlFayyad I, AlOtaibi R, Abu-Shaheen A. Epidemiology of brucellosis in Saudi Arabia. Saudi Med J 2019;40:981-8.
4. Malik GM. A clinical study of brucellosis in adults in the Asir region of Southern Saudi Arabia. Am J Trop Med Hyg 1997;56:375-7.
5. Aydin G, Tosun A, Keles I, Ayaşlioglu E, Tosun O, Orkun S. Brucellar spondylodiscitis: A case report. Int J Clin Pract 2006;60:1502-5.
6. Esmaeilnejad-Ganji SM, Esmaeilnejad-Ganji SM. Osteoarticular manifestations of human brucellosis: A review. World J Orthop 2019;10:54-62.
7. Gangi SM, Roushan MR, Janmohammadi N, Mehraeen R, Amiri MJ, Khalilian E. Outcomes of treatment in 50 cases with spinal brucellosis in Babol, Northern Iran. J Infect Dev Ctries 2012;6:654-9.
8. Lim KB, Kwak YG, Kim DY, Kim YS, Kim JA. Back pain secondary to brucella spondylitis in the lumbar region. Ann Rehabil Med 2012;36:282-6.
9. Nickerson EK, Sinha R. Vertebral osteomyelitis in adults: An update. Br Med Bull 2016;117:121-38.
10. Bozgeyik Z, Aglamis S, Bozdag PG, Denk A. Magnetic resonance imaging findings of musculoskeletal brucellosis. Clin Imaging 2014;38:719-23.
11. Demirci I. Brucella diskitis mimicking herniation without spondylitis; MRI findings. Zentralbl Neurochir 2003;64:178-81.
12. Yilmaz C, Akar A, Civelek E, Köksay B, Kabatas S, Cansever T, et al. Brucellar discitis as a cause of lumbar disc herniation: A case report. Neurol Neurochir Pol 2010;44:516-9.
13. Guglielmino A, Sorbello M, Murabito P, Naimo J, Palumbo A, Lo Giudice E, et al. A case of lumbar sciatica in a patient with spondylolysis and spondylolysthesis and underlying misdiagnosed brucellar discitis. Minerva Anestesiol 2007;73:307-12.
14. Mrabet D, Mizouni H, Khiari H, Rekik S, Chéour E, Meddeb N, et al. Brucellar spondylodiscitis affecting non-contiguous spine levels. BMJ Case Rep 2011;2011:bcr0120113788.
15. Corbel MJ. Brucellosis: An overview. Emerg Infect Dis 1997;3:213-21.
16. Applebaum GD, Mathisen G. Spinal brucellosis in a Southern California resident. West J Med 1997;166:61-5.
17. Yee N, Roach DJ. Infected abdominal aortic aneurysm caused by spinal brucellar infection. AJR Am J Roentgenol 1996;167:1068-9.
18. Yagupsky P. Detection of brucellae in blood cultures. J Clin Microbiol 1999;37:3437-42.
19. Bouaziz MC, Bougamra I, Kaffel D, Hamdi W, Ghannouchi M, Kchir MM. Noncontiguous multifocal spondylitis: An exceptional presentation of spinal brucellosis. Tunis Med 2010;88:280-4.
20. Roushan MRH, Ebrahimpour S, Afshar ZM, Babazadeh A. Cervical spine spondylitis with an epidural abscess in a patient with brucellosis: A case report. J Crit Care Med (Targu Mures) 2019;5:103-6.
21. Mehanic S, Baljic R, Mulabdic V, Huric-Jusufi I, Pinjo F, Topalovic-Cetkovic J, et al. Osteoarticular manifestations of brucellosis. Med Arch 2012;66 Suppl 1:24-6.
22. Tuna N, Ogutlu A, Gozdas HT, Karabay O. Pedro pons’ sign as a brucellosis complication. Indian J Pathol Microbiol 2011;54:183-4.
23. Cordero M, Sanchez I. Brucellar and tuberculous spondylitis. A comparative study of their clinical features. J Bone Joint Surg Br 1991;73:100-3.
24. Wu N, Zhang Y, Yu YS. Pedro pons’ sign of brucellar spondylitis. Rev Soc Bras Med Trop 2020;53:e20190561.
25. Reşorlu H, Saçar S, Inceer BŞ, Akbal A, Gökmen F, Zateri C, et al. Cervical spondylitis and epidural abscess caused by brucellosis: A case report and literature review. Folia Med (Plovdiv) 2016;58:289-92.
26. Solera J, Lozano E, Martinez-Alfaro E, Espinosa A, Castillejos ML, Abad L. Brucellar spondylitis: Review of 35 cases and literature survey. Clin Infect Dis 1999;29:1440-9.
 |
 |
 |
| Dr. James M Rizkalla | Dr. Khalid Alhreish | Dr. Ishaq Y Syed |
| How to Cite This Article: Rizkalla JM, Alhreish K, Syed IY. Spinal brucellosis: A case report and review of the literature. Journal of Orthopaedic Case Reports 2021 March;11(3): 1-5 |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com