[box type=”bio”] What to Learn from this Article?[/box]
HTO non-union can be successfully treated with revision plating and autologous bone grafting with the main objectives of restoring alignment, preserving bone stock and effecting bone healing.
Case Report | Volume 6 | Issue 3 | JOCR July-Aug 2016 | Page 91-93 | Tan Shi Ming, Wong Merng Koon DOI: 10.13107/jocr.2250-0685.530
Authors: Tan Shi Ming[1], Wong Merng Koon[1]
[1]Department of Orthopaedic Surgery, Singapore General Hospital, Singapore.
Address of Correspondence
Dr. Tan Shi Ming,
Blk 310A Ang Mo Kio Ave 1 #04-387 Singapore 561310.
E-mail: tshiming@hotmail.com
Abstract
Introduction: Uni-compartmental knee arthritis may be treated with several surgical options including uni-compartmental knee arthroplasty, total knee arthroplasty and high tibial osteotomy. Non-union is a well-established and common complication that may arise from the latter option and few reports have shown successful treatment of persistent non-union of high tibial osteotomy.
Case Presentation: We present a case of persistent non-union after high tibial osteotomy treated with autologous iliac crest bone grafting and revision plating. At 1 year post-operative interval, successful union was achieved after revision internal fixation. In addition, a good functional outcome was achieved.
Conclusion: In this patient with persistent non-union following high tibial osteotomy, the aim of revision was to restore alignment and effect bone healing while preserving adequate tibial bone stock. Revision plating with autologous bone grafting is a good surgical strategy in the treatment of persistent non-union with hardware failure.
Key Words: High Tibial Osteotomy, Non-union, Bone Graft, Revision
Introduction
Uni-compartmental varus osteoarthritis in young and active patients has always proven to be a surgical challenge. High tibial osteotomy has become a widely accepted extra-articular, biological option with high survival rates at 5 year and good functional outcomes [1]. The theoretical advantages of opening wedge high tibial osteotomy include greater precision in intraoperative angular correction, obviation of need for lateral dissection and fibular osteotomy with reduced risk of common peroneal nerve palsy, a less invasive surgical approach and absence of lateral knee instability. Despite these advantages, several authors have reported complications associated with opening wedge high tibial osteotomies [2-8], including