[box type=”bio”] What to Learn from this Article?[/box]
It is acceptable to select functional bracing for periprosthetic humeral fracture after shoulder arthroplasty without stem loosening, especially in cases where surgical treatment is difficult, such as in elderly patients, and individuals with serious complications or osteopenia.
Case Report | Volume 6 | Issue 2 | JOCR April-June 2016 | Page 3-5 | Nobuo Terabayashi, Kazu Matsumoto, Iori Takigami, Yoshiki Ito DOI: 10.13107/jocr.2250-0685.402
Authors: Nobuo Terabayashi[1], Kazu Matsumoto[1], Iori Takigami[1], Yoshiki Ito[2]
[1] Department of Orthopaedic Surgery, Gifu University Graduate School of Medicine,
Gifu, Japan.
[2] Department of Orthopaedic Surgery, Kizawa Memorial Hospital, Gifu, Japan.
Address of Correspondence
Dr. Nobuo Terabayashi,
1-1 Yanagido, Gifu-city, Gifu, 501-1194 Japan.
E-mail: jirin1022@ybb.ne.jp
Abstract
Introduction: A periprosthetic humeral fracture is rare after shoulder arthroplasty, and such cases have considerable problems. Patients with this kind of fracture are often complicated by osteopenia, other types of severe disease, or are elderly. Surgical treatment of this fracture type carries some risk, and surgeons may be unsure about the most appropriate approach to adopt.
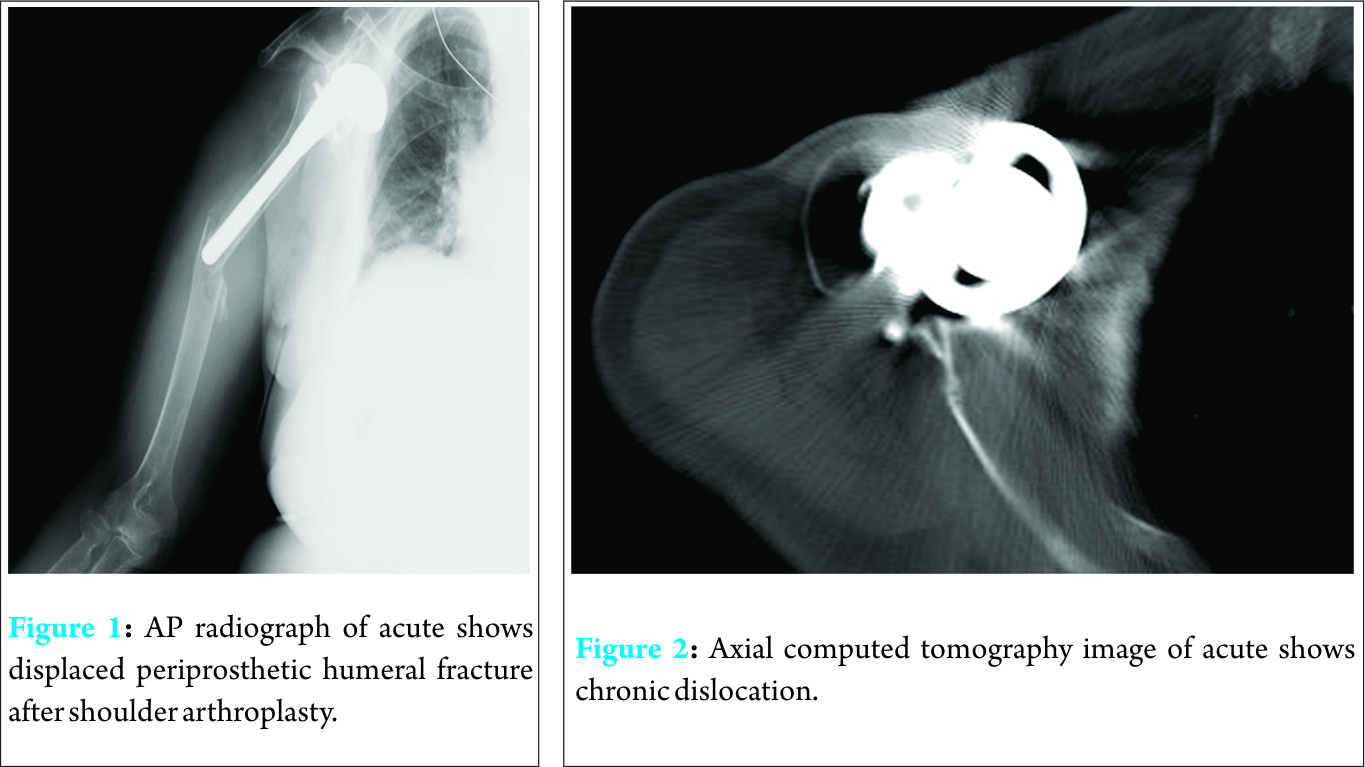
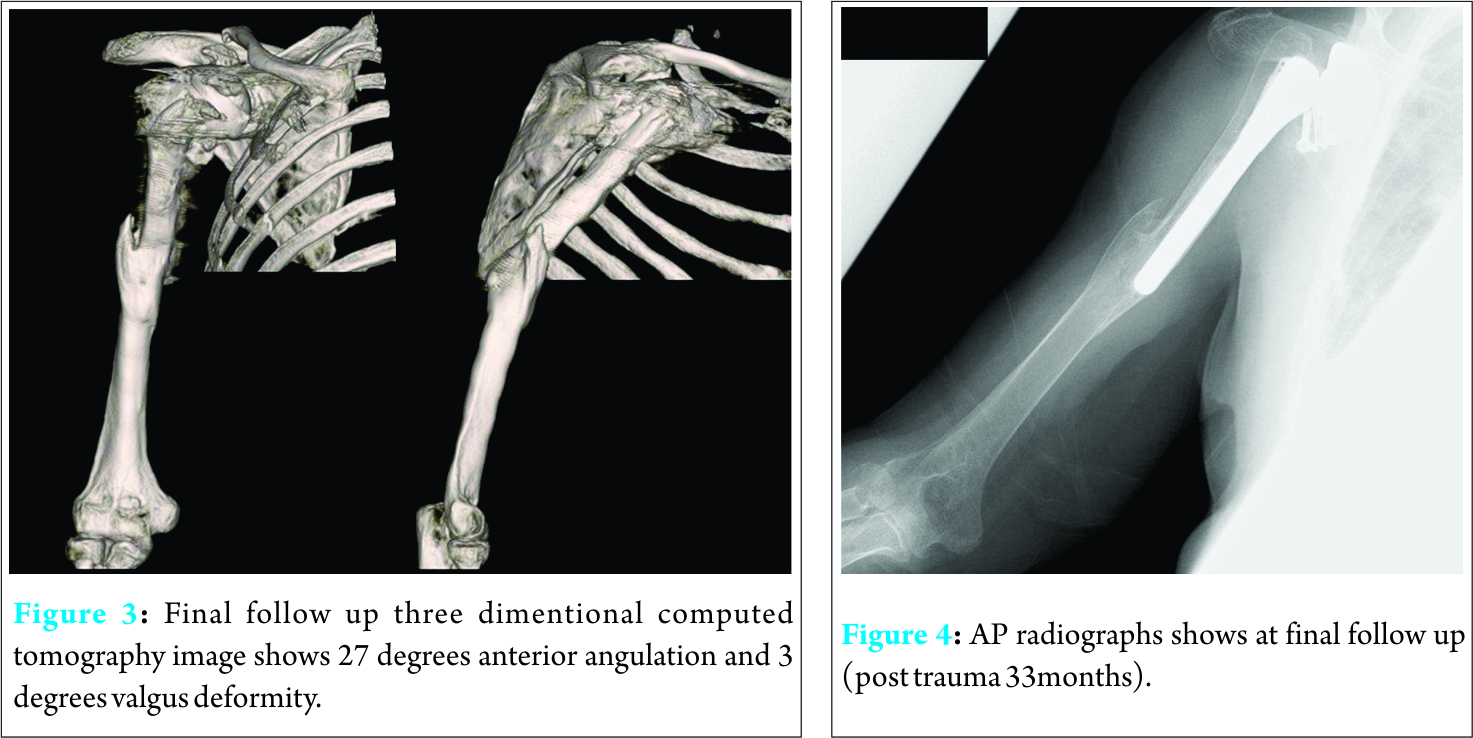
Case report: The present case occurred in a 78-year-old woman with an osteoporotic humeral bone, and chronic dislocation of shoulder after shoulder arthroplasty. There were many risk factors for revision surgery or ostheosynthesis. Therefore, we decided to treat the patient by functional bracing. Fortunately, complete radiographic union was confirmed at 17 weeks. She returned to daily life with good functional activity.
