[box type=”bio”] What to Learn from this Article?[/box]
Profunda femoris artery pseudoaneurysm is a rare but life-threatening complication after hip surgery. If there is a clinical suspicion, the surgeon should quickly actuate an adequate diagnostic-therapeutic pathway.
Case Report | Volume 7 | Issue 2 | JOCR March – April 2017 | Page 74-77| Nicola Piolanti, Michele Giuntoli, Anna Maria Nucci, Pietro Battistini, Michele Lisanti, Lorenzo Andreani. DOI: 10.13107/jocr.2250-0685.758
Authors: Nicola Piolanti[1], Michele Giuntoli[1], Anna Maria Nucci[1], Pietro Battistini[1], Michele Lisanti[1], Lorenzo Andreani[1]
[1] Department of Orthopaedics and Traumatology I, University of Pisa, 56126 Pisa, Italy.
Address of Correspondence:
Dr. Nicola Piolanti,
Department of Orthopaedics and Traumatology I, University of Pisa, 56126 Pisa, Italy.
E-mail: nicpio@hotmail.it
Abstract
Introduction: Vascular complications after femoral fixation are rare and not only easy to recognize but also potentially life-threatening. The aim of this case report is to describe how a pseudoaneurysm of the deep femoral artery can complicate an intramedullary nailing after a pertrochanteric fracture and how it can be treated.
Case Report: We report the case of a 90-year-old female who developed a pseudoaneurysm of the profunda femoris artery 16 days after intramedullary femoral nailing for a pertrochanteric hip fracture. Stenting of the artery was urgently performed with a consequent resolution of the symptoms.
Conclusion: Diagnosis of vascular complications after hip surgery may be very challenging because symptoms are often nonspecific. Despite their rarity, it is important to know this type of complications to address the diagnostic pathway in the right direction and to treat them promptly.
Keywords: Pertrochanteric fracture, femoral nailing, pseudoaneurysm, femoral artery, vascular injury.
Introduction
Fractures of the proximal femur tend to occur most often in the elderly and are more common in females. They can be divided into two principal groups: Intracapsular or medial fractures and extracapsular or lateral fractures. Pertrocantheric and subtrochanteric fractures represent the most frequent type accounting for nearly half of proximal femoral fractures. The surgical treatment of trochanteric femoral fractures includes extramedullary devices, intramedullary nailing, and arthroplasty. In the past years, intramedullary nailing has become more and more popular for the treatment of unstable (AO/OTA 31-A2.2, 31-A2.3, and 31-A3) and stable (AO/OTA 31-A1 and 31-A2.1) pertrochanteric fractures [1]. This surgical procedure presents several complications as malalignment, cutout, infection, false drilling, wrong lag screw length, and drill bit breakage during the interlocking procedure, external or internal malrotation (≥20°) of the femoral diaphysis, leg length discrepancy, impaired bone healing, fracture distal to the tip of the nail, fracture collapse, implant failure, lag screw intrapelvic migration, neurovascular injury, secondary varus deviation, complications after implant removal, trochanteric pain, and refracture [2]. Anyway, post-operative complications affect approximately 20% of patients with hip fracture, but only a few cases of vascular complications have been published [3]. Different types of vascular complications after hip fracture have been described in literature: Vessel laceration, hemorrhage, vascular compression, intimal flap tear, pseudoaneurysm, arteriovenous aneurysm, arterial thromboembolism, and ligation [4]. We report the case of a deep femoral artery pseudoaneurysm developed 16 days after femoral nailing and treated with arterial stenting.
Case Report
A 90-year-old female was admitted to our emergency department after falling on her left hip. On physical examination, the patient’s left leg was painful, shorter, and in external rotation. The patient was completely unable to bear any weight on it. A radiograph of her hips and pelvis showed a left multifragmentary pertrochanteric femoral fracture (31-A2 fracture, AO Classification) with dislocation of the lesser trochanter (Fig. 1).