infection, deep vein thrombosis, lateral tibial plateau fracture, common peroneal nerve palsy, non-union, delayed union, loss of correction and vascular injuries. The incidence of non-union after HTO has been reported to be as high as 5.7% [9, 10]. In this report, we highlight the treatment of persistent non-union in a high tibial osteotomy case with the use of autologous bone grafting and revision plating.
Case Presentation
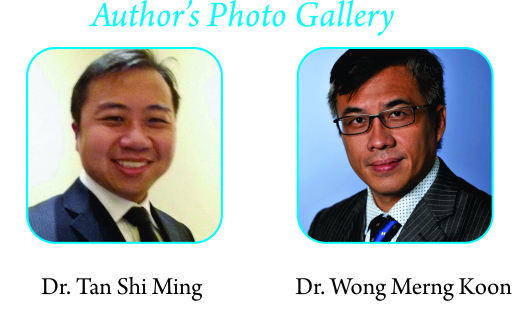
A 53-year-old Chinese lady, with a history of hypertension, diabetes mellitus and chronic depression, presented with an 8 month duration of severe medial right knee pain associated with varus knee deformity. Pain was exacerbated on walking and standing. She was initially treated conservatively with a course of non-steroidal inflammatory drugs, intra-articular visco-supplementation, physiotherapy and weight loss regime. Despite a two-year trial of non-surgical therapy, she continued to experience a deterioration in her symptoms with limitation of her functional status requiring a quadstick as a walking aid. Clinical examination revealed bilateral genu varum. Range of motion was limited to 0 to 110° with no fixed flexion deformity found bilaterally. Significantly, there was medial joint line tenderness and absence of lateral joint line and patellofemoral tenderness. Minimal effusion was found in the right knee. No limb length discrepancy or varus knee thrust was found. Bilateral weight-bearing knee and long limb radiographs were performed (Fig. 1). Significant medial compartment radiographic osteoarthritic changes were noted in the right knee, corresponding to Kellgren-Lawrence grade 3 osteoarthritis. These changes included loss of medial joint space, varus knee deformity and the presence of marginal osteophytes. The femoral-tibial angle measured was 175° and the anatomical lateral distal femoral angle was 86°. We performed a diagnostic knee arthroscopy and then proceeded to an opening wedge high tibial osteotomy using the Tomofix plate after a failed two year trial of conservative therapy (Fig. 2). Arthroscopic findings include medial compartment Outer bridge grade 4 lesion with degenerate radial tear of the posterior horn of the medial meniscus. The lateral compartment had no cartilage or meniscal tear. Intra-operative correction with the opening wedge osteotomy was guided with the use of radiographic imaging. Post-operatively, she was started on a rehabilitation programme, progressing to partial weight bearing at about 6 weeks. 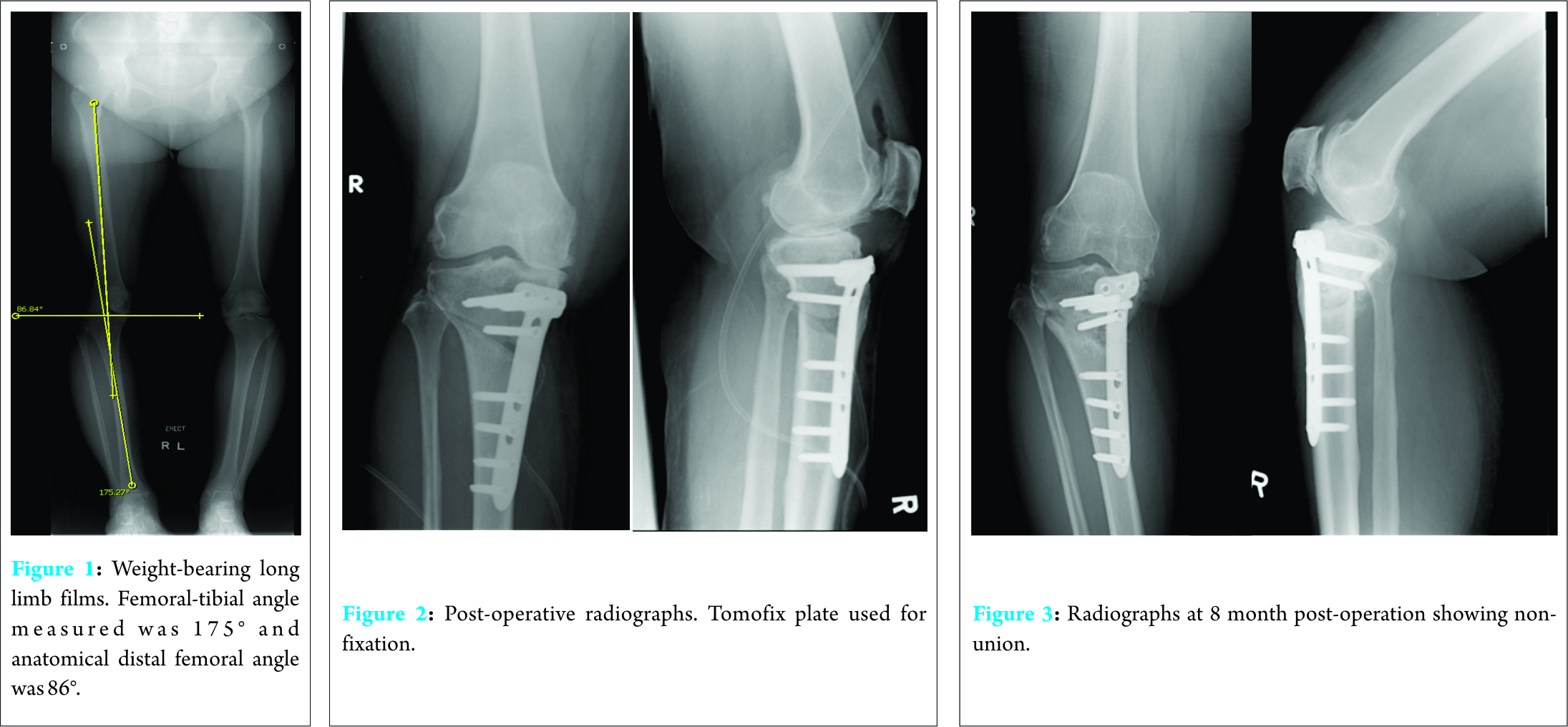