Conclusion: In our opinion, it is acceptable to select functional bracing for periprosthetic humeral fractures after shoulder arthroplasty without stem loosening in elderly patients with an osteoporotic humeral bone.
Keywords: Periprosthetic humeral fracture; functional bracing; osteoporosis; conservative therapy
Introduction
Periprosthetic humeral fracture after shoulder arthroplasty is uncommon, with a prevalence of 1% to 2% [1, 2]. Therefore, such fractures are not encountered often in clinical practice. These fractures are among the most challenging complications of shoulder arthroplasty, and published information about the outcome of treatment is limited. Patients with this fracture are often complicated by osteopenia, other types of severe disease, or are elderly. Surgical treatment of this fracture type carries a certain degree of risk, and surgeons may be unsure about the most appropriate approach to adopt. Essentially, conventional fractures of the humeral diaphysis treated non-surgically have high rate of union with good functional results [3, 4]. However, there have been only a few reports of conservative therapy using functional bracing for periprosthetic humeral fracture after shoulder arthroplasty [5]. The present case occurred in an elderly woman with an osteoporotic humeral bone. Moreover, chronic dislocation had been present after humeral head replacement for a proximal humeral fracture, and there were multiple risk factors for revision surgery or ostheosynthesis. Therefore, we decided to treat the patient by functional bracing. Despite the patient’s unfavorable conditions for fracture healing, she achieved bone union, and returned to daily life with good functional activity. We were able to obtain a good clinical outcome with functional bracing for this case of periprosthetic humeral fracture after shoulder arthroplasty.
Case report
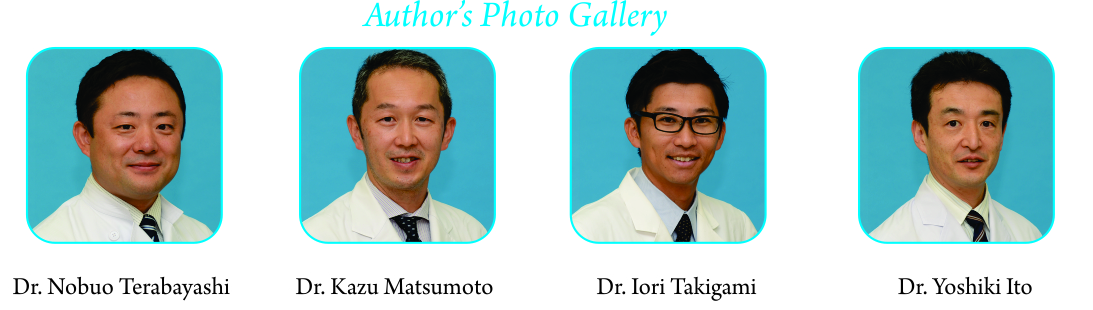
A 78-year-old right hand-dominant woman suffered a fall on her right side in a bicycle accident, and presented at our institution on the same day with severe arm pain. Her medical history included internal fixation for a glenoid fracture 7 years ago, and also hemiarthroplasty (bipolar humeral head type) for a proximal humeral fracture 5 years back. She had also undergone coracoid tip transfer to the glenoid rim for atraumatic postoperative dislocation. All the previous operations had been performed at other hospital. Upon initial presentation, the patient had severe pain in the right arm without vascular or neurological abnormalities, and the right arm was swollen, with deformity. She was not aware of any pain around the shoulder. She stated that although her range of motion in the arm had been limited before the accident, she had been able to live without assistance. Standard radiographs of the humerus revealed a periprosthetic fracture, which was centered at the tip of the prosthesis stem with minimal proximal extension, chronic anterior dislocation, proximal medial side osteolysis, and a thin cortex with osteopenia (Fig. 1 and 2) We considered that surgery might have a considerable risk of complication because of the patient’s advanced age, poor bone condition, and history of multiple operations on the shoulder. Therefore, we decided to follow her up conservatively using functional bracing with routine periodic X-ray examinations. Her arm was immobilized using a plaster U-slab in a sling, to rest the arm and allow the swelling to subside for 2 weeks after the injury. After the swelling had improved, we modeled a functional brace. At 2 weeks after injury, the functional brace was applied without a sling, and physiotherapy was started, with very good patient compliance. The arm pain gradually resolved on a daily basis, but after 3 weeks, radiography showed that the fracture gap had widened. Therefore, we treated this fracture using a sling to prevent any traction force on the fracture site until sufficient callus formation had been achieved. The presence of a callus was confirmed on radiographs after 5 weeks, and use of the sling was continued until 7 weeks after injury. The patient was able to live an almost normal daily life with a functional brace by 10 weeks. Complete radiographic union was confirmed at 17 weeks, and the bracing was then removed. At the final follow-up at 33 months after injury, three-dimensional computed tomography showed anterior angulation of 27 degrees and valgus deformity of 3 degrees (Fig. 3), and radiographs showed no change in alignment at the end of bracing (Fig. 4). The range of motion of the right shoulder was forward flexion to 90°, external rotation at the trunk to 30°, abduction to 90°, and internal rotation to level L2. The patient was relieved of the arm pain, and her level of daily living activity was the same as that before injury.
