[box type=”bio”] What to Learn from this Article?[/box]
A thorough history is critical to early diagnosis and treatment of complex regional pain syndrome in patients with unexplained pain, swelling, and decreased range of motion in the hand.
Case Report | Volume 7 | Issue 2 | JOCR March – April 2017 | Page 25-28| Christopher E Marrero, Neuyen Mclean, Keyana Varnado. DOI: 10.13107/jocr.2250-0685.734
Authors: Christopher E Marrero[1], Neuyen Mclean[1], Keyana Varnado[2]
[1] Department of Orthopaedic Surgery, Louisiana State University, New Orleans, Louisiana, USA.
[2] Louisiana State University School of Medicine, New Orleans, Louisiana, USA.
Address of Correspondence
Dr. Christopher E Marrero,
1542 Tulane Ave., Box T6-7 New Orleans, Louisiana 70112, USA. Phone: 504-568-4680.
E-mail: cmarre@lsuhsc.edu
Abstract
Introduction:
Complex regional pain syndrome (CRPS) is characterized by searing pain, hyperalgesia, edema, allodynia, and skin changes. CRPS may be difficult to diagnose and to treat given poorly understood mechanisms as well as its presentation of symptoms that may mimic common conditions such as joint stiffness in this condition as well as rheumatoid arthritis.
Case Report: A 71-year-old female presented to our clinic post shingles of the right upper extremity. We diagnosed her with CRPS based on the Budapest diagnostic criteria and the clinical findings of pain and decreased the range of motion along with edema, hypersensitivity, discoloration and allodynia of the right thumb and index finger. She was treated with vitamin C as well as gabapentin and physical therapy. The patient was unable to go consistently to physical therapy due to insurance limitations, and we found no clinical benefit of vitamin C in reducing her symptoms. She was lost to follow-up during her treatment but re-emerged at 21 months. At that time she reported, she was largely unchanged in regards to her right-hand symptoms but did believe the gabapentin was helpful and still continued to take 300 mg daily.
Conclusion: This case report highlights the usefulness of the Budapest diagnostic criteria to make the diagnosis of CRPS when associated with shingles, which can cause long-term pain and mimic some findings. Prompt diagnosis is important, as recovery typically extends beyond 6 months; our patient still reported continued symptoms at 21 months post initial presentation. Our primary treatment plan was physical therapy, which she discontinued due to insurance limitations. We recommend that patients, physicians, and third-party payers work together to extend access to physical therapy. More investigation is warranted regarding symptomatic treatment, as we found limited clinical benefit of gabapentin and vitamin C.
Keywords: Complex regional pain syndrome, shingles, herpes zoster virus, post-herpetic neuralgia.
Introduction
Complex regional pain syndrome (CRPS) is a clinical syndrome characterized by a constellation of findings including searing pain disproportionate to any inciting event, hyperalgesia, edema, allodynia, as well as sudomotor, vasomotor and skin changes [1]. CRPS is notoriously difficult to treat given the poorly understood mechanisms underlying the initiation of the syndrome, which is thought to be related to sustained sympathetic nervous system activation [1]. CRPS Type I is the most common and involves a limb without a direct nerve injury. CRPS Type II, previously referred to as causalgia, involves a defined nervous pathway and is associated with a direct nerve injury. In contrast, shingles, which is caused by the reactivation of the herpes zoster virus that typically lies dormant in the dorsal root ganglia of previously exposed individuals, affect a discrete dermatomal area with a classic vesicular rash and pain [2]. Post‑herpetic neuralgia is a frequent occurrence after shingles and is known to cause pain for long periods after the dermatomal rash has cleared. It usually involves the thoracic or abdominal dermatomes. Although CRPS associated with herpes zoster virus is well known clinically, there are relatively few published cases [2]. We add to the body of literature our clinical experience of this pathology affecting a 71-year-old female in the right upper extremity.
