[box type=”bio”] What to Learn from this Article?[/box]
Tumor thrombus is a very rare phenomenon associated with giant cell tumors. A high level of suspicion and multimodality treatment at a tertiary care center will result in a better patient outcome.
Case Report | Volume 5 | Issue 4 | JOCR Oct-Dec 2015 | Page 54-56| Ashish Gulia, Ajay Puri, Suman Byregowda, Bharat Rekhi, Siddhartha Laskar, Nitin Shetty. DOI: 10.13107/jocr.2250-0685.346.
Authors: Ashish Gulia[1], Ajay Puri[1], Suman Byregowda[1], Bharat Rekhi[2], Siddhartha Laskar[3], Nitin Shetty[4]
[1]Department of surgical oncology, Tata Memorial Centre, Mumbai, India.
[2]Department of Pathology, Tata Memorial Centre, Mumbai, India.
[3]Department of Raditaion Oncology, Tata Memorial Centre, Mumbai, India.
[4]Department of Intervention Radiology, Tata Memorial Centre, Mumbai, India.
Address of Correspondence
Dr. Ashish Gulia, Associate Professor, Orthopaedic Oncology, Department of surgical oncology, Tata Memorial Centre, Mumbai, India.
Email ID – aashishgulia@gmail.com
Abstract
Introduction: Giant cell tumor is the most common benign lesion encountered. It accounts for 5 % of all skeletal tumors. It mainly affects the epiphysis of long bones and rarely axial bones. In axial bones, sacrum is the most common site to be affected.
Case report: A 23 years old female with giant cell tumor of sacrum was treated initially with conservative treatment (serial angioembolisation and bisphosphonates). Later intralesional curettage was done as the patient started developing bladder and bowel disturbances after two sessions of angioembolisation. Six months later patient again presented with pain at the primary lesion site and bilateral limb swelling. Imaging revealed recurrence of the disease and tumor thrombus extending into the inferior vena cava up to the subhepatic region.
Conclusion: Treatment of sacral GCT (Giant Cell Tumor) poses a unique challenge to the treating surgeon because of the close proximity of vital neurovascular structures, viscera and associated complications related to the disease. Tumor thrombi are a very rare phenomenon associated with giant cell tumors of the bone. High index of suspicion and multimodality approach is the key in treating such challenging tumors and their complications.
Keywords: Sacrum, Giant cell tumor, Tumor thrombus.
Introduction