However, she continued to experience pain over the osteotomy site up till 6 months post-operatively. Pain was exacerbated on standing and ambulation. Repeat radiographs showed minimal callus formation over previous osteotomy site (Fig. 3). She was treated conservatively with continued protected weight bearing. However, her symptoms deteriorated and she developed a fix flexion deformity of her right knee. A computed tomogram performed 8 month post-operatively revealed non-union of the osteotomy site with hardware failure and loss of correction (Fig. 4). Three proximal screws were broken and 1 screw had back-out. The proximal tibia was angulated laterally in varus and anteriorly increasing the tibial plateau slope. Inflammatory markers were not elevated. 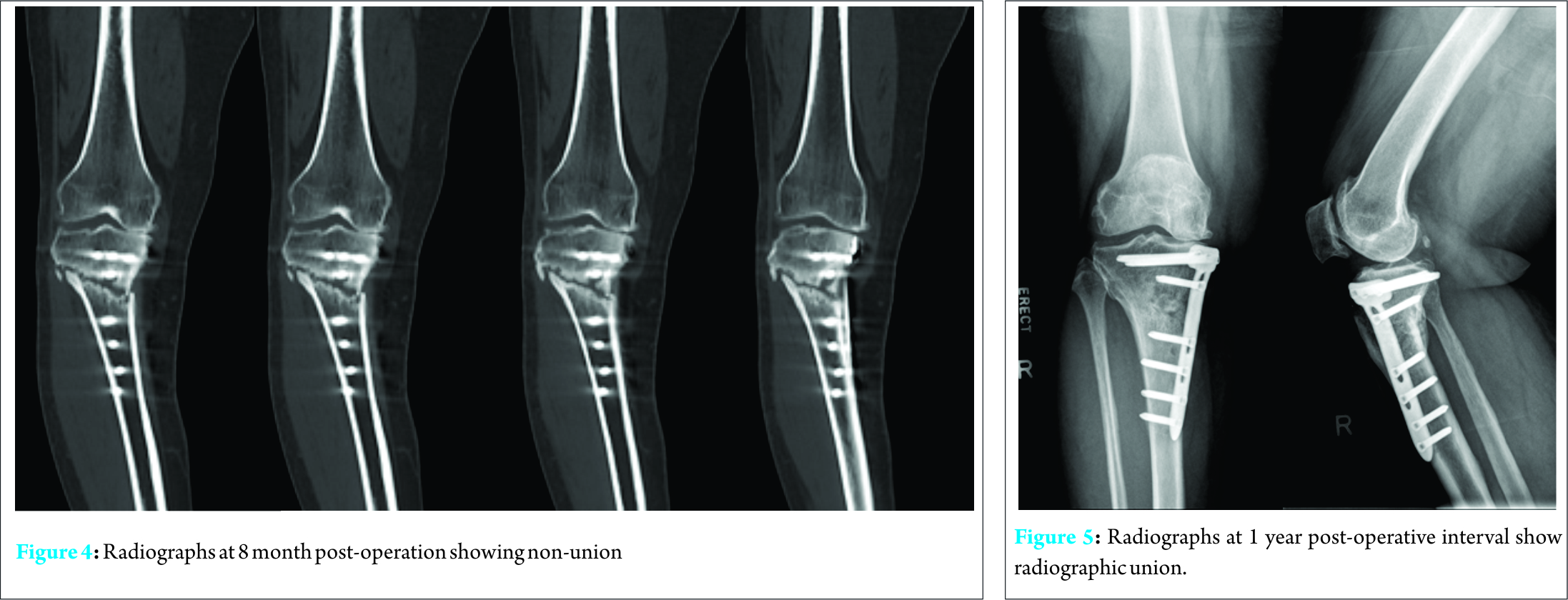
The patient subsequently underwent revision plating with autologous bone graft. The surgical approach was similar to the index surgery. Intra-operatively, findings were consistent with CT scan results. The screws were completely removed together with the Tomofix plate. Bone edges were freshened and the alignment was corrected under radiographic imaging guidance. Autologous cancellous iliac crest bone grafts were harvested and compacted into the osteotomy site. A proximal tibial locking plate was placed on the posteromedial aspect and locking screws were used to secure the fixation. The previous plate was medial. Intraoperative cultures sent were negative for infection. Post-operatively, the patient progressed from non-weight bearing to partial weight bearing at 3 months and full weight-bearing at 6 months post-operatively. She no longer experienced pain at the osteotomy site and repeat radiographs performed at 1 year post-operatively showed union (Fig. 5). She was able to ambulate without any walking aids and no longer has any limitations in her daily activities.
Discussion
Non-union is an uncommon complication associated with opening wedge high tibial osteotomy [5, 7, 9, 10]. Some authors have advocated non-operative treatment with a regimen of protected weight bearing to achieve union. In a study by Martin et al [11] looking at the adverse events following high tibial osteotomy, 3.2% (10/317) of cases were complicated by non-union (defined as absence of radiographic non-union at 6 months) and 1% of cases had hardware failure and loss of