Case Report
A 71-year-old female presented as a new patient with a chief complaint of right thumb pain that had been present for 2 months before presentation. The patient reported that the onset of her pain began after an episode of shingles involving her right shoulder and her right hand. Since the shingles episode, the patient noted significant pain over the dorsum of the interphalangeal joint of the right thumb. On physical examination, she was found to have discoloration of the right thumb with decreased range of motion of the interphalangeal joint. There was no appreciable swelling. X-rays of her right hand were normal. Her limited range of motion was initially thought to be stiffness as a consequence of guarding the painful hand for an extended period. Consequently, she was prescribed 4 weeks of physical therapy for range of motion exercises. At her 1-month follow-up visit, she stated that the physical therapy slightly helped her range of motion but was not helpful in decreasing her right thumb pain. The right-hand exam demonstrated a decreased range of motion with mild diffuse swelling of the index finger and thumb. There was pain with range of motion of the interphalangeal joint of the thumb as well as hypersensitivity and allodynia over the dorsal ulnar aspect of this region. The patient was diagnosed with CRPS of the right-hand status post shingles of the right upper extremity. She was prescribed vitamin C 500 mg daily for 15 days and gabapentin at a dose of 300 mg 3 times per day. She was also advised to continue physical therapy for the range of motion and desensitization treatment. The patient was seen for follow-up 1 month later with only slight improvement of her pain despite our interventions and complained of periodic swelling of the right index finger and thumb. Her exam was unchanged and her right-hand X-ray demonstrated mild diffuse osteopenia (Fig. 1). She was instructed to continue the gabapentin and resume range of motion exercises at home, as she was financially unable to continue physical therapy.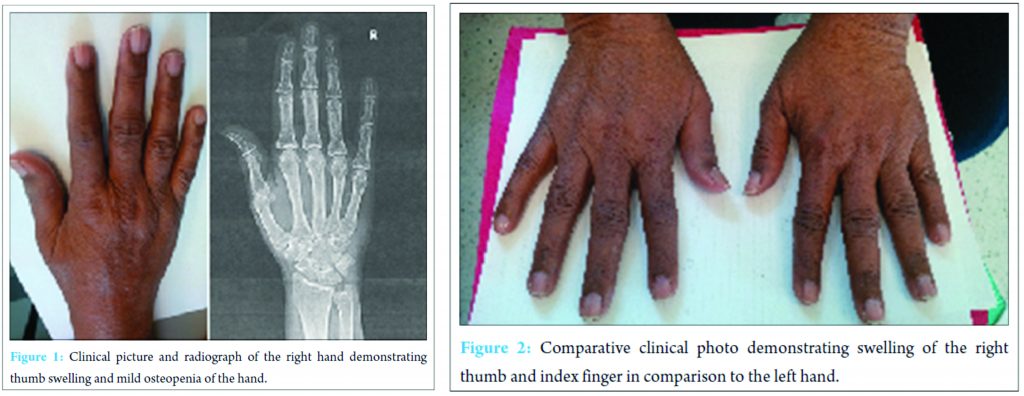
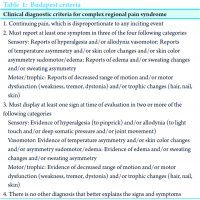
The patient returned for follow-up 3 months later stating that she was somewhat improved. She still complained of intermittent swelling of the right thumb and index finger. On physical exam, the tenderness over the right thumb was unchanged. However, the range of motion of the right thumb and index finger had increased. Gabapentin and range of motion exercises were continued. She was then lost to follow-up but did return 7 months later. At this point, she reported no improvement in pain of the right thumb or range of motion of right index finger and thumb. In the interim, she discontinued taking gabapentin because it was not helpful. The physical exam of the right hand was significant for trophic changes in the right index finger and thumb, with decreased range of motion and a significant decrease in skin wrinkling also noted (Fig. 2). She was again prescribed gabapentin and instructed to continue range of motion exercises at home. The patient was again lost to follow-up but was contacted by telephone approximately 21 months after the initial presentation. She stated that she felt unchanged with regard to hand swelling and pain but does believe the Neurontin is helpful and continues to take 300 mg 3 times per day.