The sacrum is the most common site for Giant Cell Tumor (GCT) in the axial skeleton accounting for 1.7-8.2% of sacral tumors. Management of sacral GCTs poses a unique challenge because of their anatomic location. Various methods of management are advocated, including curettage with or without adjuvants, complete excision and radiotherapy [1]. The GCT of sacrum can have various complications related to the disease and its treatment, which may include severe pain, distal neuro-vascular compromise, compressive effects on adjacent visceral organs and distant metastasis. We present a previously unreported complication of sacral GCT which led to the formation and propagation of tumor thrombus of GCT in the iliac vein and inferior vena cava. We have also discussed the treatment and follow up of this case.
Case Report
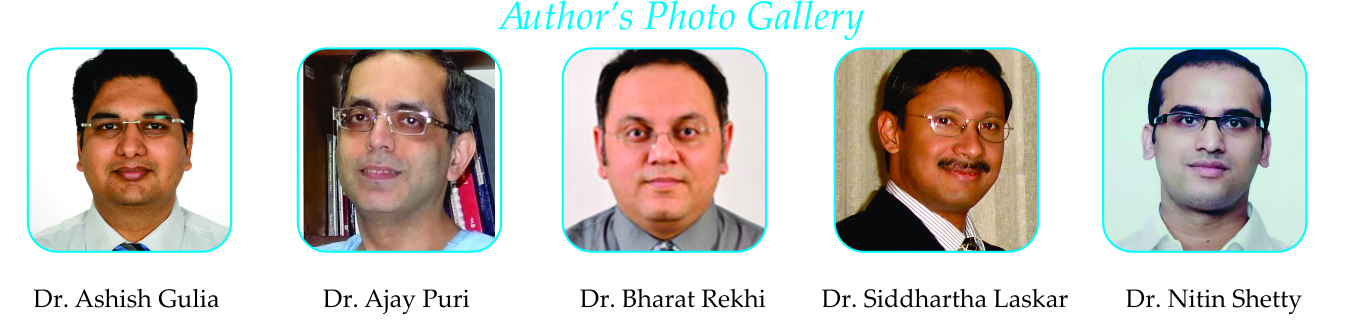
A 23 years old female presented with a history of pain and swelling in her sacral region for four months. Initially it was mild in intensity but gradually progressed to severe, continuous pain necessitating regular use of injectable analgesics. It was radiating to both her lower limbs, more so on the left side. Plain radiograph of pelvis showed an ill-defined osteolytic lesion in the sacrum (Fig 1). Magnetic resonance imaging (MRI) revealed an expansile heterogeneous lesion involving the sacral segments S1, S2 and S3. The lesion was hypo intense on T1 and hyper intense on T2 sequences. It measured 6 x 8 x 4 cm and was extending bilaterally up to the sacroiliac joint, affecting left side more than right (Fig 2). There was compression of sacral nerve roots due to the disease process. All other blood investigations including serum alkaline phosphatase were within normal limits. There was no distal neuro-vascular deficit and the patient had good bowel and bladder control.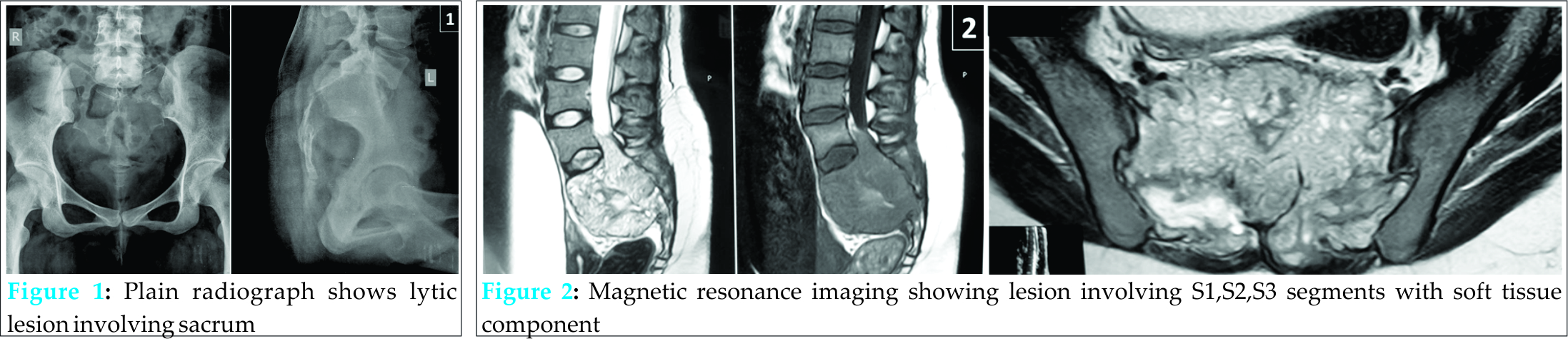
Patient underwent a Computer Tomography (CT) guided biopsy which confirmed the diagnosis of giant cell tumor of bone. Chest radiograph showed no metastasis. The case was discussed in a multidisciplinary clinic in view of the involvement of proximal sacrum, and a decision was made to treat the lesion with serial embolisation and parenteral bisphosphonates (monthly 4 mg of zolendronic acid), as intra lesional surgery would have a very high risk of loss of bowel and bladder functions. After two sessions of embolisation, symptoms were not relived and she developed retention of urine and started having difficulty in passing stools. Repeat MRI scan showed increase in the size of the lesion (7x9x7cm). Patient underwent intra-lesional curettage of the lesion. No chemical or thermal adjuvants were used in order to avoid injury to the neural structures. Patient was put on anticoagulation therapy and was kept under surveillance.
