[box type=”bio”] What to Learn from this Article?[/box]
Selective cyclooxygenase-2 inhibitors can be employed as HO prophylaxis after arthroscopic hip surgery.
Case Report | Volume 7 | Issue 1 | JOCR January – February 2017 | Page 20-23 | Yaniv Warschawski, Zachary T. Sharfman, Eyal Amar, Ehud Rath. DOI: 10.13107/jocr.2250-0685.670
Authors: Yaniv Warschawski[1], Zachary T. Sharfman[1], Eyal Amar[1], Ehud Rath[1]
[1] Department of Orthopaedics, Tel-Aviv Sourasky Medical Center and the Sackler Faculty of Medicine, Tel Aviv University, Tel Aviv, Israel.
Address of Correspondence
Dr. Zachary T. Sharfman,
Division of Minimally Invasive Orthopedic Surgery, Department of Orthopedic Surgery, Tel Aviv Sourasky Medical Center and the Sackler Faculty of Medicine, Tel Aviv University, Tel Aviv, Israel. Tel.: 972-58-7015762. Fax: 972-3-6973065.
E-mail: zachsharfman@gmail.com
Abstract
Introduction: Heterotopic ossification (HO) after hip surgery is the formation of bone in non-skeletal tissue, usually between the muscle and the joint capsule. HO after hip surgery may be associated with clinical sequelae such as pain, impingement and decreased range of motion, compromising surgical outcomes.
Case Report: A 20-year-old basketball player presented with a 2-year duration of the left groin pain after a basketball-related injury. Due to continued disability and failure of conservative management the patient underwent hip arthroscopy. No HO prophylaxis was given. Follow-up radiographs at 3 months after left hip arthroscopy showed Grade 3 HO on the left side. On the 2nd post-operative visit, the patient complained of contralateral (right-sided) hip pain. Due to continued symptoms on the right side and failure to respond to conservative management the patient underwent right hip arthroscopy. HO prophylaxis was initiated with non-steroidal anti-inflammatory medications (NSAIDs) treatment (Etodolac) 600 mg/day for 14 days. Follow-up radiographs at 3 months after the right hip arthroscopy showed no HO.
Conclusion: This case demonstrates the efficacy of HO prophylaxis in a single patient. Routine HO prophylaxis with NSAIDs should be considered for patients undergoing hip arthroscopy with osteoplasty. A minimum of 9 weeks post-operative follow-up is recommended to assess the radiographic presence of HO.
Keywords: Case report, heterotopic ossification, hip arthroscopy.
Introduction
Heterotopic ossification (HO) after hip surgery is the formation of bone in non-skeletal tissue, usually between the muscle and the joint capsule. The mechanism and etiology of HO remain unclear. The lesion arises from the primitive mesenchymal cells, present at the site of injury, that are activated by the inflammatory mediators released from the injured tissue [1]. The interaction between injured periosteum and necrotic or damaged muscle may accelerate ectopic bone formation [2]. The clinical manifestations of HO have a wide spectrum. Lesions range from small clinically insignificant foci of ossification to large deposits of bone. HO after hip surgery may be associated with clinical sequelae such as pain, impingement, and decreased range of motion compromising surgical outcome. The reported rates of HO after hip arthroscopy without prophylaxis may be as high as 44% [3, 4, 5, 6, 7, 8]. Low dose irradiation and non-steroidal anti-inflammatory medications (NSAIDs) are two common prophylactic methods used to prevent post-operative HO. Non-steroidal anti-inflammatory medications are effective in decreasing the formation of HO by suppressing the inflammatory process [9, 10]. Randelli et al. [2] demonstrated that NSAID prophylaxis after arthroscopic femoroacetabular impingement treatment were effective in preventing HO. Amar et al. [11] did not find capsular closure to be a contributing factor to the formation of HO after hip arthroscopy. This paper presents the case of a patient treated with arthroscopic femoroacetabular osteoplasty and labral repair bilaterally. The patient received NSAID HO prophylaxis after the second surgery but did not receive any HO prophylaxis for the first procedure. The patient developed Grade 3 HO only on the non-prophylactic side. The clinical presentation, imaging, and intraoperative findings are described.