Discussion
Our case presentation brings forth the question of whether the patient suffered CRPS triggered by the shingles outbreak or if this was simply a case of post-herpetic neuralgia with CRPS-like symptoms. A prospective randomized study by Berry et al. demonstrated that CRPS-like symptoms were found exclusively in patients whose herpetic rash extended into the affected extremity. Further, that study found that the more distal the herpetic rash on an extremity, the more severe and the longer the clinical course. In that series of 25 patients, no subject progressed to severe CRPS with the associated symptoms of sweating, hair and nail changes, severe dystonia or joint deformity [2]. In our patient, we noted similar signs and symptoms of pain, asymmetrical skin discoloration, edema, and decreased range of motion to the thumb and index finger. However, at no time did the patient demonstrate increased perspiration, hair and/or nail changes or joint deformity to the hand (Fig. 1 and 2) that could be associated with CRPS. This case also highlights the difficulty in making the clinical diagnosis. Other common conditions, such as rheumatoid arthritis and osteoarthritis, may also present with hand pain associated with decreased range of motion. In this case, we used the Budapest criteria to make the clinical diagnosis of CRPS (Table 1) [3]. The diagnosis may have been missed if not for using the diagnostic criteria. A delay in diagnosis would have led to a delay in treatment with possibly an even longer course of recovery for the patient. Our primary modality of treatment planned for this patient was to be an extended physical therapy regimen. There is evidence to suggest that this modality is helpful in decreasing the symptoms of CRPS [4, 5]. Physical therapy using graded motor imagery for an extended period up to 1 year may be required [4]. Our patient had a barrier to extended physical therapy due to insurance limitations. This is an ever increasing issue, and patients, as well as physicians, may need to work with third-party payers to extend access to physical therapy longer than a few visits over a few weeks.
Hand surgery with immobilization has been demonstrated as a trigger for CRPS [6]. Ascorbic acid (vitamin C) has been advocated as a means of decreasing the incidence of CRPS in hand surgery and has been shown to decrease the incidence of this in certain hand surgical procedures [7]. However, a recent randomized study of 336 patients with distal radius fractures demonstrated no benefit of the addition of vitamin C in preventing the occurrence of CRPS [8]. There is a lack of guidance in the literature regarding treating CRPS ex-post facto with vitamin C. We identified one case report of an adolescent female successfully treated with vitamin C and gabapentin after the development of CRPS. This, however, was in the lower extremity, and there was no clear indication as to which of the two agents, vitamin C or gabapentin, had the greater treating effect [9]. Our experience in treating CRPS after a shingles outbreak with vitamin C demonstrates little if any positive effect. Gabapentin was used as the primary agent to decrease symptoms in our patient. The agent was started relatively early in the patients course with a dosing of 300 mg 3 times a day. Gabapentin is a structural analog of gamma-aminobutyric acid. This molecule acts to inhibit large primary afferent nerve fibers presynapticly [10]. Gabapentin has demonstrated its efficacy in reducing neuropathic pain, as well as pain in post-herpetic neuralgia [11, 12]. We found limited clinical benefit in this patient’s case, as she gave mixed symptomatic response to the drug. This, however, may have been a dosing issue. While our patient remained on 300 mg/3 times a day, there are studies demonstrating successful use of gabapentin in CRPS from 900 to 3600 mg/day [13, 14]. Thus, it is unknown if an increased dosing regimen would have been more efficacious. Sympathetic blocks have also been demonstrated as helpful for symptomatic relief in CRPS. Although this treatment plan was not attempted in this patient, it may be a viable option [15]. To our knowledge and after a review of the literature, shingles in association with CRPS has not been demonstrated to be more resistant to treatment than CRPS from other causes. This is an area where more research is needed with regard to the course of the disease, residual symptoms, and long-term functional outcomes. In our clinical experience making the diagnosis of CRPS early along with early aggressive treatment is key to success in treating patients afflicted with CRPS. Treatment should always include therapy to maintain range of motion and for desensitization. Also in addition to pain medication, an anti-epileptic such as gabapentin should be considered to assist with symptoms.
Conclusion
In summary, the early clinical presentations of CRPS after a shingles outbreak may be missed without consideration to its presentation. We found the Budapest clinical diagnostic criteria helpful in making the diagnosis. It is uncertain if the disease process is a continuum of post-herpetic neuralgia or simply CRPS triggered by the herpes zoster virus. The clinical road to recovery should be detailed to the patient as typically extending well over 6 months. More investigation is needed in the realm of symptomatic treatment, as we observed little if no effect of gabapentin and vitamin C.