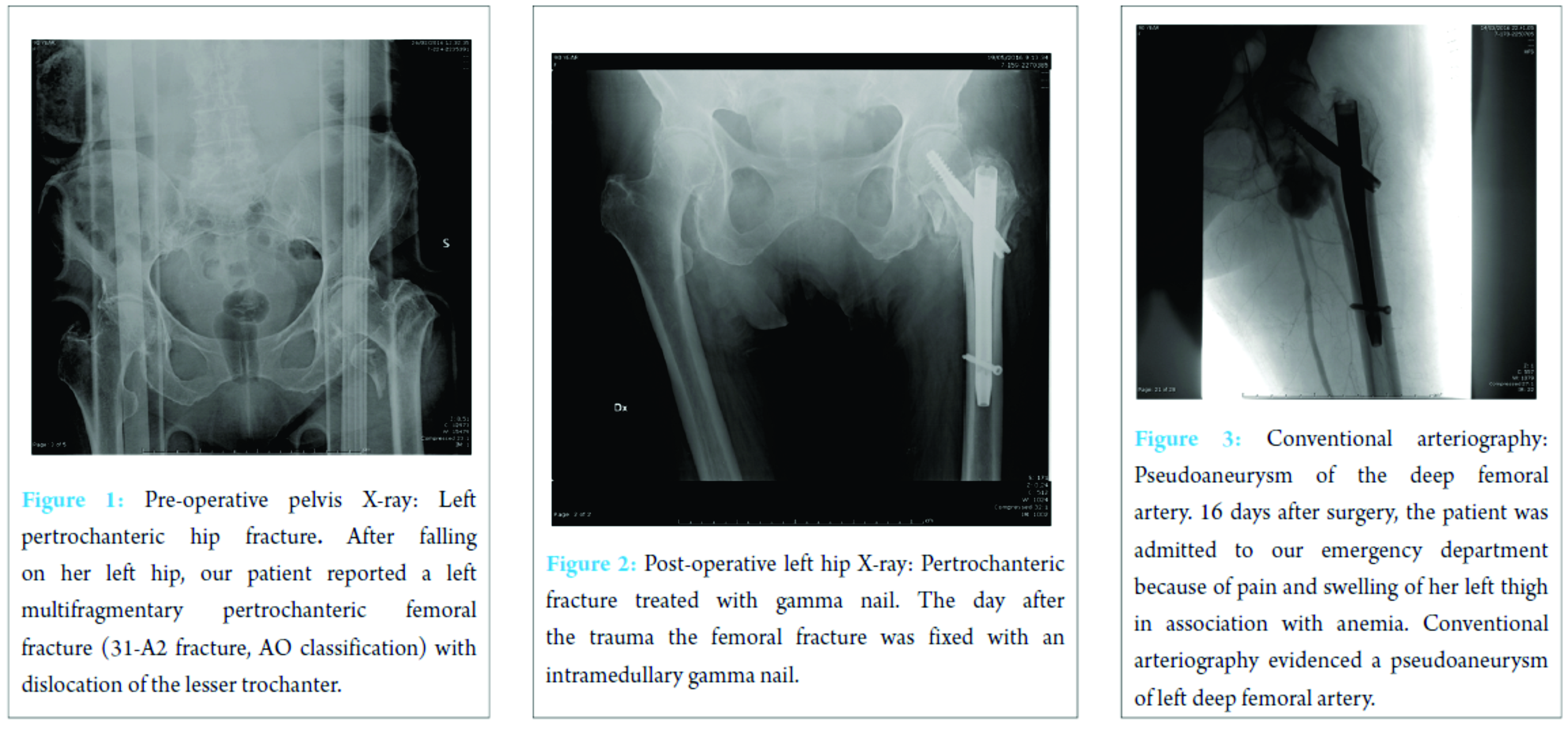
The day after, the fracture was fixed by means of an intramedullary nail without perioperative complications (Fig. 2). The post-operative course was regular apart from mild post-surgical anemia on the second post-operative day that was treated with two blood transfusions. On the 5th post-operative day, general conditions of the patient were good and the surgical wound had no signs of infection and no exudate, so she was discharged. 16 days after discharge, the patient made a new access to our emergency department for the appearance of severe anemia, pain, and swelling of her left hip. First of all, Doppler ultrasound was performed, and a large pseudoaneurysm of the proximal part of the profunda femoris artery was found. Her hemoglobin value was 7.7 g/dL, so she was urgently transfused. Then, left lower extremity arteriogram was performed and confirmed the diagnosis (Fig. 3).