Case Report
Informed consent was obtained from the patient for the use of all images and publication of this report before the beginning of this project. A 20-year-old basketball player presented with a 2-year duration of the left groin pain after a basketball-related injury. The pain was aggravated by athletic activity and prolonged sitting. Physical examination of the left hip showed pain with hip external rotation at 40° and internal rotation at 10°. Radiographs showed a lateral center-edge angle of 36° and an alpha angle of 83° on the anterior–posterior (AP) and 72° on the frog view (Fig. 1 and 2). Due to continued disability and failure of conservative management, the patient underwent hip arthroscopy.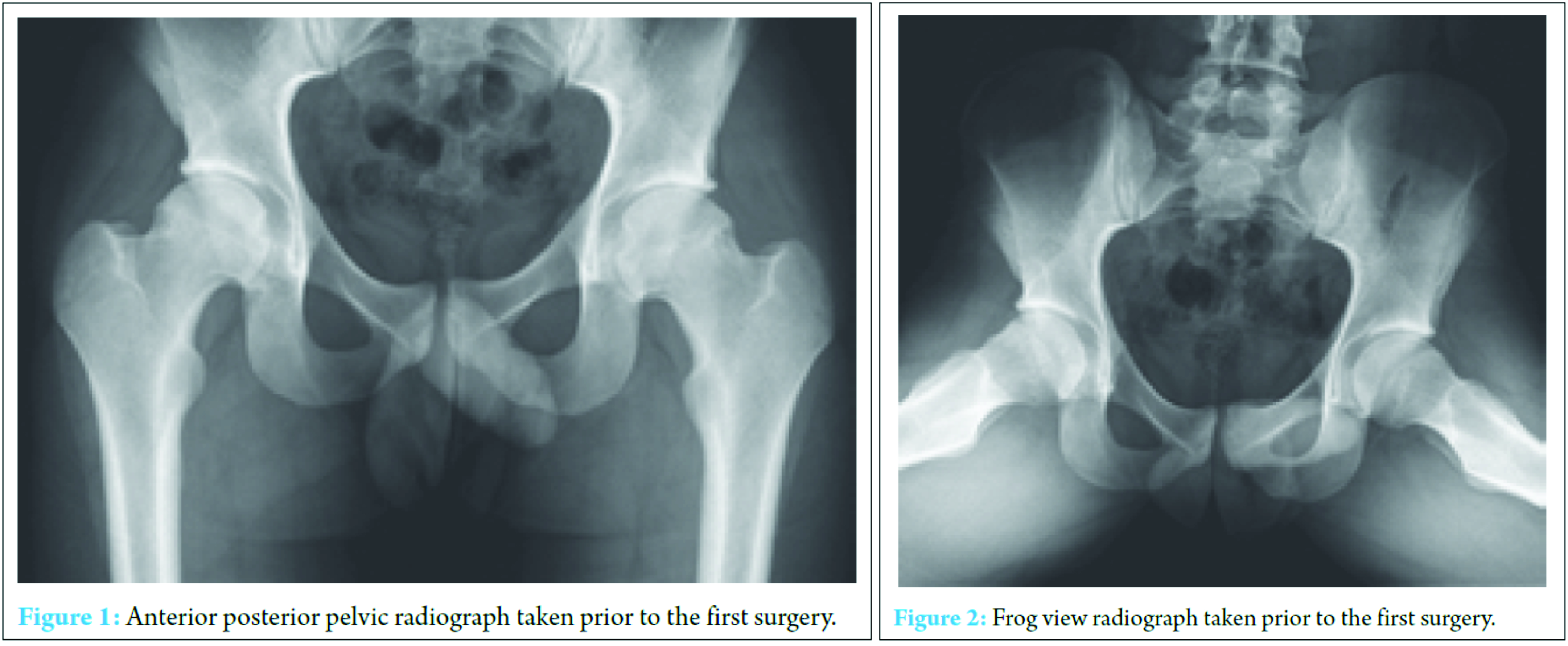
Intraoperative findings included chondral detachment at the chondrolabral junction in zone 3 and an adjacent partial labral tear. These were treated with chondroplasty, microfracture, acetabular