correction. In this retrospective review, non-operative treatment with continued protected weight bearing regimen was able to achieve union in 7 out of 10 patients. Three patients underwent revision surgery for aseptic non-union with the use of either autologous iliac crest bone grafting or allograft. All 3 patients had further supplementation either with BMP-2, BMP-7 or platelet-rich plasma. Active smokers were found to have a higher rate of non-union (4.8%) as compared to ex-smokers (4.3%) and non-smokers (2.4%) while diabetic patients were also found to have a higher rate of non-union (16.6%) than non-diabetic patients (2.6%). Various surgical options have been utilized in the treatment non-union after high tibial osteotomy including internal fixation with bone grafting [10, 12], external fixation with grafting including the use of Ilizarov external fixator [13-15] and staged total knee arthroplasty [16]. In a high tibial osteotomy, the metaphyseal location of the non-union site makes the achievement of stable fixation difficult because of the transverse plane of the non-union and a small proximal fragment. A major disadvantage of utilizing external fixation is the inability to provide adequate rotational stability as the small proximal fragment has little room for multiple Steinman pin fixation. Furthermore, external fixation may introduce pin site infections, potentially converting an aseptic non-union to a septic non-union. A 3rd disadvantage would be the loss of correction with pin-site loosening. Wolff et al in his series of 6 cases reported successful outcomes with the use of internal fixation and bone grafting. Internal fixation obviates the need for pin sites and reduces the risk of infection and chronic osteomyelitis. With the primary goal of effecting bone healing over the non-union site and preserving tibial bone stock for a subsequent total knee arthroplasty, internal fixation with bone grafting provides a very good option in achieving these aims.
Conclusion
Our patient experienced persistent non-union despite conservative measures, thus, in our case the aim of the revision with internal fixation using a proximal locking plate was to restore alignment and effect bone healing. Tibial bone stock had also been preserved. Additionally, she was able to achieve a good functional outcome. Revision plating with autologous bone grafting is a good surgical strategy in the treatment of persistent non-union with hardware failure.