Discussion
Periprosthetic fracture of the humerus after shoulder arthroplasty is rare, with a reported prevalence between 1.6% [1] and 2.4% [2] . Generally, effective treatment is challenging and difficult, and there have been few reports. Wright and Cofield classified the pattern of such periprosthetic humeral fractures according to their relationship with the distal tip of the implant stem: type A, centered at the tip and extending proximally for more than one-third of the stem length; type B, also centered at the stem tip, but with less proximal extension; type C, involving the humeral shaft distal to the prosthesis tip and extending into the distal humeral metaphysis [6]. Accordingly, the present fracture, which was short and oblique, being located at the stem tip, was type B by this classification. Previous studies have suggested that type C fractures respond favorably to non-operative treatment [2, 6, 7], whereas type A and type B fractures do not. This is because fractures centered at the tip of the prosthesis stem (types A and B) behave in a manner very different from the usual course of a humeral fracture [1, 2, 8]. Conversely, Wright et al. recommended non-operative treatment with a coaptation splint, followed by a plastic orthosis, for type B fractures that have a long oblique or spiral pattern [6]. Kumar et al. reported that a trial of non-operative treatment may be considered for a well-aligned type B fracture that is associated with a well fixed humeral component [7]. The present fracture showed a well fixed humeral component, but was unstable, and the cortex was thin due to osteopenia. Although, radiography it indicated that the condition was not good enough for fracture healing, bone union was fortunately achieved. Sarmiento reported that the use of functional bracing for fractures of the humeral dyaphysis was associated with a high rate of union, particularly when used for closed fractures. The residual angular deformities were usually functionally and aesthetically acceptable [3, 4]. However, periprosthetic humeral fracture after arthroplasty is rare, there are a few reports describing conservative therapy. Kim et al. reported good clinical results using a functional brace for two cases of periprosthetic humeral fracture after shoulder arthroplasty with a very poor general condition and poor bone quality. Both cases were type B and unstable [5]. Several authors have also recommended surgical treatment [1, 6, 8]. Other than the shoulder, there have been many reports on periprosthetic femoral fracture, for which there seems to be a consensus on surgical treatment [9, 10]. Periprosthetic fractures located at the tip of the stem differ from conventional fractures due to the presence of an intramedullary stem. Therefore, there is some concern that the fracture site might not receive enough blood flow; furthermore, the degree of bone fragment contact is lower than in a conventional fracture. However, functional bracing for humeral fracture is an established conservative therapy. Moreover, there has been a good clinical outcome for open fracture cases, and also cases of high-energy trauma such as gunshot injury, which are just as unusual as humeral shaft fractures [3]. Therefore, we consider it acceptable to select functional bracing for periprosthetic humeral fracture after shoulder arthroplasty without stem loosening, especially in cases where surgical treament is difficult, such as in elderly patients, and individuals with serious complications or osteopenia. Sarmiento considered that manipulation of fractures of the humeral diaphysis is not necessary when functional bracing is employed. They reported that the triceps, brachialis, and biceps muscle show coiling of their fibers as the bone fragments rotate after injury, whereas they recoil as the muscles contract during activity. This recoiling appears to align the fragments in a parallel direction, thus correcting any malrotation [3]. As our patient had suffered chronic dislocation of the shoulder and undergone a post-coracoid tip transfer procedure, we were seriously concerned about non-functional recoiling. However, although some anterior angulation deformity remained, the fracture healed. We speculate that the anterior angulation deformity might have been due to a change in biceps muscle function resulting from chronic dislocation and the coracoid tip transfer procedure.