osteoplasty and labral repair followed by osteoplasty of the femoral head-neck junction. No HO prophylaxis was given. Follow-up radiographs at 3 months after the left hip arthroscopy showed Grade 3 HO on the left side (Fig. 3 and 4). On the 2nd post-operative visit (following 6 weeks of non-weight bearing rehabilitation) the patient complained of contralateral (right-sided) hip pain.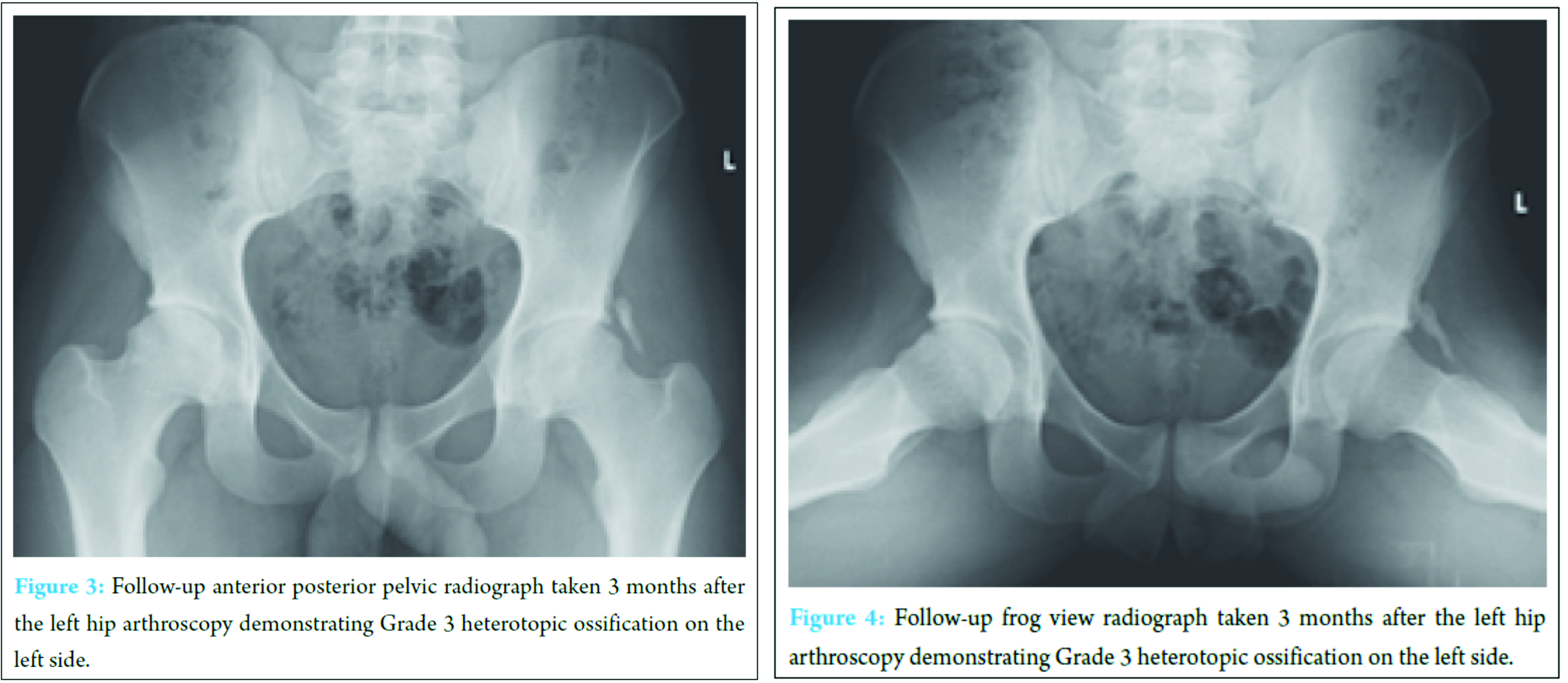
At 6 months, the patient returned his regular basketball activity with no left hip pain. Left hip external rotation and internal rotation improved to 60° and 30° respectively. However, in the right hip, the patient had a positive impingement test with pain on flexion, adduction, and internal rotation and flexion, abduction, and external rotation. AP radiographs showed a lateral center-edge angle of 30° and an alpha angle of 84° in the right hip. Due to continued symptoms on the right side 1 year after the left hip arthroscopy and