Clinical Message
The diagnosis of CRPS after a shingles outbreak may be missed due to similar findings in each entity. We found the Budapest clinical diagnostic criteria helpful in making the diagnosis of CRPS in this situation. Making the diagnosis and starting treatment early is important as CRPS may have a protracted course. Gabapentin was minimally effective while vitamin C demonstrated no clinical benefit.
References
1. Baron R, Levine JD, Fields HL. Causalgia and reflex sympathetic dystrophy: Does the sympathetic nervous system contribute to the generation of pain? Muscle Nerve 1999;22(6):678-695.1. Baron R, Levine JD, Fields HL. Causalgia and reflex sympathetic dystrophy: Does the sympathetic nervous system contribute to the generation of pain? Muscle Nerve 1999;22(6):678-695.
2. Berry JD, Rowbotham MC, Petersen KL. Complex regional pain syndrome-like symptoms during herpes zoster. Pain 2004;110(1-2):e1-e12.
3. Harden RN, Oaklander AL, Burton AW, Perez RS, Richardson K, Swan M, et al. Complex regional pain syndrome: Practical diagnostic and treatment guidelines, 4th edition. Pain Med 2013;14(2):180-229.
4. Oerlemans O, Oostendorp R, Boo T, van der Laan L, Severens J, Goris J. Adjuvant physical therapy versus occupational therapy in patients with reflex sympathetic dystrophy/complex regional pain syndrome Type I. Arch Phys Med Rehabil 2000;81:49-56.
5. Daly AE, Bialocerkowski AE. Does evidence support physiotherapy management of adult complex regional pain syndrome type one? A systematic review. Eur J Pain 2009;13(3):339-353.
6. Pepper A, Li W, Kingery WS, Angst MS, Curtin CM, Clark JD. Changes resembling complex regional pain syndrome following surgery and immobilization. J Pain 2013;14(5):516-524.
7. Zollinger PE, Kreis RW, van der Meulen HG, van der Elst M, Breederveld RS, Tuinebreijer WE. No higher risk of CRPS after external fixation of distal radial fractures – Subgroup analysis under randomised vitamin C prophylaxis. Open Orthop J 2010;4:71-75.
8. Ekrol I, Duckworth AD, Ralston SH, Court-Brown CM, McQueen MM. The influence of vitamin C on the outcome of distal radial fractures: A double-blind, randomized controlled trial. J Bone Joint Surg Am 2014;961(17):1451-1459.
9. Oliveira M, Manuela M, Cantinho G. Reflex sympathetic dystrophy. Acta Med Port 2011;24(6):1091-1096.
10. Rosenquist RW. Gabapentin. J Am Acad Orthop Surg 2002;10(3):153-156.
11. Kanodia SK, Seth AK, Dixit AM. Dose related efficacy of gabapentin in acute herpetic neuralgia among geriatric patients. Indian J Dermatol 2012;57(5):362-365.
12. Moore RA, Wiffen PJ, Derry S, McQuay HJ. Gabapentin for chronic neuropathic pain and fibromyalgia in adults. Cochrane Database Syst Rev 2011;3:CD007938.
13. Mellick GA, Mellicy LB, Mellick LB. Gabapentin in the management of reflex sympathetic dystrophy. J Pain Symptom Manage 1995;10(4):265-266.
14. Mellick GA, Mellick LB. Reflex sympathetic dystrophy treated with gabapentin. Arch Phys Med Rehabil 1997;78(1):98-105.
15. Toshniwal G, Sunder R, Thomas R, Dureja G. Management of complex regional pain syndrome type I in upper extremity evaluation of continuous stellate ganglion block and continuous infraclavicular brachial plexus block: A pilot study. Pain Med 2012;13(1):96-106.
 |
| Dr. Christopher E Marrero |
| How to Cite This Article: Marrero CE, Mclean N, Varnado K. Complex Regional Pain Syndrome following an Episode of Herpes Zoster: A Case Report. Journal of Orthopaedic Case Reports 2017 Mar-Apr;7(2):25-28 |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com