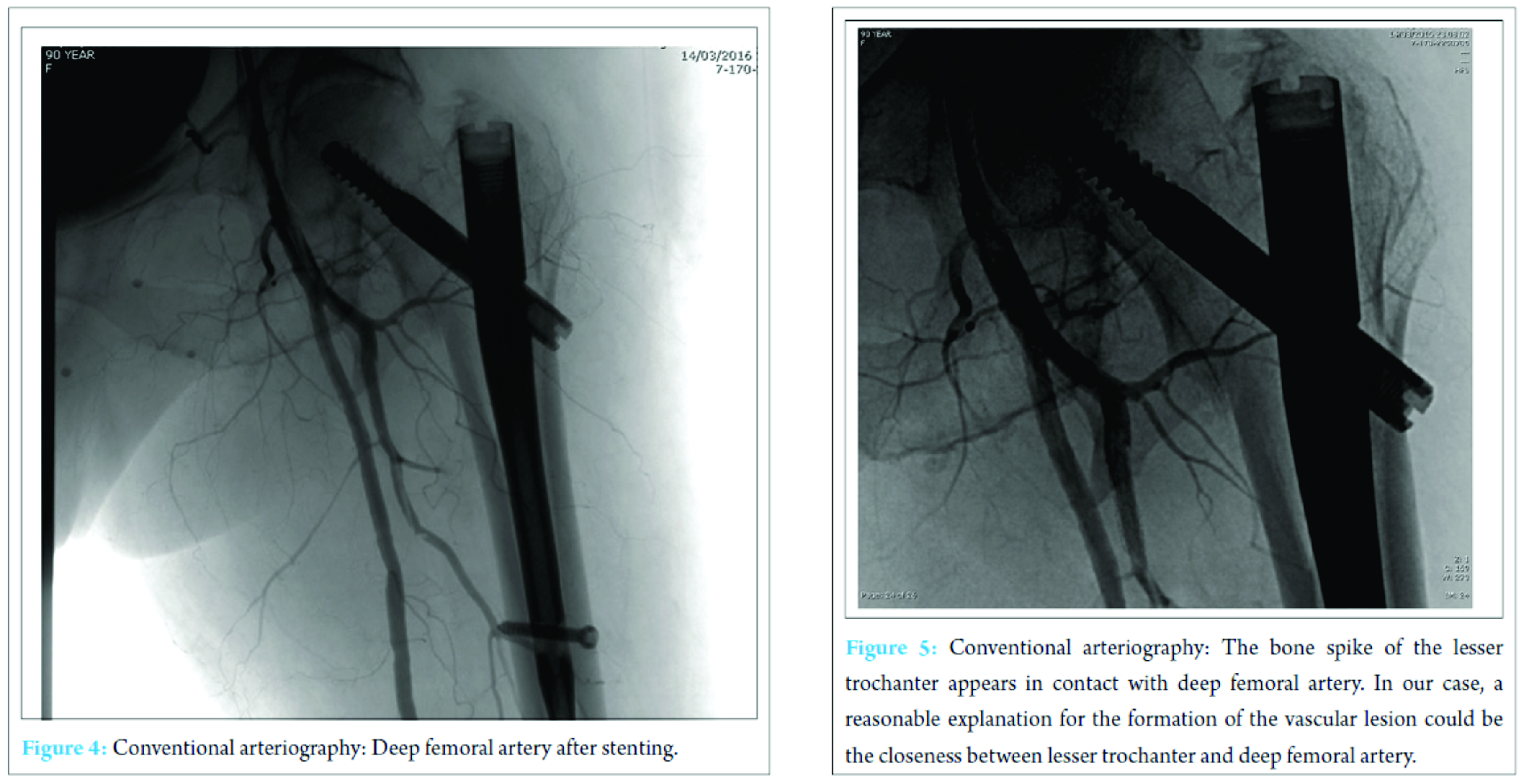
Therefore, a stent was placed (Fig. 4). After this procedure, the clinical conditions improved and the patient was discharged 4 days later with stable blood exams. On the last clinical control, 3 months after the stenting, the patient was feeling well and had started physical rehabilitation.