failure to respond to conservative management the patient underwent right hip arthroscopy. Acetabular osteoplasty and labral repair were followed by osteoplasty of the femoral head-neck junction. Subsequently, HO prophylaxis was initiated with NSAID treatment (Etodolac) 600 mg/day for 14 days. Follow-up radiographs at 3 months after the right hip arthroscopy showed no HO (Grade 0) (Fig. 5).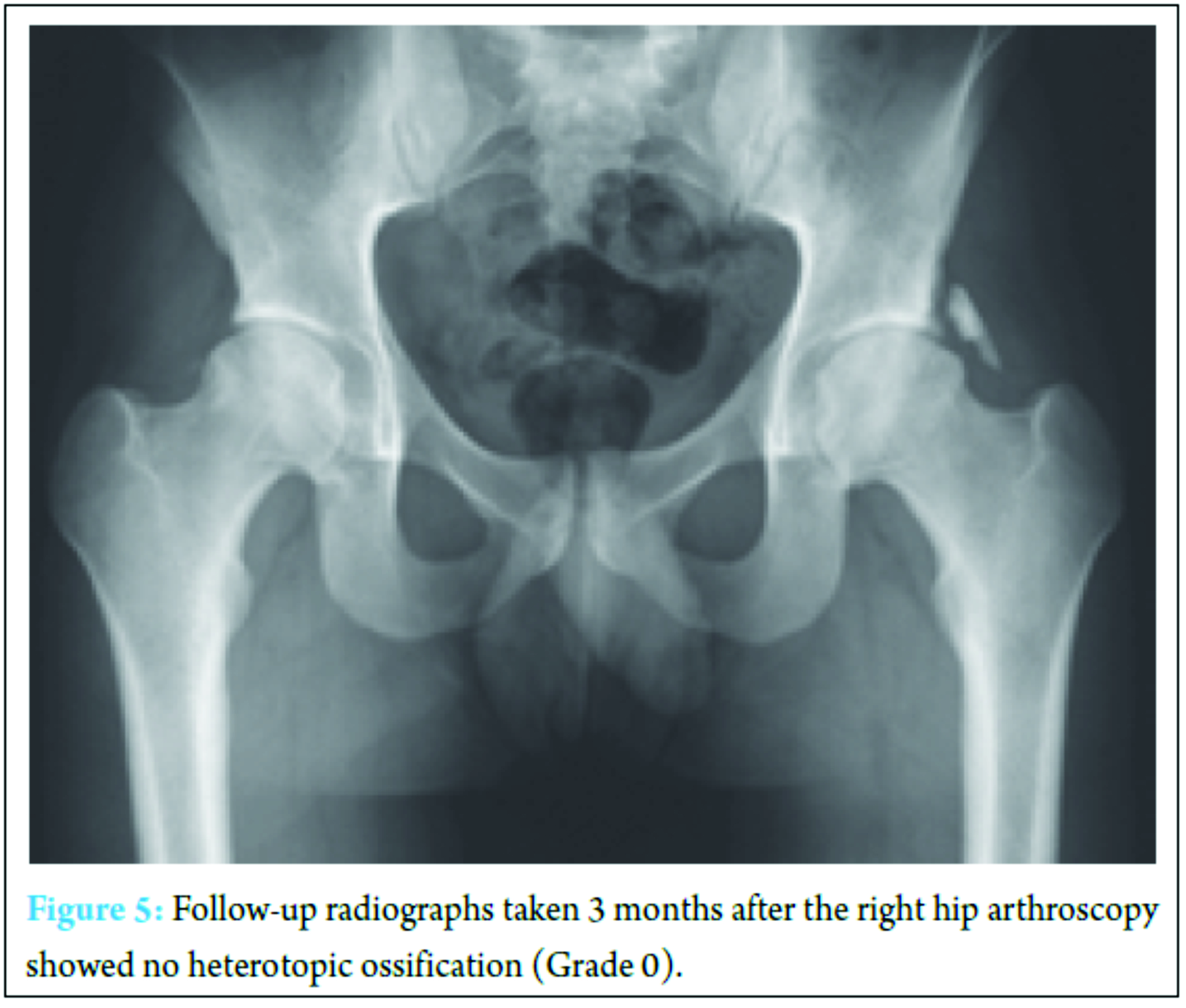
Before the right hip arthroscopy, the patient presented with a modified Harris Hip Score (mHHS) of 95.7, furthermore, he presented with an SF-12 score of 52 Physical Component Score (PCS) and 39 Mental Component Score (MCS). He described his “General Activity Level” to be 90% of normal. An 18-month postoperatively, the patient reported an mHHS of 100. His SF-12 scores improved to 56 (PCS) and 57 (MCS). His “General Activity Level” was increased to 100% postoperatively and he returned to play basketball professionally.