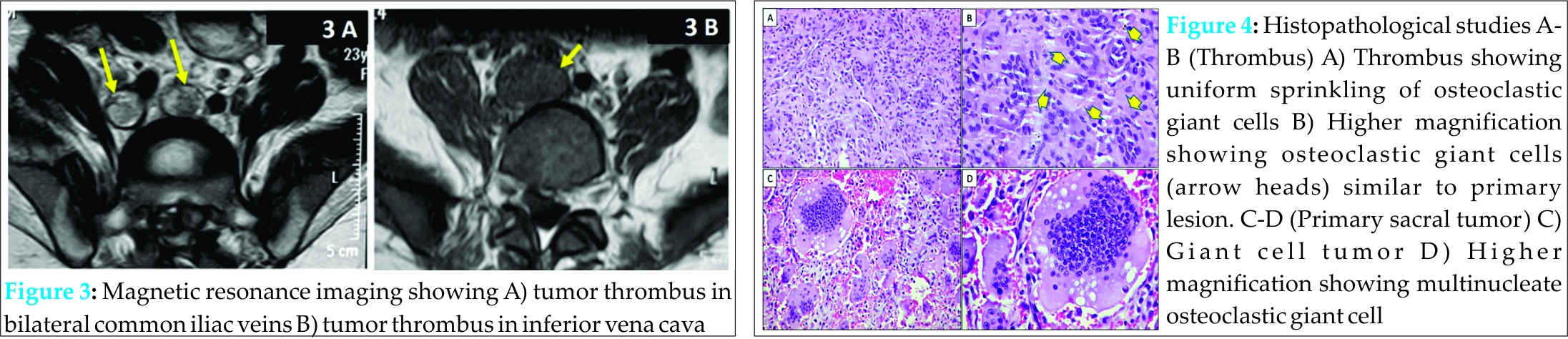
Six months post-surgery, the patient again presented with pain at the primary lesion and bilateral limb swelling. The MRI revealed recurrence of the disease in the sacrum and expansion of the inferior vena cava (IVC) with a non-homogenous intramural mass which had heterogeneous signal intensity in both T1 and T2 images, suggestive of tumor thrombus (Fig 3). This mass was extending superiorly up to sub hepatic region and distally into bilateral common and external iliac veins. A Positron Emission Tomography (PET) scan revealed a hyper metabolic intramural lesion involving right external iliac, bilateral common iliac and inferior vena cava extending up to sub hepatic region with standard uptake value (SUV) of 14.3 which was suggestive of tumor thrombosis. In addition, it also showed a hyper metabolic destructive lesion in sacrum with SUV max of 11.7 which was suggestive of recurrence of disease. An IVC filter was deployed to prevent pulmonary embolism. We placed a retrievable IVC filter through right internal jugular vein and performed thrombo-aspiration from the right femoral vein. Large amount of thrombus was aspirated using an 8 French guiding catheter (Vistabrite, Cordis Corporation). The aspirated thrombus showed characteristic histological features similar to the primary sacral lesion with no evidence of malignant transformation (Fig 4). The sacral recurrence and the infrahepatic IVC tumor thrombus were treated with definitive radiotherapy using helical tomotherapy based Intensity Modulated Radiation Therapy (IMRT). The gross residual mass in the pelvis was treated with a dose of 50Gy/25 fractions at the rate of 2Gy/fraction while the infrahepatic IVC with tumor thrombus received 45Gy/25 fractions at the rate of 1.8Gy/fraction using simultaneous integrated boost technique. The patient was followed up with MRI at regular intervals. At the last follow up 3 years post radiation therapy, she had stable disease with reduction in vena caval obstruction symptoms and complete control of her bowel and bladder movements.
Discussion
Giant cell tumor (GCT) of bone is a rare neoplasm that accounts for approximately 5% of all primary bone tumors in adults. [1] Axial lesions most commonly affect the sacrum. [2] Sacral GCTs usually develop in an eccentric manner but often extend to involve both sides of the midline and involve multiple levels in sacrum. [3]
This case report describes a recurrent giant cell tumor which developed a tumor thrombus post curettage and had extension up to the sub hepatic part of inferior vena cava. To the best of our knowledge this is the first report of inferior vena caval tumor thrombus secondary to giant cell tumor of the bone. There can be two possible hypotheses for tumor propagation 1) tumor dissemination due to curettage 2) direct extension of the disease process through the draining venous plexus. Such incidences have been observed in other malignancies like ovarian cancer, pancreatic and other gastrointestinal malignancies.
Management of sacral GCTs poses a unique challenge because of their anatomic location. Recently, non-surgical methods are becoming more popular as they prevent the surgical morbidity of massive blood loss and neurological deficit. Repeated serial arterial embolization (tumor necrosis due to lack of blood supply) along with third generation bisphosphonates have shown opportune results by their synergistic actions. [4] However, there is still no definitive treatment algorithm for sacral GCTs partly because of their rarity.
The present case was treated on the same function preserving philosophy as stated earlier. Hosalkar et al have shown encouraging results in the treatment of sacral giant cell tumors with serial embolisation [5]. Seven of their nine patients had good control with serial embolisation done every six weeks. Thangaraj et al also advocate the use of serial embolisation for the treatment of sacral giant cell tumors with proximal involvement. They emphasized that for proximal sacral lesions, initial conservative treatment with serial embolisation should always be considered in order to decrease morbidity and preserve majority of functions [6].