Conclusion
Periprosthetic humeral fracture is rare, and among the most challenging complications of shoulder arthroplasty. Surgical treatment is especially difficult for elderly and frail patients with osteopenia. However, a few previous reports have suggested the use of conservative therapy [5, 6]. Although our patient was considered a poor candidate for fracture healing, bone union was successful with conservative therapy using a functional brace with careful follow-up.
Clinical Message
Periprostetic humeral fracture may need a surgical procedure. However, some cases amongst these are elderly and frail patients. Therefore, in our opinion it is acceptable to select functional bracing for periprosthetic humeral fractures occurring after shoulder arthroplasty without stem loosening.
References
1. Boyd A.D., Jr., Thornhill T.S., and Barnes C.L.. Fractures adjacent to humeral prostheses. J Bone Joint Surg Am 1992;74(10): 1498-504.
2. Worland R.L., Kim D.Y., and Arredondo J.. Periprosthetic humeral fractures: management and classification. J Shoulder Elbow Surg. 1999;8(6): 590-4.
3. Sarmiento, A., et al., Functional bracing for the treatment of fractures of the humeral diaphysis. J Bone Joint Surg Am 2000;82(4): 478-86.
4. Sarmiento, A., et al. Functional bracing of fractures of the shaft of the humerus. J Bone Joint Surg Am 1977; 59(5): 596-601.
5. Kim, D.H., Clavert P., and Warner J.J, Displaced periprosthetic humeral fracture treated with functional bracing: a report of two cases. J Shoulder Elbow Surg 2005;14(2): 221-3.
6. Wright, T.W. and Cofield R.H. Humeral fractures after shoulder arthroplasty. J Bone Joint Surg Am 1995;77(9): 1340-6.
7. Kumar, S., et al. Periprosthetic humeral fractures after shoulder arthroplasty. J Bone Joint Surg Am 2004; 86-A(4): 680-9.
8. Bonutti, P.M. and Hawkins R.J. Fracture of the humeral shaft associated with total replacement arthroplasty of the shoulder. A case report. J Bone Joint Surg Am 1992;74(4): 617-8.
9. Fink B., Fuerst M., and Singer J. Periprosthetic fractures of the femur associated with hip arthroplasty. Arch Orthop Trauma Surg 2005;125(7): 433-42.
10. Pike, J., et al., Principles of treatment for periprosthetic femoral shaft fractures around well-fixed total hip arthroplasty. J Am Acad Orthop Surg 2009;17(11): 677-88.
| How to Cite This Article: Terabayashi N, Matsumoto K, Takigami I, Ito Y. Treatment of Humeral Fracture after Shoulder Arthroplasty using Functional Brace: A Case Report. Journal of Orthopaedic Case Reports 2016 April – June;6(2): 3-5. Available from: https://www.jocr.co.in/wp/2016/04/01/2250-0685-402-fulltext/ |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com