Discussion
Despite widespread literature regarding HO in open hip surgery, few studies have documented the prevalence of this complication in hip arthroscopy. In the few existing studies, the incidence of HO after hip arthroscopy varies widely between 0% and 44% [3, 4, 6, 7, 8]. A minimum of 9 weeks post-operative follow-up is recommended to assess the radiographic presence of HO [4]. The pathophysiology of HO is composed of three essential components: Inductive/inflammatory signaling pathways, inducible osteoprogenitor cells, and a heterotopic environment conducive to osteogenesis [7, 9]. Eliminating one of the essential components of HO is the key to its prevention. Therefore, therapy or prophylaxis aimed at disrupting the inductive/inflammatory signaling pathways, impairing the osteoprogenitor cells, or altering the conducive environment is paramount in disease management and prevention [9]. Non-steroidal anti-inflammatory drugs function by impeding the formation of inflammatory prostaglandins necessary for heterotopic bone formation. In addition, pre-operative radiation has been used to disrupt the cellular response after joint arthroplasty to successfully prevent HO [10, 12]. The prevention of the interaction between the damaged periosteum and necrotic cells may reduce heterotopic bone formation [13, 14]. This concept is further strengthened by Rath et al. [15] who showed that debridement of necrotic gluteus minimus reduced heterotopic bone formation after acetabular fracture fixation. Aho et al. [16] showed that isolating periosteum and damaged muscle may prevent the stimulation of ectopic bone formation. These examples indicate that altering the local environment may play a role in removing one of the essential components in HO formation. The described case report provides a rare opportunity to examine the process of HO in a controlled system. The clinical conditions described in the case were nearly identical (same patient, same surgeon, same arthroscopic technique and equipment, 1 year between surgeries, and same post-operative management) with the sole exception being 600 mg prophylactic Etodolac for 14-day postoperatively [5]. At the 3-month time point, while the patient was still undergoing physical therapy he described the improvement in his SF-12 scores, his “General Activity Level” score, as well as his mHHS. The patient’s presentation without HO (Grade 0), 3 months following prophylactic treatment, indicates a possible role for NSAIDs in post-operative prevention of HO, even in a case of previous development of HO. In this case, the presence of HO on the left hip was not associated with clinical manifestations of pain, discomfort, or limited hip motion. A more complete understanding of the etiology of HO and factors associated with its clinical expression will likely have therapeutic implications for patients undergoing hip arthroscopy.
Conclusion
HO is common after hip arthroscopy. A minimum of 9-week post-operative follow-up is recommended to assess the radiographic presence of HO. This case demonstrates the efficacy of HO prophylaxis in a single patient. Routine HO prophylaxis with NSAIDS should be considered for patients undergoing hip arthroscopy with osteoplasty.
Clinical Message
HO is common after hip arthroscopy. Routine HO prophylaxis with NSAID medications or other proven prophylactic measures should be considered for all patients undergoing hip arthroscopy.