Discussion
Hip fractures in older patients are the most common fractures treated by orthopedic surgeons. The incidence increases with age and degree of osteoporosis. The most frequent traumatic mechanism is a low energy fall from a standing height [5]. Proximal femoral fractures may be treated using different techniques of fixation. Screws or partial arthroplasty proves to be efficient for the synthesis of intracapsular fractures, whereas nails and plates are the most commonly employed for extracapsular fractures. In our case, we treated a 31-A2 fracture with a gamma nail. The role of intramedullary fixation for the treatment of this kind of fracture is still debated. Anyway, gamma nail is often preferred to slide hip screws, especially, because of easy handling instrumentarium and implant versatility. According to many authors, gamma nail has proved to be a safe and efficient fixation of pertrochanteric fractures [6]. Vascular complications after intramedullary fixation of pertrochanteric fracture are rare. These complications can develop after fracture during intramedullary hip nailing and displacing of bone fragment during fracture or repair. Furthermore, some authors suggest that manipulation of atherosclerotic vessels of the leg on the fracture table may injure their brittle endothelium with an increased risk of bleeding and thromboembolic events. Vascular injuries may be hemorrhagic or thrombotic, acute (hemorrhage), or delayed (pseudoaneurysm formation). Regardless of the type of vascular lesion, the most frequently injured vessel is the deep femoral artery followed by its perforating branches [4]. False aneurysms or pseudoaneurysms are surrounded by a thin fibrous capsule in contrast to true aneurysms that consist of the true layers of the arterial wall. The fibrin capsule is made of soft tissues and/or hematoma adjacent the vessel. There is a high risk of enlargement and rapture of the vessel, in particular, when the dimension of the pseudoaneurysm is superior to 3 cm. Rapid expansion, infection, skin or soft tissue necrosis, neuropathy, distal ischemia, pain, or rupture are the most important indications for repair [7]. The incidence of pseudoaneurysm after hip fracture is very low (0.21% of incidence) and rarely reported as a consequence of dislocated bone fragments. According to literature, arterial damages can occur because of bone spikes, tip of the screws, drills, displaced implants, and retraction of surrounding tissue [8]. In our report, X-ray imaging after surgery shows the proximal migration of lesser trochanteric fragment, due to the action of iliopsoas that fits on the lesser trochanter, near the pseudoaneurysm. According to symptoms and instrumental studies, it seems that dislocated fragment may have damaged the deep femoral artery that lies near proximal femur (Fig. 5). However, in almost 25% of pertrochanteric fracture, the lesser trochanter was involved, but vascular complications rarely occur, probably thanks to vessels elasticity. Clinical manifestations of a false aneurysm after hip fracture have been reported between 3 days and 14 years, but in cases of dislocated lesser trochanter being responsible for vascular lesion, these manifestations are more frequent between 18 and 36 days. Probably clinical appearance of the pseudoaneurysm is delayed until the patient starts mobilization that can dislocate bone fragments. In this case, we found the pseudoaneurysm 16 days after surgery, below the average reported in literature. Often it is difficult to identify this complication because of non-specific symptoms including pain, edema, and swelling that are common after hip surgery. We should suspect a pseudoaneurysm if the patient presents falling of hemoglobin level, pulsatile swelling, or venous engorgement, and we can diagnose this complication by duplex ultrasound (US), conventional angiography, and computed tomography (CT) angiography [9]. US is the method of choice for diagnosis of pseudoaneurysm with sensitivity between 94 and 97%. As in our case, conventional angiography (or CT-angiography) can be useful to confirm and to better define the vascular lesion. There are numerous treatment options for deep femoral artery pseudoaneurysm: Conservative management for smaller aneurysms, US-guided compression, percutaneous US-guided thrombin injection, percutaneous US-guided collagen injection, insertion of coils, covered stents, and open surgery [10]. The treatment we chose consisted in positioning an endovascular stent covered by polytetrafluoroethylene. After the procedure, symptoms improved and the patient was able to resume the rehabilitation program a few days later.