After an attempt of non-surgical management and clinico-radiological evidence of disease progression, our patient was treated with curettage of the lesion. In spite of the higher chances of recurrence after curettage (reported by Leggon et al up to 48%) when compared with resection, curettage was our preferred initial mode of surgical treatment in this case as it had a better chance of preserving bowel and bladder function [7]. Six months after curettage the tumor recurred locally, with MRI also revealing presence of thrombus in the common iliac veins and extending up to sub hepatic portion of inferior vena cava. Even though the incidence of venous thromboembolism is high, the tumor thrombosis incidence is low [8]. Inferior vena-caval tumor thrombosis are commonly seen with renal, hepatic and retroperitoneal pathologies like renal cell carcinoma, Ewing’s sarcoma of kidney, hepatocellular carcinomas and retroperitoneal tumors [9]. After an extensive literature search we could not find any other case with inferior vena-caval tumor thrombosis secondary to giant cell tumor. A bland thrombus will have low signal intensity compared with tumor thrombi because of the T2 shortening effect of blood breakdown products. The tumor thrombi shows contrast enhancement, which helps to differentiate it from a bland one [10]. PET scan is also useful in differentiating tumor thrombi from bland ones. Sharma et al found that a cut-off SUV of 3.63 can be used to differentiate benign from tumor thrombus with a sensitivity and specificity of 72% and of 90% respectively [11]. In our case all these radiologic criteria were present and we were also able to confirm the etiology with histopathological examination. Although filter placement was primarily done to prevent spontaneous pulmonary embolism, it also permitted us to perform thrombo-aspiration with reduced risk of massive embolism.
Radiotherapy has been shown to increase the local control in unresectable sacral GCTs [12]. In our case too, radiotherapy helped to arrest tumor progression at the primary site, as well as tumor thrombus in IVC.
In future, Denosumab, a monoclonal antibody to receptor activator of nuclear factor kappa-B ligand (RANKL ) may offer a ray of hope for such patients as it clearly retards osteoclastic activity and may offer symptom and disease control. Though the duration of treatment and long term side effects are still areas of debate for the use of Denosumab, it can be used for the treatment of recurrent and surgically unsalvageable GCT of bone [13].
Conclusion
Sacral tumors should be treated with multimodality management at specialized centers with a function preserving approach. Propagation of tumor thrombus in inferior vena cava is an extremely rare complication of giant cell tumor of sacrum or pelvis. The treating team needs to be aware of the possibility of complications and the possible avenues for management
Clinical Message
Ours is the first case of sacral giant cell tumor reported to have a tumor thrombus in the inferior vena cava and this case report stresses on the importance of a multimodality approach for treating such challenging tumors and their complications.
References
1. Turcotte RE. Giant cell tumor of bone. Orthop Clin North Am 2006;37:35-51.
2. Peh WC, Koh WL, Kwek JW, Htoo MM, Tan PH. Imaging of painful solitary lesions of the sacrum. Australas Radiol 2007;51:507–15.
3. Llauger J, Palmer J, Amores S, Bague´ S, Camins A. Primary tumors of the sacrum: diagnostic imaging. AJR Am J Roentgenol 2000;174:417–24.
4. Puri A, Agarwal MG, Shah M et al. Decision making in primary sacral tumors. Spine J 2009;9:396-403.
5. Hosalkar HS, Jones KJ, King JJ, Lackman RD. Serial arterial embolization for large sacral giant-cell tumors: mid- to long-term results. Spine 2007;32:1107–15.
6. Thangaraj R, Grimer RJ, Carter SR, Stirling AJ, Spilsbury J, Spooner D. Giant cell tumour of the sacrum: a suggested algorithm for treatment. Eur Spine J 2010;19:1189-94.
7. Leggon RE, Zlotecki R, Reith J, Scarborough MT. Giant cell tumor of the pelvis and sacrum: 17 cases and analysis of the literature. Clin Orthop Relat Res 2004;423:196-207.
8. Fennerty A. Venous thromboembolic disease and cancer. Postgrad Med J 2006; 82:642–8.
9. ATsuji Y, Yamashita C, Wakiyama H et al. Surgical treatment for transvenous tumor extension into the heart: four cases. J VascSurg 1998;27:740-4.
10. Akin O, Dixit D, Schwartz L. Bland and tumor thrombi in abdominal malignancies: magnetic resonance imaging assessment in a large oncologic patient population. Abdom Imaging. 2011 Feb;36(1):62-8.
11. Sharma P, Kumar R, Jeph S et al.18F-FDG PET-CT in the diagnosis of tumor thrombus:can it be differentiated from benign thrombus?. Nucl Med Commun 2011;32:782-8.
12. Shi W, Indelicato DJ, Reith J et al. Radiotherapy in the management of giant cell tumor of bone. Am J Clin Oncol 2013;36:505-8.
13. Xu S.F, Adams B. Yu X.C, Xu M. Denosumab and giant cell tumour of bone—a review and future management considerations. Curr Oncol 2013;20:442-7.
| How to Cite This Article: Gulia A, Puri A, Byregowda S, Rekhi B, Laskar S, Shetty N. Inferior Vena Caval Tumor Thrombus in Giant Cell Tumor of Sacrum – An Unusual Complication Treated with Multimodality Management. Journal of Orthopaedic Case Reports 2015 Oct-Dec;5(4): 54-56. Available from: https://www.jocr.co.in/wp/2015/10/01/2250-0685-346-fulltext/ |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com