References
1. Larson CM, Giveans MR. Arthroscopic management of femoroacetabular impingement: Early outcomes measures. Arthroscopy 2008;24(5):540-546.
2. Randelli F, Pierannunzii L, Banci L, Ragone V, Aliprandi A, Buly R. Heterotopic ossifications after arthroscopic management of femoroacetabular impingement: The role of NSAID prophylaxis. J Orthop Traumatol 2010;11(4):245-250.
3. Bedi A, Zbeda RM, Bueno VF, Downie B, Dolan M, Kelly BT. The incidence of heterotopic ossification after hip arthroscopy. Am J Sports Med 2012;40(4):854-863.
4. Rath E, Sherman H, Sampson TG, Ben Tov T, Maman E, Amar E. The incidence of heterotopic ossification in hip arthroscopy. Arthroscopy 2013;29(3):427-433.
5. Rath E, Warschawski Y, Maman E, Dolkart O, Sharfman ZT, Salai M, et al. Selective COX-2 inhibitors significantly reduce the occurrence of heterotopic ossification after hip arthroscopic surgery. Am J Sports Med 2016;44(3):677-681.
6. Ayers DC, Evarts CM, Parkinson JR. The prevention of heterotopic ossification in high-risk patients by low-dose radiation therapy after total hip arthroplasty. J Bone Joint Surg Am 1986;68(9):1423-1430.
7. Kaplan FS, Glaser DL, Hebela N, Shore EM. Heterotopic ossification. J Am Acad Orthop Surg 2004;12(2):116-125.
8. Schmidt SA, Kjaersgaard-Andersen P, Pedersen NW, Kristensen SS, Pedersen P, Nielsen JB. The use of indomethacin to prevent the formation of heterotopic bone after total hip replacement. A randomized, double-blind clinical trial. J Bone Joint Surg Am 1988;70(6):834-838.
9. Amar E, Sharfman ZT, Rath E. Heterotopic ossification after hip arthroscopy. J Hip Preserv Surg 2015;2(4):355-363.
10. Burd TA, Lowry KJ, Anglen JO. Indomethacin compared with localized irradiation for the prevention of heterotopic ossification following surgical treatment of acetabular fractures. J Bone Joint Surg Am 2001;83-A(12):1783-1788.
11. Amar E, Warschawski Y, Sampson TG, Atoun E, Steinberg EL, Rath E. Capsular closure does not affect development of heterotopic ossification after hip arthroscopy. Arthroscopy 2015;31(2):225-230.
12. D’Lima DD, Venn-Watson EJ, Tripuraneni P, Colwell CW. Indomethacin versus radiation therapy for heterotopic ossification after hip arthroplasty. Orthopedics 2001;24(12):1139-1143.
13. Zaccalini PS, Urist MR. Traumatic periosteal proliferations in rabbits. The enigma of experimental myositis ossification traumatica. J Trauma 1964;4:344-357.
14. Michelsson JE, Rauschning W. Pathogenesis of experimental heterotopic bone formation following temporary forcible exercising of immobilized limbs. Clin Orthop Relat Res 1983;176:265-272.
15. Rath EM, Russell GV Jr, Washington WJ, Routt ML Jr. Gluteus minimus necrotic muscle debridement diminishes heterotopic ossification after acetabular fracture fixation. Injury 2002;33(9):751-756.
16. Aho HJ, Aro H, Juntunen S, Strengell L, Michelsson JE. Bone formation in experimental myositis ossificans. Light and electron microscopy study. APMIS 1988;96(10):933-940.
| How to Cite This Article: Yaniv Warschawski, Zachary T. Sharfman, Eyal Amar, Ehud Rath. Anti-inflammatory Prophylaxis Prevents Heterotopic Ossification in Contralateral Side Hip Arthroscopy: A Case Report. Journal of Orthopaedic Case Reports 2017 Jan-Feb;7(1):20-23. Available from: https://www.jocr.co.in/wp/wp-content/uploads/9.-2250-0685.670.pdf |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com