Conclusion
Profunda femoris artery pseudoaneurysm is a rare vascular complication of surgical proximal femoral fractures. Facing this vascular lesion, the orthopedic surgeon should pay particular attention as it can involve severe consequences including death. The formation of a false aneurysm is often not promptly recognized because symptoms can develop many days after surgery and are not specific. Furthermore, the vascular lesion is not visible on plain radiograms. In case of acute anemia, pain and swelling of the fractured hip the appearance of a pseudoaneurysm should be considered, and the second level instrumental studies such as duplex US, conventional angiography, and CT angiography should be performed. It is clear that early diagnosis and adequate treatment can prove lifesaving in this type of complication.
Clinical Message
The formation of a pseudoaneurysm is a rare complication after hip surgery. Symptoms are often non-specific, and diagnosis can be very challenging. In case of acute anemia, pain, and swelling of the leg, this type of complication should be considered as a possible cause. To avoid severe consequences, an adequate diagnostic-therapeutic pathway should be promptly actuated.
References
1. Fracture and dislocation compendium. Orthopaedic Trauma Association Committee for Coding and Classification. J Orthop Trauma 1996;10 Suppl 1:v-ix, 1-154.1. Fracture and dislocation compendium. Orthopaedic Trauma Association Committee for Coding and Classification. J Orthop Trauma 1996;10 Suppl 1:v-ix, 1-154.
2. Mavrogenis AF, Panagopoulos GN, Megaloikonomos PD, Igoumenou VG, Galanopoulos I, Vottis CT, et al. Complications after hip nailing for fractures. Orthopedics 2016;39(1):e108-e116.
3. de Raaff CA, van Nieuwenhuizen RC, van Dorp TA. Pseudoaneurysm after pertrochanteric femur fracture: a case report. Skeletal Radiol 2016;45(4):575-578.
4. Barquet A, Gelink A, Giannoudis PV. Proximal femoral fractures and vascular injuries in adults: Incidence, aetiology and outcomes. Injury 2015;46(12):2297-2313.
5. Cumming RG, Nevitt MC, Cummings SR. Epidemiology of hip fractures. Epidemiol Rev 1997;19(2):244-257.
6. Georgiannos D, Lampridis V, Bisbinas I. Complications following treatment of trochanteric fractures with the gamma3 nail: Is the latest version of gamma nail superior to its predecessor? Surg Res Pract 2014;2014:3598.
7. Corriere MA, Guzman RJ. True and false aneurysms of the femoral artery. Semin Vasc Surg 2005;18(4):216-213.
8. Unay K, Poyanli O, Akan K, Poyanli A. Profunda femoris artery pseudoaneurysm after surgery and trauma. Strategies Trauma Limb Reconstr 2008;3(3):127-129.
9. Regus S, Lang W. Arterial injury and pseudoaneurysm formation after lesser trochanter fracture. Int J Surg Case Rep 2015;14:4-6.
10. Ahmad F, Turner SA, Torrie P, Gibson M. Iatrogenic femoral artery pseudoaneurysms – A review of current methods of diagnosis and treatment. Clin Radiol. R Coll Radiol 2008;63(12):1310-1316.
 |
 |
 |
 |
 |
 |
| Dr. Nicola Piolanti | Dr. Michele Giuntoli | Dr. Anna Maria Nucci | Dr. Pietro Battistini | Dr. Michele Lisanti | Dr. Lorenzo Andreani |
| How to Cite This Article: Piolanti N, Giuntoli M, Nucci AM, Battistini P, Lisanti M, Andreani L. Profunda Femoris Artery Pseudoaneurysm after Intramedullary Fixation for a Pertrochanteric Hip Fracture. Journal of Orthopaedic Case Reports 2017 Mar-Apr;7(2):74-77 |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com