Clinical Message
Persistent non-union following a high tibial osteotomy presents a unique surgical challenge. With wide ranging considerations including achieving union and restoring alignment while preserving bone stock, revision plating with autologous bone grafting remains a key strategy in treating such cases.
References
1. Bode G, Von Heyden J, Pestka J, Schmal H, Salzmann G, Südkamp N, Niemeyer P. Prospective 5-year survival rate data following open-wedge valgus high tibial osteotomy. Knee Surg Sports TraumatolArthrosc. 2015 ;23(7):1949-55.
2. Spahn G. Complications in high tibial (medial opening wedge)osteotomy. Arch Orthop Trauma Surg 2003;124:649-653.
3. Hernigou P, Ma W. Open wedge tibial osteotomy with acrylic bone cement as bone substitute. Knee 2001;8:103-110.
4. Warden SJ, Morris HG, Crossley KM, Brukner PD, Bennell KL. Delayed- and non-union following opening wedge high tibial osteotomy: Surgeons’ results from 182 completed cases. KneeSurg Sports Traumatol Arthrosc 2005;13:34-37.
5. Staubli AE, De Simoni C, Babst R, Lobenhoffer P. TomoFix: A new LCP-concept for open wedge osteotomy of the medial proximal tibia—Early results in 92 cases. Injury 2003;34 (2):B55-62.
6. Amendola A, Fowler PJ, Litchfield R, Kirkley S, Clatworthy M. Opening wedge high tibial osteotomy using a novel technique: Early results and complications. J Knee Surg 2004;17:164-169.
7. Bauer T, Hardy P, Lemoine J, Finlayson DF, Trainer S, Lortat-Jacob A. Drop foot after high tibial osteotomy: A prospective study of aetiological factors. Knee Surg Sports Traumatol Arthrosc 2005;13:23-33.
8. Lobenhoffer P, Agneskirchner JD. Improvements in surgical technique of valgus high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc 2003;11:132-138.
9. Naudie D, Bourne RB, Roraback CH, Bourne TJ. Survivorship of the high tibial valgus osteotomy: a 10-to-22 year followup study. ClinOrthopRelat Res 1999;367:18–27.
10. Wolff AM, Krackow KA. The treatment of nonunion of proximal tibial osteotomy with internal fixation. ClinOrthopRelat Res 1990;250:207–15.
11. Martin R, Birmingham TB, Willits K, Litchfield R, Lebel ME, Giffin JR. Adverse Event Rates and Classifications in Medial Opening Wedge High Tibial Osteotomy. Am J Sports Med. 2014 ;42(5):1118-26
12. Cameron HU, Welsh RP, Jung Y-B, Noftall F. Repair of nonunion of tibial osteotomy. ClinOrthopRelat Res 1993;287:167 9.
13. Schatzker J, Burgess RC, Glynn MK. The management of nonunions following high tibial osteotomy. ClinOrthopRelat Res 1985;193:230–3.
14. Tjornstrand B, Hagstedt B, Persson BM. Results of surgical treatment for non-union after high tibial osteotomy in osteoarthritis of the knee. J Bone J Surg Am 1978;60:973–7.
15. Gillooly JJ, Tilkeridis K, Simonis RB, Monsell F. The treatment of high tibial osteotomy non-union with the Ilizarov external fixator. Strategies Trauma Limb Reconst. 2012;7(2):93-7
16. Yoshino N, Takai S, Watanabe Y, Nakamura S, Kubo T. Total knee arthroplasty with long stem for treatment of nonunion after high tibial osteotomy: a case report. J Arthroplast 2004;19:528–31.
| How to Cite This Article: Tan Shi Ming, Wong Merng Koon. Autologous Bone Grafting and Revision Plating in a Case of Persistent High Tibial Osteotomy Non-Union. Journal of Orthopaedic Case Reports 2016 July-Aug;6(3): 91-93. Available from: https://www.jocr.co.in/wp/2016/07/10/2250-0685-530-fulltext/ |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com